POLITECNICO DI MILANO
FACOLTÀ DI INGEGNERIA
Dipartimento di Bioingegneria
Corso di Laurea Magistrale in Ingegneria Biomedica
BREATHING PATTERN VARIABILITY IN PRETERM
INFANTS: THE EFFECT OF CAFFEINE WITHDRAWAL
Relatore:
Prof. Ing. Raffaele DELLACA’
Tesi di Laurea Specialistica di:
Marzia Liuni
Matr. n. 805749
Index
SUMMARY ... 1 INTRODUCTION ... 13 1.RESPIRATORY SYSTEM... 17 1.1 Physiology and Anatomy ... 1.2 Stages of lungs developments ... 1.3 Lung volumes ... 1.4 Modeling of respiratory system ... 2.PREMATURITY ... 33
2.1 Introduction ... 2.2 Breathing in preterm newborn ... 2.2.1 Apneas ... 2.2.2 Paradoxical movement ... 2.3 Management of neonatal failures ... 2.3.1 Pharmacologic therapy ... 2.3.2 Assisted ventilation ... 2.3.3 Special ventilation techniques: NAVA ... 3. ASSESSMENT OF BREATHING PATTERN ... 49 3.1 Techniques for monitoring breathing pattern ... 3.1.1 Direct measurements of volume ... 3.1.2 Indirect measurements of volume ... 3.1.3 Comparison between the different techniques ... 3.2 Methods to evaluate breathing pattern ... 3.2.1 Breathing pattern parameters ... 3.2.2 Variability analysis ... 4.THE SYSTEM ... 69
4.1 Limitations of the former system ... 4.2 Hardware ... 4.2.1 Material and framework ... 4.2.2 Webcams and pc ... 4.2.3 Marker ...
4.3 Software ... 4.3.1 Acquisition ... 4.3.2 Reconstruction of the signals ... 4.4 Analysis ... 4.4.1 Asynchronies ... 4.4.2 Variability ... 5.CLINICAL STUDY ... 97 5.1 Aim of the study ... 5.2 The study protocol ... 5.2.1 Studied population ... 5.2.2 Data and Statistical analysis ... 5.3 Results and discussion ... 5.4 Conclusions ... REFERENCES... 109
1
SUMMARY
Preterm newborns (less than 37 weeks of gestation) represent nearly the 9% of all infants.
They are low-weight and need assistance to breath, eat and fight infections. Many of their organs may be not completely developed (the most exposed are lungs, brain, intestine and retina), an immature respiratory system at various levels is common.
Lungs are one of the last organs to be developed; in premature infants being born at 23–27 respiratory bronchioles, alveolar ducts and primitive alveoli are starting to develop; epithelial cells are differentiating into type I and type II pneumocytes. Type II pneumocytes produce surfactant. Lastly, the alveolar duct arteries are giving rise to the alveolar capillaries.
At a structural level, in addition to an insufficient production of surfactant, an extremely elevated compliance of the chest wall (weak respiratory muscles, incomplete mineralization of the rib cage’s bones) exists. Moreover at the central level an undeveloped control system contributes to make respiratory disease of infancy one of the major complications in premature infants, with possible impact upon short and long-term respiratory morbidity.
Apnea of prematurity, defined by the American Academy of Pediatrics as a pause in breathing of greater than 20 seconds, or less than 20 seconds if accompanied by bradycardia and/or cyanosis are fairly common in preemies, moreover abnormal respiration phenomena like thoraco-abdominal asynchronies are frequent.
2 Chest wall asynchronism refers to the non-coincident motion of two compartments: pulmonary and abdominal ribcage or pulmonary ribcage and abdomen.
The procedure in these cases consists in assisted ventilation or pharmacologic therapies.
Methylxanthines: aminophylline, theophylline, and caffeine, have been used as respiratory stimulants in preterm infants for more than 30 years.
With their effect of competitive non-specific antagonist of adenosine receptors, methylxanthines work as CNS stimulants. Moreover caffeine acts as a central nervous system stimulant by increasing the medullary respiratory sensitivity to carbon dioxide.
It has been widely shown that caffeine citrate reduces the incidence of episodes of apnea and the rates of bronchopulmonary dysplasia, increases skeletal muscle tone and decreases diaphragmatic fatigue aiding respiratory effort. Caffeine citrate is frequently employed as prophylaxis in extubation from mechanical ventilation, moreover its administering was associated with a reduced incidence of cerebral palsy and cognitive delay when compared with placebo.
Stimulating central inspiratory drive, caffeine induces a significant increase in ventilation and in tidal volume (Vt) but while its action at the central level has
been object of many studies, the effect of caffeine on muscle strength performance has been less thoroughly examined. Findings have suggested direct effects on muscle excitation-contraction coupling and motor unit recruitment, reporting increase in electromyographic activity and enhanced muscle performance.
At date, discontinuation of drug therapy is largely empirical; a small percentage of patients may require home monitoring for apnea episodes upon hospital
3 discharge. Furthermore a clear indicator to establish the optimal dosage is absent.
It is considerable that some concerns have been expressed about possible adverse effects when used in the newborn period.
Many are the directions taken under considerations to understand how the analysis of the breathing pattern (BP) could lead to medical advances; it has been demonstrated that many parameters are significant to a deeper knowledge of some un-physiological respiration features and the effects of caffeine citrate treatment on them.
In particular, the study of variability of BP provides important information about the respiratory mechanism.
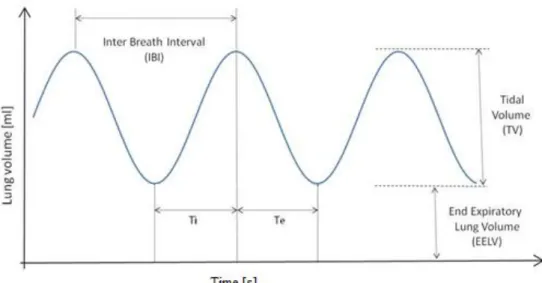
The interbreath interval (IBI) and Vt that together determine the minute
ventilation and therefore the amount of gas exchange show a correlation with the level of maturation of the respiratory control. [58, 59] Moreover, expiration lung volume (EELV) plays an important role in infants as it has to be actively elevated above the functional residual capacity (FRC) in order to avoid the alveolar collapse.
Chest wall asynchronies, a note respiratory dysfunction, when not subsisting with other severe pathologies (parenchymal processes, BDP, neuromuscolar disease...), are a useful indicator of respiratory muscle load and clinically assessed as a sign of increased work of breathing in patient with a structurally immature respiratory system.
Our aims were
-obtaining a reliable device able to monitor the previously mentioned parameters and possibly
4 -assessment of a correlation between their temporal properties and some pathological state or a certain response to caffeine citrate therapy.
More generally our purpose was to extract from the BP useful information for the management of the caffeine therapy and support of the clinical practice. Several techniques and devices for measuring lung tidal volume and flow have been considered; in order to permit studies of variability of BP they need to respond to some requisites like a sufficient spatial and temporal resolution, to allow registration long enough and to avoid the introduction of drift. Moreover to grant the detection of asynchronies meanwhile the respiration, techniques of indirect measurement of volume (through recording chest wall motion) would be preferable.
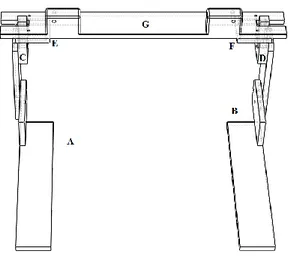
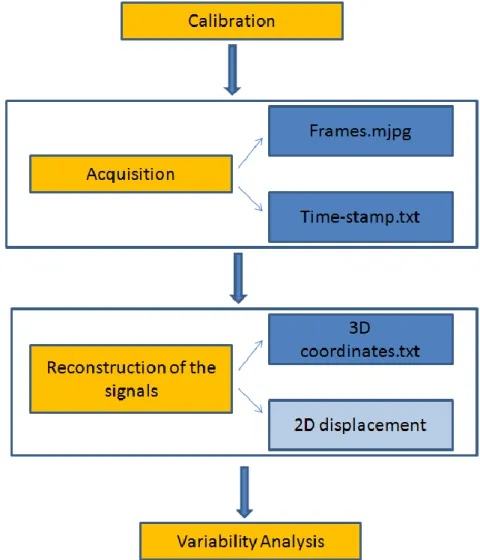
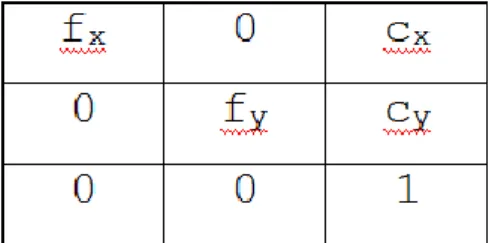
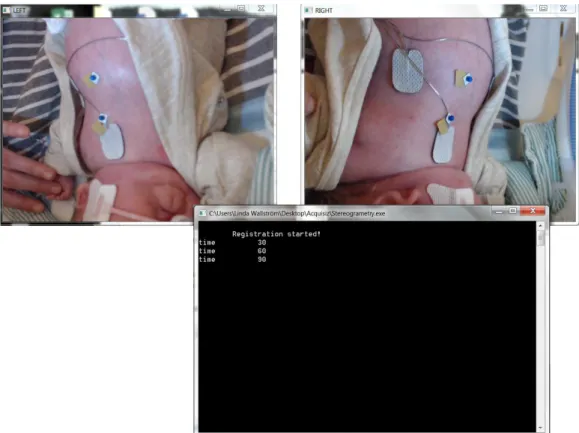
A new system responding to some of these requirements has been developed and validated at TBMlab (Politecnico di Milano). It shares the same idea behind the OEP but exploits two common webcams and works in the visible field instead of the infrared one. Once registered the displacement of one marker on the chest wall its trajectory is reconstructed with a stereophotogrammetry algorithm. In the end variability analysis are computed on the breathing pattern obtained. The system presents the same advantages of the OEP (precision, non-invasivity) and it is also inexpensive, portable and easy to use.
However by using this set up some observations have been done:
- tracking the displacement of a single point on the chest wall doesn't allow the assessment of the ribcage asynchronies
- some structural limits could be overcome for a major comfort meanwhile the measurements and better quality of the data acquired
5 - the usability of Linux, the operating system on which the application is enveloped, could appear tough to less expert users, moreover it makes the program non-transferable.
With our work, we have improved this former system with the aim to make it easier to use, granting more accurate measurements.
In the end we have explored one of its application fields employing the new system in the study of the effects of the caffeine citrate on the breathing pattern in preterm newborns.
The study was conducted on 10 subjects at NICU of Akademiska Sjukhuset hospital of Uppsala (Sweden) and at NICU of San Gerardo hospital of Monza, reporting their different response to the therapy.
Finally the detrended fluctuation analysis of IBI, Vt, EELV and asynchrony
indexes has been computed. Through the observation of the variability factor obtained: we have tried to establish whether the temporal properties of the BP are correlated to the instances where it is necessary to reintroduce the drug. If this correlation exists, the value may be used as an indicator of the optimal time of suspension of the drug or be prognostic of disease.
In conclusion, a reliable, cheap and easy to use device based on the same concept of the OEP and able to monitor the BP has been developed. With this work we have improved this former system and applied it in a study of variability of the BP in premature babies receiving caffeine citrate.
The results show different behaviors for each case, not allowing a general and unique trend. The limited size of the study sample does not allow any significant statement at this phase, as it could be investigating further with a larger number of measurements now that the system is validated, optimized and better known.
7
SOMMARIO
I nati pretermine (meno di 37 settimane di gestazione) costituiscono quasi il 9% della popolazione neonatale.
Caratterizzati da un basso peso, hanno bisogno di assistenza per respirare, nutrirsi e combattere le infezioni. Molti dei loro organi non sono completamente sviluppati (i più a rischio sono polmoni, cervello, intestino e retina), e spesso il loro apparato respiratorio deve ancora terminare lo sviluppo.
I polmoni sono fra gli ultimi organi a maturare; negli infanti prematuri nati fra la 23esima e la 27esima settimana di gestazione, i bronchioli, i dotti alveolari e gli alveoli primitivi stanno cominciando a svilupparsi; le cellule epiteliali stanno differenziandosi fra pneumociti di Tipo I e di Tipo II (che producono surfattanti) e i capillari alveolari si stanno formando.
A livello strutturale, oltre a un’insufficiente produzione di surfattanti, è presente un’estrema complianza della parete toracica (a causa di muscoli respiratori deboli e una cassa toracica non completamente mineralizzata). A questo si va ad aggiungere lo sviluppo non completo del sistema di controllo a livello centrale, col risultato di rendere le malattie respiratorie infantili una delle maggiori complicazioni nei nati prematuri, con possibili impatti sulla morbilità a breve e lungo termine.
Le apnee della prematurità, definite dalla American Academy of Pediatrics come una pausa nella respirazione di più di 20 secondi, o meno se accompagnate da bradicardia e cianosi, sono molto comuni nei prematuri. Sono inoltre frequenti fenomeni respiratori anormali come asincronie toracico-addominali.
8 Con “asicronia della parete toracica” si intende il movimento non simultaneo di due compartimenti: cassa toracica polmonare e addominale o, in alternativa, cassa toracica polmonare e addome.
In questi casi si procede con ventilazione assistita o terapie farmacologiche. Metilxantine: aminofilline, teofilline e caffeina sono usate da più di 30 anni come stimolanti respiratori nei bambini nati pretermine.
A causa del loro effetto antagonista competitivo non-specifico dei recettori per l’adenosina, le metilxantine agiscono come stimolanti del sistema nervoso centrale. Inoltre, la caffeina ha un’ulteriore effetto stimolante aumentando la sensibilità respiratoria della medulla all’anidride carbonica.
E’ stato ampiamente dimostrato che il citrato di caffeina riduce l’incidenza di episodi di apnea e la frequenza delle displasie broncopolmonari, aumenta il tono della muscolatura scheletrica e diminuisce l’affaticamento del diaframma aiutando la respirazione. Il citrato di caffeina è spesso impiegato come profilassi durante l’estubazione dalla ventilazione meccanica, e si è osservato che, rispetto a un placebo, il suo impiego in questa fase riduce l’incidenza di ritardi cognitivi e paresi cerebrali.
Attraverso la stimolazione dei centri che comandano l’inspirazione, la caffeina induce un aumento significativo della ventilazione e del Volume Corrente (Vt) .
Tuttavia, anche se l’azione della caffeina sul sistema centrale è stata ampiamente studiata, meno si è indagata la sua influenza sulle prestazioni muscolari.
Alcuni indizi suggeriscono un effetto diretto sulla muscolatura che comanda il meccanisco di eccitazione/contrazione e sul reclutamento delle unità motorie, mostrando un incremento dell’attività elettromiografica e delle prestazioni muscolari.
9 Al giorno d’oggi, la tempistica della terapia farmacologica è molto empirica. Una piccola percentuale di pazienti può richiedere un monitoraggio delle apnee anche dopo la dimissione dall’ospedale.
In aggiunta, un indicatore univoco e chiaro per stabilire il dosaggio ottimale è tuttora assente.
Sono stati sollevati inoltre dubbi su possibili effetti negativi sull’uso di una terapia del genere in età neonatale.
Lo studio del tracciato respiratorio (Breathing Pattern – BP), attualmente affrontato secondo diverse filosofie, può portare a progressi medici importanti in questo settore. È stato dimostrato che diversi parametri sono significativi allo scopo di una conoscenza più approfondita delle caratteristiche di una respirazione non fisiologica e degli effetti del trattamento con citrato di caffeina. In particolar modo, lo studio della variabilità del BP può fornire importanti informazioni riguardo il meccanismo respiratorio.
L’intervallo fra un respiro e il successivo, l’Interbreath Interval (IBI) e il Vt
determinano la ventilazione al minuto e conseguentemente lo scambio di gas, e sono collegati direttamente alla maturità del controllo respiratorio [58,59]. Inoltre, il volume espiratorio (EELV - expiration lung volume) ha un ruolo importante negli infanti e va mantenuto al di sopra della capacità funzionale residua (FRC) per evitare il collasso degli alveoli.
Le asincronie della parete toracica, una disfunzione respiratoria ben nota, quando non compresenti altre patologie gravi (processi parenchimatici, BDP, malattie neuromuscolari) sono un buon indicatore del carico muscolare respiratorio ed è clinicamente dimostrata come un segnale di fatica respiratoria aumentata in un paziente con un sistema respiratorio strutturalmente immaturo.
10 Gli obiettivi di questo lavoro sono:
Ottenere un dispositivo affidabile capace di monitorare i parametri di cui sopra.
Trovare una correlazione fra le proprietà temporali di questi parametri e alcuni stati patologici o la terapia con citrato di caffeina.
Più in generale, il nostro scopo è di estrarre dal BP informazioni utili alla gestione della terapia con caffeina e al supporto della pratica clinica.
Sono state considerate molte teniche e apparecchiature per misurare il volume corrente polmonare e i flussi respiratori; condizione necessaria per lo studio della variabilità del BP è che queste tecniche e apparecchiature abbiano una risoluzione spaziale e temporale sufficiente, che registrino sufficientemente a lungo e evitare l’introduzione di un drift. Inoltre, per garantire il rilevamento delle asincronie durante la respirazione, sono preferibili tecniche indirette di misurazione del volume (attraverso la registrazione del movimento del torace). Il TBMlab del Politecnico di Milano ha sviluppato e validato un nuovo sistema che risponde alla maggior parte di queste richieste.
Il concetto basilare è simile all’OEP ma fa uso di due webcam e acquisisce nel campo del visibile invece che nell’infrarosso.
Una volta registrato lo spostamento di un marker posto sulla parete toracica, si riscostruisce la sua traiettoria con un algoritmo stereofotogrammetrico. Il Breathing Pattern ottenuto è utilizzato per le analisi di variabilità.
Il sistema presenta alcuni vantaggi in comune con l’OEP (non invasivo, preciso) ed è inoltre poco costoso, portatile e di facile utilizzo.
11
La tracciatura di un singolo marker sul torace non permette il rilevamento di asincronie.
Ci sono alcuni limiti strutturali da superare per migliorare il confort del paziente durante la misurazione e aumentare la qualità dei dati acquisiti.
L’utilizzo di Linux, il sistema operativo su cui è stato sviluppata l’interfaccia informatica con il sistema, può essere complesso per utenti non esperti e inoltre rende il programma non trasferibile.
Con questo lavoro, abbiamo migliorato il sistema, rendendolo d’uso più facile e aumentando l’accuratezza delle misurazioni.
Al termine del lavoro abbiamo esplorato uno dei possibili campi di utilizzo del sistema, ovvero lo studio degli effetti del citrato di caffeina sul BP dei nati pretermine.
Lo Studio è stato condotto su 10 soggetti presso il NICU dell’ospedale Akademiska Sjukhuset di Uppsala (Svezia), e il NICU dell’Ospedale San Gerardo di Monza, riportando eventuali risposte differenti alla terapia.
Per concludere, è stata condotta la Detrended Fluctuation Analysis di IBI, Vt,
EELV e degli indici di asincronia.
Dall’osservazione dei fattori di variabilità ottenuti: α, abbiamo provato a stabilire se le proprietà temporali del BP sono legate ai casi in cui è necessario reintrodurre la terapia. Se è presente una correlazione, il valore di α può essere impiegato come indicatore del tempo di sospensione ottimale del farmaco o essere indicatore di una malattia.
È stato sviluppato un dispositivo affidabile, economico e facile da usare, basato sullo stesso concetto dell’OEP, in grado di monitorare il BP. Con questo Studio abbiamo ottimizzato questo sistema pre-esistente e lo abbiamo applicato in uno studio di variabilità del BP in neonati prematuri sotto terapia di caffeina citrato.
12 I risultati non mostrano un trend univoco. In questa fase pilota, la dimensione del campione non permette nessun affermazione significativa come si potrà ottenere in seguito aumentando la numerosità del campione essendo il sistema ora validato, ottimizzato e meglio conosciuto.
13
INTRODUCTION
Preterm newborns (less than 37 weeks of gestation) represent nearly the 9% of all infants.
They are low-weight and need assistance to breath, eat and fight infections. Many of their organs may be too immature for life outside the mother's uterus; the most exposed are lungs, brain, intestine and retina.
Lungs are one of the last organs to be developed thus lung disease of infancy remains one of the major complications in premature infants, with possible impact upon short- and long-term respiratory morbidity. The respiration system could be immature at the structural level with less alveoli, weak respiratory muscles and incomplete mineralization of the rib cage’s bones and at the central level with an undeveloped control system.
Their lungs are often characterized by an insufficient production of surfactant and an extremely elevated compliance of the chest wall. All this leads inevitably to a not physiological breathing pattern; apnea of prematurity is fairly common in preemies, moreover abnormal respiration phenomena like paradoxical movement are frequent. The procedure in these cases consists in assisted ventilation or pharmacologic therapies.
Methylxanthines: aminophylline, theophylline, and caffeine, have been used as respiratory stimulants in preterm infants for more than 30 years. It has been widely shown that caffeine citrate reduces the incidence of episodes of apnea and the rates of bronchopulmonary dysplasia, increases skeletal muscle tone and decreases diaphragmatic fatigue aiding respiratory effort. Caffeine citrate is frequently employed as prophylaxis in extubation from mechanical ventilation; moreover, its administering
14 was associated with a reduced incidence of cerebral palsy and cognitive delay when compared with placebo.
At date, discontinuation of drug therapy is largely empirical; a small percentage of patients may require home monitoring for apnea episodes upon hospital discharge. Furthermore a clear indicator to establish the optimal dosage is absent.
It is considerable that some concerns have been expressed about possible adverse effects when used in the newborn period.
Many are the directions taken under considerations to understand how the analysis of the breathing pattern (BP) could lead to medical advances.
With the aim to identify reliable and useful indicators for therapy and diagnosis it has been demonstrated that many parameters obtained from the analysis of the BP are significant to a deeper knowledge of some un-physiological respiration features and the effects of caffeine citrate treatment on the BP.
In particular, the study of variability of BP provides important information about the respiratory mechanism.
The interbreath interval (IBI) and TV that together determine the minute ventilation and therefore the amount of gas exchange show a correlation with the level of maturation of the respiratory control. [58, 59] Moreover, expiration lung volume (EELV) play an important role in infants as it has to be actively elevated above the functional residual capacity (FRC) in order to avoid the alveolar collapse.
Chest wall asynchronies, a note respiratory dysfunction, when not subsisting with other severe pathologies (parenchymal processes, BDP, neuromuscolar disease...), are a useful indicator of respiratory muscle load and clinically assessed as a sign of increased work of breathing in patient with a structurally immature respiratory system.
15 Several techniques and devices has been developed for measuring lung tidal volume and flow; in order to permit studies of variability of BP they need to respond to some requisites like a sufficient spatial and temporal resolution, to allow registration long enough and to avoid the introduction of drift. A new system responding to these requirements has been developed and validated at TBMlab (Politecnico di Milano). It shares the same idea behind the OEP but exploits two common webcams and works in the visible field instead of the infrared one. Ones registered the displacement of one marker on the chest wall its trajectory is reconstructed with a stereophotogrammetry algorithm. In the end variability analysis are computed on the breathing pattern obtained. The system presents the same advantages of the OEP (precision, non-invasivity) and it is also inexpensive, portable and easy to use.
However by using this set up some observations have been done:
- tracking the displacement of a single point on the chest wall doesn't allow the assessment of the ribcage asynchronies, common in preemies.
- some structural limits could be overcome for a major comfort meanwhile the measurements and better quality of the data acquired
- the usability of Linux, the operating system on which the application is enveloped, could appear tough to less expert users, moreover it makes the program non-transferable.
With our work, we have improved this former system with the aim to make it easier to use, granting more accurate measurements.
In the end we have explored one of its application field employing the new system in the study of the effects of the caffeine citrate on the breathing pattern in preterm newborns; a variability study of IBI, , EELV and asynchrony indexes has been computed with the purpose to extract useful information for the management of the caffeine therapy and support the decisions.
17
1.RESPIRATORY SYSTEM
1.1 Physiology and Anatomy
The respiratory system is a complex system consisting of specific structures for the exchange of oxygen and carbon dioxide between an organism and the environment. The passage of air into the lungs to supply the body with oxygen is called inhalation, the passage of air out of the lungs to expel carbon dioxide is called exhalation. The functional components which combine to bring about this process are:
- a neurological central controller which orders the respiratory muscles to contract or release
- the respiratory muscles; the most important of them is the diaphragm which allow the expansion and the reduction of the space into the thorax cavity.
- the airways (from the oral and nose cavity to the lungs) through which the air moves within the respiratory apparatus allowing the interchange of oxygen and carbon dioxide with the blood taking place.
- receptors sensitive to changes in the O2 and CO2 blood concentrations and stretch receptors located into the airways which stimulate the respiratory center.
18
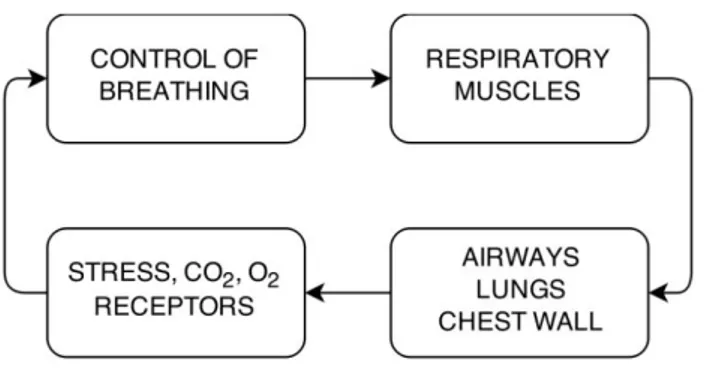
Figure 1 - Neurological central controller
Respiratory rhythm generation lies in the brainstem; the medulla oblongata contains numerous small nuclei of respiratory neurons. Each nucleus contains neurons that oscillate their discharge rate according not only to integral ionic ‘pacemaker’ currents analogous to those of cardiac cells, but also in response to both excitatory (e.g. glutamate) and inhibitory (e.g. g-aminobutyric acid (GABA), glycine) neurotransmitters released from nearby neurons.
Current opinion suggests that at least six types of neurons, each with characteristic firing patterns, form a complex network within the brainstem to produce a cycle of breathing. This medullary pattern generator is subject to influences from other areas of the central nervous system and from chemoreceptors and mechanoreceptors that make the system a feedback closed loop. [1]
The respiratory muscles
The respiratory muscles are morphologically and functionally skeletal muscles, their task is to displace the chest wall rhythmically to pump gas in and out of the lungs. They are the neck muscles, the intercostal muscles, the abdominal muscles and the diaphragm.
19 The neck muscles [6] include the sternocleidomastoid muscles and the scalenes. Their action is counteracting the action of the diaphragm on the upper ribcage. In normal subjects breathing at rest, however, these muscles are inactive, being recruited only when ventilation increases substantially, or when the inspiratory muscle pump is abnormally loaded.
The intercostal muscles [6] are two thin layers of muscle fibers occupying each of the intercostals spaces. When an intercostal muscle contracts in one interspace, it pulls the upper rib down and the lower rib up.
The wall of the abdomen is mainly made up of four abdominal muscles [6]: the rectus abdominis, the external and internal obliques and the transverses abdominis. These four muscles have two principal actions. First, as they contract, they pull the abdominal wall inward and produce an increase in abdominal pressure. This causes the diaphragm to move cranially into the thoracic cavity, and this motion, in turn, results in an increase in pleural pressure and a decrease in lung volume. Second, they pull the lower ribs caudally and deflate the cage.
The diaphragm is the dome-shaped sheet of muscle and tendon and it is the primary muscle used for respiration.
As the diaphragm contracts during inspiration its muscle fibers shorten, and the axial length of the apposed diaphragm diminishes so that the dome of the diaphragm descends relative to its costal insertions. The height of the zone of apposition, the portion of muscle directly apposed to the inner part of the lower ribcage, in normal subjects actually decreases by about 1.5 cm during quiet inspiration. In contrast, the dome of the diaphragm remains relatively constant in size and shape during breathing. This descent of the dome has two effects. First, it causes a fall of the pleural pressure. Hence, the thoracic cavity expands along
20 its cranio-caudal axis. Second, it produces a displacement of the abdominal visceral mass and an increase in abdominal pressure; this results in an outward motion of the ventral abdominal wall. In addition, because the muscle fibers of the costal diaphragm insert onto the upper margins of the lower six ribs, they apply a force on these ribs when they contract. The force has the effect of lifting the ribs and rotating them outward.
Lung and chest wall
The human lungs are a pair of large, spongy organs optimized for gas exchange between our blood and the air. Each lung is surrounded by the pleura; a double layered membrane between them, the so-called pleural cavity, creates a hollow space for the lungs to expand into during inhalation. Serous fluid secreted by the pleural membranes lubricates the inside of the pleural cavity to prevent irritation to the lungs during breathing.
Air enters the body through the nose or mouth and passes through the pharynx, larynx and trachea. Just before reaching the lungs, the trachea then splits into the left and right bronch: large, hollow tubes made of rigid hyaline cartilage that prevents the bronchi from collapsing and blocking airflow to the lungs. As the primary bronchi enter the lungs, they branch off into smaller secondary bronchi that carry air to each lobe of the lung. Thus, the right bronchus branches off into 3 secondary bronchi while the left lung branches off into 2 secondary bronchi. The secondary bronchi further branch into many smaller tertiary bronchi within each lobe. The secondary and tertiary bronchi improve the efficiency of the lungs by distributing air evenly within each lobe of the lungs.
The epithelium (pseudostratified) that lines the bronchi contains many cilia and goblet cells that secrete mucus to coat the lining of the bronchi. Particles of dust and even pathogens like viruses, bacteria and fungi in the air entering the lungs
21 stick to the mucus and are carried out of the respiratory tract. Cilia move together to push mucus secreted by the goblet cells away from the lungs. Many small bronchioles branch off from the tertiary bronchi. Bronchioles differ from bronchi both in size (they are smaller) and in the composition of their walls. While bronchi have hyaline cartilage rings in their walls, bronchioles are made of elastin fibers and smooth muscle tissue. The tissue of the bronchiole walls allows the diameter of bronchioles to change to a significant degree. When the body requires greater volumes of air entering the lungs, such as during exercise, the bronchioles dilate to permit greater airflow. The bronchioles further branch off into many tiny terminal bronchioles that terminate at the alveoli of the lungs. Alveoli are the functional units of the lungs that permit gas exchange between the air in the lungs and the blood in the capillaries of the lungs through diffusion. Each alveolus is an hollow, cup-shaped cavity surrounded by many tiny capillaries. Three major cell types (pneumocytes) compound its wall: type I with a structural function, type II that secrete surfactant, a surface-active lipoproteine that, lowering the surface tension of water,
- allows the membrane to separate, - increase pulmonary compliance
- prevent collapse of the lung at the end of expiration and type III that destroy foreign material, such as bacteria.
Chest wall is defined by all the anatomical structures surrounding the lung and moving with it. It can be thought of as consisting of two compartments: the ribcage and the abdomen, separated from each other by a thin musculotendinous structure, the diaphragm.
The abdomen contains the abdominal content and the abdominal wall (made up of abdominal muscles). When the diaphragm contracts during inspiration its descent usually results in an outward displacement of the ventral abdominal
22 wall; conversely, when the abdominal muscles contract, they generally cause an inward displacement of the belly wall, which results in a cranial motion of the diaphragm into the thoracic cavity [2, 6].
The ribcage is a complicated structure, consisting of a series of skeletal arches that are constituted by the thoracic vertebrae, the bony ribs, the costal cartilages and the sternum. These skeletal supports are connected by joints and ligaments. The attachment of the ribs to the sternum and spine in the first 7 ribs limits mobility of the structure in this area. There is a little mobility where the rib attaches to the cartilage before attaching to the sternum. Ribs 8-10 have longer costal cartilages which attach to other cartilage, so this area of the ribcage has more mobility. Ribs 11-12 have no anterior attachment at all so the greatest mobility of the structure is in this area. Due to these attachments, the upper ribs move differently from the lower ribs.
Expansion of the lungs can be accommodated by expansion of the ribcage compartment, the abdominal compartment, or both compartments simultaneously.
23
Figure 2
Receptors
Chemoreceptors and mechanoreceptors provide close loop feedback to the system; in particular the controller is influenced by stimuli received from:
- central chemoreceptors located in the medulla oblongata, which monitor the chemistry of cerebrospinal fluid and periferical chemoceptors located in the wall of the aortic arch and in the walls of the carotid arteries, which monitor the chemistry of the blood. The entrance of carbon dioxide (CO2) leads to the acidification of the liquid, for release
of ions. In response to the decrease in pH the chemoreceptors stimulate the respiratory center to increase the inspiratory rate.
- stretch receptors located in the walls of bronchi and bronchioles are activated when the lungs expand to their physical limits, signaling the respiratory center to interrupt stimulation of the inspiratory muscles and allow the beginning of expiration.
24
1.2 Stages of lungs developments
Human lung development can be subdivided into three chronological periods: an early embryonic period, until week 7 in which the formation of trachea and bronchial tree takes place, a fetal period and a postnatal period, during which lungs mature to an adult form.
The development process is well represented in the schematic below.
Figure 3
In premature infants being born at 23–27 the lung is at the canalicular stage of fetal lung development weeks gestational age.
At the canalicular stage, respiratory bronchioles, alveolar ducts and primitive alveoli are starting to develop; epithelial cells are differentiating into type I and type II pneumocytes. Type II pneumocytes produce surfactant. Lastly, the alveolar duct arteries are giving rise to the alveolar capillaries.
At 36 weeks of gestational age the “alveolar” phase begins and it will last for almost 3 years.
25 At the alveolar stage, terminal airways are differentiating into alveolar air sacs, microvasculature matures and the capillaries fuse. The epithelial cells flatten, with marked reduction in the alveoli-capillary diffusion barrier exchange unit which becomes 2 cells thick.
During the whole fetal period the mother's placenta helps the baby "breathing" while it is growing in the womb. Oxygen and carbon dioxide flow through the blood in the placenta. Most of it goes to the heart and flows through the baby's body. [7]
Despite the fetus doesn’t rely on ventilation to oxygenate tissues, he still breaths.
Indeed the mechanical forces generated by these intermittent thoracic movements seem necessary for normal growth and maturation of the fetal lung; their importance for development and maintenance of alveolar epithelial differentiation has been demonstrated. This “breathing” movements cause additional intermittent deformation of 5%, similar to postnatal breathing [14] that promotes alveolar epithelial type II cell differentiation.
At birth, although already functional, the lung is structurally still in an immature condition, because alveoli, the gas exchange units of the adult lung, are practically missing. The airspaces present are smooth-walled transitory ducts and saccules with primitive type septa that are thick and contain a double capillary network.
Right after the delivery the baby's lungs are filled with amniotic fluid. They are not inflated. The baby takes the first breath within about 10 seconds after the delivery. This breath sounds like a gasp, as the newborn's central nervous system reacts to the sudden change in temperature and environment. Once the baby takes the first breath, a number of changes occur in the infant's lungs and circulatory system:
26 - Increased oxygen in the lungs causes a decrease in blood flow resistance
to the lungs.
- Also blood flow resistance of the baby's blood vessels increases. - Amniotic fluid drains or it is absorbed from the respiratory system. The lungs inflate and begin working on their own, moving oxygen into the bloodstream and removing carbon dioxide by breathing out (exhalation).
After delivery, the breathing pattern has to progressively evolve from the periodic non-air-breathing pattern of the fetus to the continuous air-breathing pattern of the infant.
During the first 1-3 years of postnatal life, alveoli are formed through a septation process that greatly increases the gas exchange surface area. The primitive septa with their capillaries undergo a complete remodeling, gaining the mature slender morphology found in the adult lung [3, 4]
27
1.3 Lung volumes
Different lung volumes at rest can be defined associating them with different phases of respiratory cycle:
- The total lung capacity (TLC) is the volume in the respiratory system after as much air as possible has been inhaled.
- The gas volume exchanged during a breath is termed tidal volume ( ).
- The inspiratory reserve volume (IRV) is the maximum volume that can be inspired from an end-tidal inspiratory level.
- The sum of and IRV is defined as inspiratory capacity (IC).
- The volume of air breathed out after the deepest inhalation is defined
vital capacity (VC).
- Residual volume (RV) is the volume of air remaining in the lungs after a maximal exhalation.
- The volume remaining after a normal expiration is termed functional
residual capacity (FRC) or end-expiratory lung volume (EELV).
28
Figure 4
As explained before, the respiratory system is a closed loop, equipped with feed-forward and adaptive mechanisms (like change in chemoreceptor sensitivity) important for plasticity of the system.
This behavior paradigm provides a model framework to understand the control of breathing pattern for a breath. The traditional construct of respiratory physiology follows the principle of homeostasis: the idea that a regulatory mechanism, to maintain a given steady state, exists.
The ventilator pattern can be considered as an integrated output, which is influenced by changes in sensory inputs and behavioral demands on a breath-by-breath basis.
The ventilator control system is a complex system that manifests stochastic and deterministic variability, even in healthy subjects. Significant differences persist between infants, children and adults. In contrast to adults, infants actively maintain a level of end-expiratory lung volume (EELV) higher than the respiratory relaxation volume.
In infants, especially preterm ones, the expiration is not entirely passive, but it is active and complex. This cohort of patients is prone to lung collapse because of
29 an insufficient production of surfactant, the functional residual capacity of lungs close to airways closing volume and an extremely compliant chest wall with an immature respiratory center. The active control of EELV is due to active contraction of inspiration muscles during expiration, the closure of glottis and an increase in respiratory frequency. Changes in breathing pattern variability have been proposed as markers of the development of disease.
30
1.4 Modeling of respiratory system
The mechanical behavior of the respiratory system can be described by the following model:
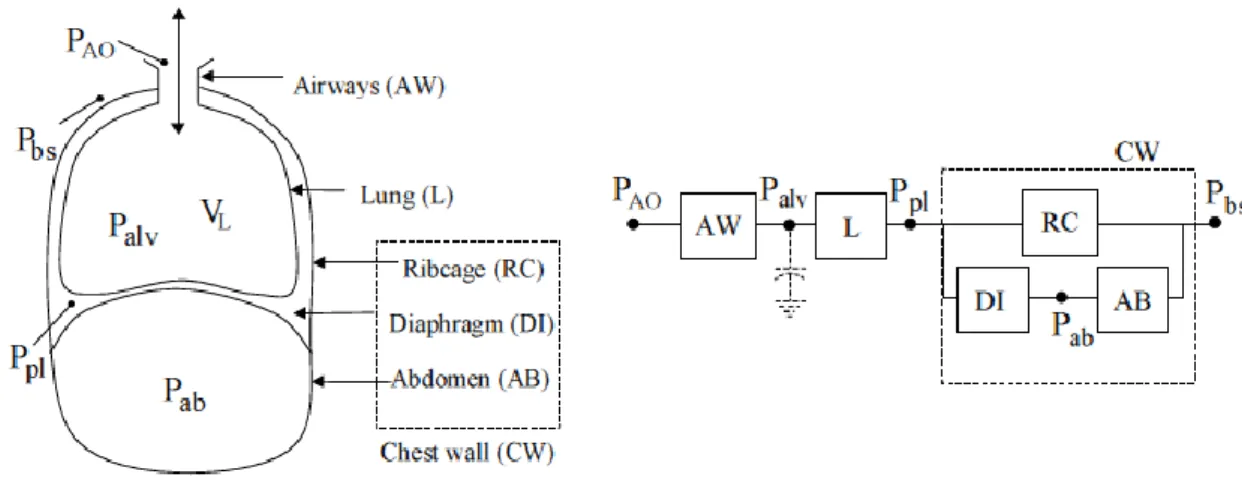
Figure 5
With PAC indicating the pressure at airway opening, Pbs pressure on body
surface, Ppl pleural pressure, Palv alveolar pressure, while V represents the
pulmonary airflow.
The block scheme models the respiratory system as made up of airways (AW), lungs (L) and chest wall (CW).
The blocks which constitute the model are furthermore characterized by resistive and elastic properties; the airways are well represented by a resistance while lungs and chest wall are resistance and compliance elements in series as depicted in Fig.6.
31
Figure 6
The total pressure on the respiratory system (P rs ), defined as the difference between the pressure at the mouth (P ao ) and the external pressure at the body surface (P bs ) is equal to:
Equation 1
However, the model described considers only one degree of freedom for the chest wall.
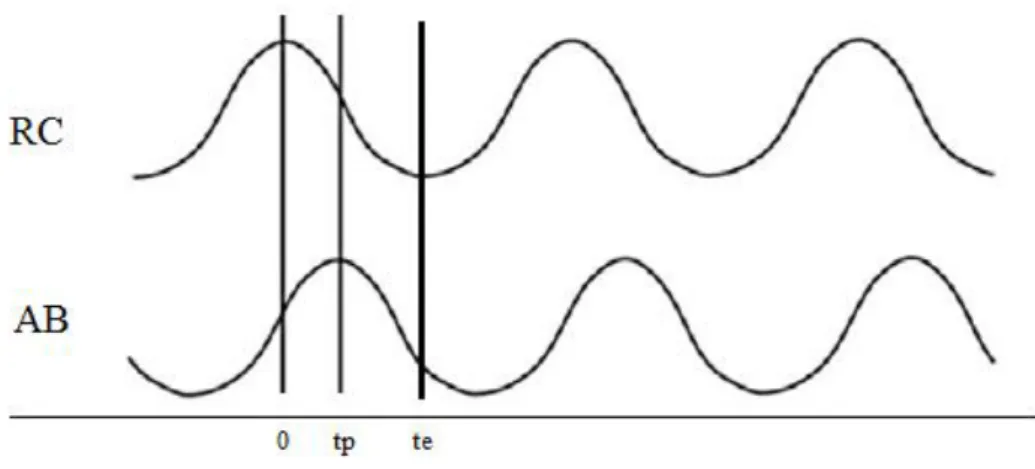
The first model of the chest wall was proposed by Konno and Mead [24]. Under the observation that the chest wall changes its volume and shape during breathing, they showed that, as a first approximation, the changes in shape could be accounted for by treating the chest wall as a system composted by two compartments, each with a single degree of freedom, the first being the ribcage (RC) and the second being the abdomen (AB). The two compartments may move independently from each other because they have one degree of freedom each (volume). However, when the airways are closed, the system has only a degree of freedom. Therefore the volume variations of the chest wall and abdomen are equal and opposite.
When considering the chest wall as composed by two compartments, as in the Konno and Mead model, the ribcage has been considered as a single compartment with a single degree of freedom. Available evidence suggests,
32 however, that such unitary behavior is the result of the highly coordinated action of the inspiratory muscles rather than inherent rigidity of the ribcage.
Figure 7 – Schematic of block model
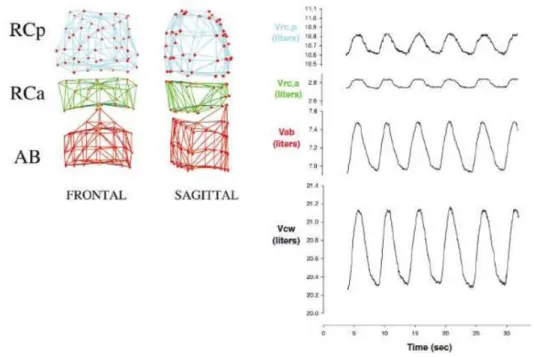
Ward et al proposed a more sophisticated model where the ribcage is divided into two compartments: the zone apposed to the lungs (pulmonary ribcage, RCp) and the zone apposed to the diaphragm (abdominal ribcage, RCa). This model, considering the diaphragm as divided into two components, the costal and the crural parts [13], makes it easy to understand how each compartment can move independently under the action of different groups of muscles.
Thanks to this it's possible to evaluate both the interaction between the ribcage and the abdomen (thoraco-abdominal asynchronies), and the interaction between the two ribcage’s compartments (ribcage distortion).
33
2.PREMATURITY
2.1 Introduction
A premature infant is a baby born before 37 completed weeks.
Health condition of the mother may contribute to preterm labor. Often, the cause of preterm labor is unknown.
About 15% of all premature births are multiple pregnancies.
Other factors that increase the risk for preterm labor and a premature delivery include:
Age of the mother (mothers who are younger than 16 or older than 35)
Being African-American
Lack of prenatal care
Low socioeconomic status
Use of tobacco, cocaine, or amphetamines
Common signs of prematurity include:
Abnormal breathing patterns (shallow, irregular pauses in breathing called apnea)
Difficulty in keeping a constant body temperature.
Low weight
Low muscle tone
Soft cartilages
Incomplete mineralization of the rib cage’s bones
Little body fat
Problems feeding due to trouble sucking or coordinating swallowing and breathing
34 After birth, the baby is admitted to a high-risk nursery. The infant is placed under a warmer or in a heated box called incubator. Monitoring machines track the baby's breathing, heart rate, and level of oxygen in the blood.
A premature infant's organs are not fully developed. The infant needs special care in a nursery until the organs have developed enough to keep the baby alive without medical support. This may take weeks to months.
35
2.2 Breathing in preterm newborn
Preterm respiratory failure has heterogeneous manifestations not only for the many pathologies that could be present at the birth with the symptoms of a respiratory distress but especially because the immaturity of the different components of the respiratory system lead to a complex framework the more severe the less is the gestational age.
Periodic breathing and thoraco-abdominal asynchronies are common symptoms of a not completely enveloped respiratory system; the resulting abnormal breathing pattern requires a treatment with the aim to grant an appropriate oxygenation and removal of CO2 of reducing the fatigue and the breathing work.
Pharmacologic intervention or, in most severe cases, ventilatory support are enacted.
2.2.1 Apneas
Periodic breathing is generally defined as groups of respiratory movements interrupted regularly by intervals of apnea
Apnea of prematurity, defined by the American Academy of Pediatrics as a pause in breathing of greater than 20 seconds, or less than 20 seconds if accompanied by bradycardia and/or cyanosis, is one of the most common respiratory problems in babies sheltered in neonatal intensive care units [65, 63]. If prolonged, apnea can lead to hypoxemia damaging the developing brain and other organs. Incidence of apnea of prematurity is directly related to gestational age, with apnea occurring in approximately 80% of neonates weighing less than 1000 g at birth [63, 66].
36 Advances in neonatal care in recent decades has resulted in an increased survival rate in low birth-weight premature neonates, and therefore the number of neonates with this disorder is increasing [63].
The manifestation of this phenomenon results from a number of influences (intrinsic and extrinsic) affecting the central respiratory network, peripheral and central chemoreceptors and mechanoreceptors, and ultimately leads to a reduction in output to the muscles of respiration.
The chest wall and soft tissues of the upper airway, both of which are quite compliant in premature infants, predispose to upper and lower airway collapse and obstruction.
Apnea is categorized as either central, obstructive or mixed.
Central apnea is the total cessation of inspiratory efforts with no evidence of obstruction.
Obstructive apnea is absence of airflow associated with respiratory movements against a closed larynx or pharynx.
Mixed apnea consists of obstructed respiratory efforts, usually following central pauses. During mixed apnea there is an initial loss of central respiratory drive during the central component, followed by a delayed recovery with activation of upper airway muscles superimposed upon a closed upper airway. In preterm infants, mixed apnea is the most frequent, typically accounting for 50% of long apneic episodes, followed by central apnea [71]. Purely obstructive spontaneous apnea in the absence of positional or fixed anatomical problems is uncommon in infants. While this classification of apnea implies different mechanisms, it is more likely all types are part of a continuum with the speculation that all apnea are a result of low central drive from the integrated respiratory network [51].
37 2.2.2 Paradoxical movement
In healthy subjects the contraction of the respiratory muscles is coordinated and the movement of the chest wall compartments is homogeneous. A note dysfunction of these muscles is the chest wall asynchronism; this refers to the non-coincident motion of two compartments: pulmonary and abdominal ribcage or pulmonary ribcage and abdomen.
Anatomical factors distinguishing the preterm from the full-term infant chest wall include: less ribcage ossification resulting in increased flexibility, less mature contractile activity of the intercostal and accessory muscles of respiration [20, 21]; thus reduce to an extremely compliant chest wall.
Meanwhile the inspiration, the lowering of the diaphragm isn't followed by the physiologic expansion of the chest wall anchored to a rigid structure of muscles and bones and it collapses instead.
During the expiration the rise of the diaphragm doesn't suffice to let the air flowing out because of the weakness of the chest wall.
The result is a non uniform movement of the upper compartment against the lower one.
The time lag between the two motions is able to guarantee ventilation, but in the worse cases may cause ventilation to be less effective or even totally ineffective; the highest degree of asynchrony occurs when one compartment moves in the opposite direction to the other. This is commonly referred to as paradoxical breathing movements.
The results of the study of Warren et all indicate a significant increase in the degree of ribcage and abdomen asynchrony in the preterm subjects compared to the full-term infants confirming the evaluation of the chest wall asynchronies as a significant indicator of the level of maturation of the respiratory system [64].
38 Moreover thoraco-abdominal asynchronies (TAA) are often observed in many respiratory disorders and/or respiratory muscle dysfunctions and clinically assessed as a sign of respiratory distress and increased work of breathing. They are a typical clinical sign of obstructive upper and lower airways disease in children. TAA can also be noticed in infants with parenchymal processes and with diaphragmatic weakness or diaphragmatic paralysis.
In conclusion, monitoring of thoraco-abdominal asynchronies is a useful, non-invasive indicator of respiratory muscle load or respiratory muscle dysfunction and can be used to determine response to therapy in individual patients.
39
2.3 Management of neonatal failures
While short respiratory pauses and respiratory dysrhythmias may be of minimal consequences if oxygenation is maintained, they can be problematic if accompanied by chronic intermittent hypoxemia.
Intermittent hypoxemia contributes to the immediate and long term co-morbidities. Therefore, this failure is treated with invasive and noninvasive respiratory supports and pharmacological therapies.
2.3.1 Pharmacologic therapy
Pharmacologic interventions include the treatment with methylxanthine class agents, which includes aminophylline, theophylline, and caffeine. This class of substances has been shown to reduce the frequency of apnea and the need for mechanical ventilation [19] and have been used as respiratory stimulants for premature neonates for more than 30 years and since 2005 caffeine was one of the 10 medications most frequently prescribed in neonatal intensive care units [5].
Of the methylxanthine agents, caffeine is the preferred agent because of its higher therapeutic ratio, longer half-life, and more reliable absorption when administered orally [63].
Currently, caffeine (C8H10N4O2) is the most widely consumed psychoactive
substance in the world. When caffeine is taken, it is completely absorbed and equally distributed throughout the total body water within forty-five minutes of assumption. There is a similarity between the molecular structures of caffeine and adenosine, a naturally occurring substance in the brain. This similarity allows caffeine to bind to the same receptor sites as adenosine. However, the binding of caffeine to an adenosine receptor site does not produce the same effect as binding of adenosine to the receptor. Thus, caffeine is classified as an
40 adenosine antagonist; a drug that attaches to a receptor and blocks the action of any other molecule trying to bind to the receptor site. One of the main functions of the adenosine is to maintain balance between energy intake and metabolic demand. Normally, adenosine inhibits the release of the neurotransmitter, dopamine, resulting in increased fatigue and lack of spontaneous behavioral activity.
Disrupting the interaction between adenosine and its receptor affects the production of neurotransmitters in the brain, like dopamine, serotonin, and epinephrine, which result in one’s ability to stay awake longer and have more energy.
Moreover caffeine acts as a central nervous system stimulant by increasing the medullary respiratory sensitivity to carbon dioxide.
In conclusion, stimulating central inspiratory drive, caffeine induces a significant increase in ventilation and in tidal volume ( ) [53, 54, 56].
While its action at the central level has been object of many studies, the effect of caffeine on muscle strength performance has been less thoroughly examined. Findings have suggested direct effects on muscle excitation-contraction coupling and motor unit recruitment, reporting increase in electromyographic activity and enhanced muscle performance.
The potential performance enhancing effects of caffeine have been explained by means of multiple mechanisms. These include changes in central nervous system transmission leading to blunted perception of exertion and pain.
Moreover, caffeine ingestion has been associated with increased motor unit activation; a proposed explanation has been that caffeine may positively enhance calcium release from the sarcoplasmic reticulum, resulting in increased
41 Caffeine treatment results in:
- a decrease of periodic breathing and hypoxic depression
- a rapid and sustained increase in minute ventilation, diaphragmatic activity and in preterm infants [53].
The standard dosage regimen for caffeine citrate is a 20 mg/kg loading dose followed by a maintenance dose of 5–10 mg/kg given daily.
Due to the hepatic metabolism and renal elimination of methylxanthines, studies have been conducted to assess the need for maturation-dependent dose modifications. Hepatic activity reaches adult values at 6 months of life, while renal clearance of caffeine differs significantly between preterm and full-term neonates, increasing with gaining weight and postnatal age and reaching adult values at 8-12 months of age. For these reasons, it is postulated that lower doses may be needed in preterm neonates compared with term neonates or children. However it has to be said that AOP typically resolves at 33-34 weeks postmenstrual age, and consequently the therapy is usually stopped in this period.
Although highly effective for the management of apnea of prematurity, caffeine has adverse effects in neonates, including tachycardia, vomiting, and feeding intolerance [63].
Furthermore there are some concerns that caffeine may result in neonatal brain injury and may also have an effect on childhood behaviour.
Despite a large amount of information on therapy for apnea of prematurity, there are minimal information on the response rate relative maintenance doses and
42 gestational age. The relationships between initial maintenance dose of caffeine citrate therapy and gestational age is still to be investigated as determining the safety of higher maintenance doses in the management of apnea of prematurity. Because apneic events were not consistently documented by the providers as a means of evaluating dose-related response to therapy, the number of clinical interventions needed (weight adjustment, mini-loading, or maintenance dose increases from initial) was utilized as a marker of efficacy. Sometimes it's even necessary to reintroduce the caffeine, after a former interruption of the therapy, for patients who show again apneic phenomena.
Nowadays a clear indicator to establish the optimal dose and the most suitable time of interruption of the therapy is still absent.
2.3.2 Assisted ventilation
Less than three decades ago, survival of extremely premature infants was rare. Smaller, more immature neonates do survive today, in part, because of improved mechanical ventilation.
Mechanical ventilators available since the mid-1960s used mandatory ventilation and they essentially function independently of the infant, delivering a mechanical breath at a present of interval, irrespective of his spontaneous ventilatory effort. It's therefore not surprising that infants often exhibit asynchronous breathing, during which their own spontaneous breaths are out of phase with the mechanically delivered breaths.
Asynchrony may result in several deleterious effects.
Advances in microprocessor technology and ventilator design have overcome the obstacles in detecting and responding to the spontaneous effort of even the
43 smallest preterm infants. Synchronized ventilatory modes are characterized by the delivery of a mechanical breath in response to a signal derived from the patient representing spontaneous respiratory effort.
There are many ways to detect the signal from the patient; the most common triggering variables are the flow and the pressure.
Flow triggered ventilation
The breath is triggered by variations of a baseline flow considered as a constant. These variations are monitored next to the expiratory valves or through flow sensors inside the patient's circuit. The ventilator measures the flow from both the ventilator and the patient. In a closed loop the two flows are the same if the patient's effort is absent. When the patient tries to inspire the difference between the expiratory and the inspiratory flow is measured.
When this value reaches an established threshold, the ventilator delivers a breath.
Pressure triggered
The inspiratory effort of the patient causes a pressure drop into the respiratory ways and inside the ventilation circuit. The inspiration is started when the pressure falls down a determined threshold. The site where the measurement is done affects the performances of the device; the most accurate location would be the trachea but the discomfort of an endotracheal tube with a measurement site lead to the choice of different solutions. Nowadays the sensor is located into the Y circuit or into the expiration/expiration doors.
Obviously, the further from the source of pressure or flow is the sensor, the bigger is the delay of the ventilator's response; the site of reveal of the patient's signal should be as near as possible to its origins.
44 The aim of the assisted mode at synchronizing the ventilator insufflation to the patient’s effort is both to optimize comfort and to minimize the work of breathing, but the price to pay for this strategy is a risk of patient–ventilator asynchrony, which can be defined as a mismatch between the patient’s neural output and the ventilator’s inspiratory and expiratory times [34, 37].
Recent evidences suggest that lung injury is partially dependent on the ventilatory strategies used. There is an emerging consensus that mechanical ventilation leads to lung injury
Thille and colleagues reported that one-quarter of patients had high rates of asynchrony during assisted ventilation [34].
Frequent asynchrony is associated with a longer duration of mechanical ventilator [34, 38].
Various ventilation strategies have been evaluated (enveloped) with the aim of reducing lung injury in neonates. Optimal ventilatory strategies should promote adequate gas exchange with minimum lung injury and other adverse effects. The new challenge in developing ventilation strategies thus consists of minimizing the risk of lung injury, avoiding disuse atrophy of the diaphragm, and improving the match between the patient’s needs and the assistance delivered by the ventilator [59]. New ventilation modes have been designed to meet this challenge [42, 55].
45 2.3.3 Special ventilation techniques: NAVA
The best approach to coordinate the patient and the ventilator would be that to use the neural signals from the respiratory centers; such a method is clearly impossible. The only clinical approach permitted consists of the measurement of the electric activity of the diaphragm; the most important inspiratory muscle. NAVA is an assist mode of mechanical ventilation that delivers a pressure proportional to the integral of the electrical activity of the diaphragm (EAdi), and therefore proportional to the neural output of the patient’s central respiratory command.
The level of pressure delivered is thus determined by the patient’s respiratory-center neural output. With NAVA, the ventilator is triggered and cycled-off based on the EAdi value, which directly reflects the activity of the neural respiratory command (see fig.8). The inspiratory airway pressure applied by the ventilator is determined by the following equation:
46
Figure 8
In NAVA, the pressure in the airway is modulated by the intensity of the inspiratory efforts of the patient and not predetermined by the clinician settings. As a result, the pressure, the inspiratory flow and the tidal volume varies from one cycle to another.
For this reason the fan curves present in NAVA have a more irregular aspect than ones observed in other ventilation modality.
About the benefits of NAVA compared to standard ventilation modes (SVM), a review of the literature highlights the following points. NAVA improves patient-ventilator synchronization against the SVM by reducing the trigger delay, decreasing the inspiratory time excess and reducing the total number of asynchrony compared to the others. NAVA also serves to remove inefficient
47 efforts, frequent source of increased work of breathing in ventilated patients [52, 9, 46].
In NAVA, greater variability in tidal volume than SVM is observed [9, 58] which probably results in a more "physiological" ventilation or at least better respecting the patient's inspiratory demand. Several studies show that, compared to the SVM, NAVA ensures adequate ventilation while maintaining average airway pressure and lower tidal volumes, thus avoiding [52, 47, 26, 27, 46] adverse effects of overassistance.
48 THIS PAGE IS INTENTIONALLY LEFT BLANK
49
3. ASSESSMENT OF BREATHING
PATTERN
3.1 Techniques for monitoring breathing pattern
Techniques used to obtain tidal breathing data can be divided in direct and indirect assessments of breathing.
3.1.1 Direct measurements of volume
Direct measurements are obtained using a sensor (flow meter) placed at or near the airways opening. They allow acquisition of breath-to-breath tidal volume, thanks to integration of the flow signal.
3.1.1.1 Pneumotachograph (PNT)
The pneumotachograph is a flow sensor with a flow-resistive element, characterized by flow-pressure relation approximately linear. It is connected in series to a silicon mask encompassing the infant’s nose, with or without the mouth. Minimization of technical dead space is crucial because the increase of CO2, due to dead space, may alter the control of breathing and affect the tidal flow waveform [47]
3.1.1.2 Ultrasonic flow meter
This sensor, recently commercially available for clinical uses, measures the average velocity of a fluid along the path of an emitted beam of ultrasound. Frey et al suggest this sensor to measure lung volume (FRC) and ventilation distribution in spontaneously breathing infants because flow and gas
50 concentration can be measured simultaneously and the adjustment of the delay time between flow and tracer gas signal is not necessary. Moreover they reported that the breathing pattern was unaffected by the measurement technique [32]. These sensors are quite expensive compared to the others.
3.1.1.3 Hot wire anemometer
The operating principle of this sensor is the proportional relation between the heat transfer, between a heated element and a moving gas, and the speed of the gas. The heat lost to the gas is used to measure flow. This transducer has high sensitivity at low flow and vice versa, hence it has a wide dynamic range, other advantages are small size and good frequency response. Disadvantages include nonlinearity, dependence on temperature and other gas properties, presence of a small technical dead space and they are not sensitive to flow direction [40]
3.1.2 Indirect measurements of volume
Indirect techniques, instead of measuring respiratory flow or pressure at the airway, characterize the activity of associated tissues, i.e. chest wall, abdominal wall and esophageal pressure.
This other kind of techniques allows, through recording chest wall motion, the detection and assessment of asynchronies meanwhile the respiration.
3.1.2.1 Respiratory inductance plethysmography (RIP)
The Respiratory Inductive Plethysmography (RIP) consists of two loops of wire which are coiled and sewed into (compliant) elastic belts. It measures changes in cross-sectional areas.
A low alternating current at a frequency of usually 300 kHz is passed through the belt generating a magnetic field normal to the orientation of the belt.
51 Respiratory movements change the cross-sectional area of the compartment and cause changes in the electrical self-inductance of the coils. This signal is demodulated and amplified such that waveforms of the ribcage excursions are converted to analogue voltage changes and can be digitally processed [31]. The following image depicts a schematic of RIP-
Figure 9
RIP requires calibration in order to convert the voltage output to units to volume.
The calibration coefficients are obtained experimentally by special isovolume maneuvers at different lung volumes on each subject combined with spirometric measurement. Calibration procedures in patients who are unable to perform an isovolume maneuvers have been difficult and therefore alternative techniques for calibration of RIP have been developed which use the different patterns of chest wall motion during tidal volume breathing. A negative aspect of RIP is the validity of the coefficients’ estimation that is limited to the tidal volume under conditions matched to those during which the calibration was performed.