JAC()E}S
PUBLISI-IERS
h
OPEN ACCESS
Jacobs
Journal
of
Cancer Science and
Research
Research article
Second
Primary
Lung
Cancer: A
Current
Problem
in
Long-Survivor
Cancer
Patients
Felice
Mucillir-,
Pierpaolo Camplese'. Ciuseppe Cipolloner, f)ecioDi
Nuzzor. Massimolppoliti'.
Luigi
Cuettir, Marco Priolettar.Mirko
Barone', Antonia Rizzuto:. Rosario Sacco2lAepartment of
Qeneraf an[[froracic Surgery, 'Ùniversitl "§.
finnunzio
"- Cfiieti,Ita[J
2Aepartment of fotefica[an[surgicaf Sciences,'l)niversitl "foLagna Qraccia'- Qatanzaro,
Itatl
"Coresporu{ing autfror: iSrofessor fefice futuciffi, Associate cProfessor
of
T froracic Surgery, Airectorof
tfre Departmentof
Qeneraf
an[
llfioracic Surgery, Scfioof of Speciafizationin
Ifrorack Surgery, 'tJniversitl 'Q.fAnnunzio
'-Cfrieti(Itob),
'fe[
+390871358288,+ 39087 1 3 5 8289; Emai[ [email protected]
tfuceberf:
01-17-2016jlccepted:
02-18-2016 tPu6fi.sfied: Copytigfit:A
2016 gvluci[[iAbstract
Background:
Lung may be the site of synchronous or metachronous secondprimary
malignancies (SPM)with
an incidence between 0.8 and 14.50lo ofcases. Synchronous or metachronous SPM present,howevel
diagnostic andtherapeutic
challeng-es. The authorsreport their
experience in thetreatment
of secondprimary
ìung tumors.Methods:
A retrospective studyfrom
2008to
2074 was conductedin
patientswith
synchronousor
metachronous secondprimary
lung cancer.Results:
30patients
(69.8o/o)underwent to pulmonary
lobectomy, 4 (9,3o/o) to segmentectomy and 6 (74.0o/o) to wedge re-sections [Table n.1J. Lung-sparing resections werereferred
to patientswith
unsuitablerespiratory
volumesfor
anatomicalones. The presence
in
the medicalhistory
ofan
intra- or
extrathoracicprimary
cancer doesnot significantly
influence sur-vival,while
the secondprimary
malignancy's stage is crucial.Conclusions:
Lobectomywith
hilar-mediastinal
lymph node dissection should be offered to all suitable patient.Keywords:
SecondPrimary
Lung Cancer;Martini
and Melamed'sCriteria;
Lobectomy; OveraÌl Survival.Abbreviations
SPLC: Second
Primary
Lung Cancer; SPM: SecondPrimary
Malignancies;DFI: Disease Free
Interval
Introduction
Lung cancer is the leading cause of cancer-related death [1].
Non small cell lung cancer [NSCLCJ and Small cell
lung
can-cer (SCLC) are the ma;'or histotypes,with
the previous repre-senting about 85% of cases [2,3]. The lung may be the siteof
synchronous or metachronous second
primary
malignanciesISPM)
with
an incidence between 0.8 and 74.5o/o of cases [4]. Howevecsynchronous
or
metachronous
SPMs presentdi-agnostic and
therapeutic
challenges.In
fact, occasionally,it
isdifficult
to differentiate
a SPMfrom
a local recurrenceor
distant
metastasis.Martini
andMelamed's [5]
andAntakli's
[6]
diagnosticcriteria
are universally accepted. TheAuthors
report
their
experiencein
thetreatment of
secondprimary
Jacobs Publishers
2
lung tumors.
Material and Methods
This study involves 43 patients
with
a meanof
69.5 yearsof
age, observed
in our
lnstitutions
from
2008to
2014
(Table n.1). Inclusioncriterion
was the presence of a diagnosedsyn-chronous
or
metachronous secondprimary
Ìungtumor
[ac-cording to
Martini
and Melamed's and Antakli's diagnosticcri-teria); while
exclusion one was the presence of a pulmonarymetastases from extrathoracic or thoracic cancers. Aim of the study was to assess patients' outcome and to analyze
risk
fac-tors
(such as hystology, demographic datasJinterfering
with
cumulative
survival
andwith
prognosis.All
patients
under-went total
body CT andby
PET-CT scans and were assessedfor
livec
kidney, bone marrow,heart
(echocardiogram studywith
ejection fraction), andrespiratory
(PFR and blood gases)functions.
Table n.1. Second primary lung cancer patients.
N o//o Demographics Ser Male Female Age Smoking history 107
Table n.2. First primary malignancies
N % Site Histology Third primarv cancer
Colon-rectum
8Upper GI tract (stomach,
pancreas)
3Urologiul tract (kidnet blodder, prostate, 12
adrenal gland, penis) Breast Larinx Lung Parathyroid Sfir Eye Blood Uterus Adenocarcinoma
Ep idermoid squamous ca rcinoma
Le pi di c a d eno c a r c ino na
Cleur cell carcinona
Ductal carcinoma
Melanona
Transitional cell carcinoma
Lambda nonoclonal gammopathv
18.6 7,0 28.0 I t,6 7,0 14,0 7l t1 L,) 2,3 ,)1 l9 6 I 4 5 3 4 I M,t l4 ,t q1 I 1,6 7,0 9,3 2,3 l6,l 83,7 i2
ll
69,5+8,64 (48-84) l3 74,4 )56 32,6\T)
41,9 Yes No 7 36 No Former Previous chemotherapy t4 l6 l8 Table n.3.Second primary lung cancer: characteristics.
25 58,1
Death
Yes
No
Disease Free Intervall 59,26+40,74
Overall Survival 80,40+40,33 (10-231)
Overall survival (Lung) 2r,l+12,08 (3-49)
13 patients (30.2o/o) were smokers, 16 (37.2o/o) former
smok-ers and
74
(32.60/o) hadno history of
smoking. Urological,colorectal, breast cancer and
lung
cancer were the prevalentfirst primary
neoplasms,followed by
laryngeal
and
upper gastrointestinaltract
ones fTable n.2).78
patients
(47.9o/o)were previously treated
with
adjuvant chemotherapy for thefirst
primary
cancer. Right lung was the predominant sitefor
second
primary
lung malignancies [n. 37-
72.09o/o). Histolog-ically, adenocarcinoma wasthe
predominanthistotype
(n.25-
46.50/o), followed by squamous carcinoma and bylepidic
or papillary adenocarcinoma(former
BAC) (Table n.3).Occurrences reflect the current epidemiology
oflung
cancer. In fact, there has been a turnaroundin
incidence and prevalencebetween adenocarcinomas and squamous carcinomas [7-10]. Finally, 93o/o (n.
40)
of patients
hada
metachronous tumo4Hystology Lobe Occurrence Thcrapeutic stratcg\ Adenocurcinoma Lep i di c ad e no c a rc i n o ma P api I I ary adenoc a rcinoma
Epidermoid squtmous carcinoma Large cell carcinona
Right upper lobe Middle lobe Right inlerior lobe Le[t upper lobe Left inferior lobe
Synchronous Melochrofioas Surgery Surgery + chemolherapy Chemotherapy N 20 7 J ll 1 t7 2 t2 6 6 3 40 46,5 16,3 7,0 25,6 4,7 l3 30 10,2 69,8 39,5 4,7 )7 0 14,0 14,0 23 l6 4 7,0 93,0 58, I 32,6 o1
Cite this article: Felice Mucilli. Second Primary Lung Concer: A Current Problem in Long-Survivor Concer Patients. I I Concer Sci Res. 2016, 2(1): 028.
Jacobs Publishers
3
while 7o/o [n.3) a synchronous one
Statistical Analysis
All data are presented as frequencies INJ and simple
percentag-es (%). Bivariate analysis of some variables was accomplished
and statistically significant results were defined as p less than
or
equalto
0,005. Patient overall survival was expressedac-cording
to the
Kaplan and Meier's method.[n
particular; the survival function was adoptedfor
the analysis of disease-freeinterval
[DFIJor
the histological correlationin
relation to pa-t'ients' outcome.Results
37 (72.090/o) patients presented
with
aright
secondprimary
lung carcer (SPLC),
with
a prevalence for theright
upper lobe.All patients were staged according to the seventh edition of the
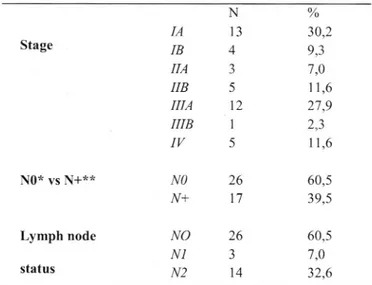
TMN lung cancer staging system (Table n. 4).
Table n.4. Second primary lung cancer: staging.
Stage o//o 30,2
ql
7,0tt,6
)1
q/,)
I 1,6 N0* vs\l+**
severe
comorbidities.
Surgicalstrategy was confident with
the guidelines of
the
European Societyof
Thoracic Surgeons (ESTS) and the American Society of Thoracic Surgery (AATSI.A
hilar-mediastinal
lymphadenectomy has been always per-formedin
orderto
assessthe
presence oftumoral
lymphatic disseminationor
skip metastasis, since lung cancer shows alymphotropic behavior both in progression and dissemination.
Referring to our data, previous chemotherapic protocols was a
negative prognostic factor. In fact, patients who had undergone chemotherapy
for the
first
primary
tumor, showed a median survival of84.9t6.5
monthsvs
749.0t26.9 monthsin patient
with
nohistory
[p <0.005). In the secondpart
of the study, weanalyzed the relationships between
the
Disease Free Interval(i.e. the time between
the
diagnosis of theprimary tumor
and second primarytumor)
and the Overall Survival. In this regard, we proceeded by dividing the populationinto
cohorts in orderto
havefour
independent braces: patientswith
early onsetof
secondary neoplasm (DFI: 0-36 months), patients
with
rela-tive
early onset of cancer (DFI: 37-72monthsl,
patientswith
relative late
onsetof
malignancy (DFI: 73-108 monthsJ,pa-tients
with
late onset of malignancy (DFI> 108 months).Compared
to our
results,it
can be arguedthat
patientswith
late
or
relativelylate
onset secondprimary lung
cancerpre-sented
the
highestsurvival
rates (DFI>1.08: 180 months vsDFI0-36: 58.9
monthsJ(p<0.001) (Figure
n
1).
Finally, the presenceof a
correlation
betweenhistological
concordancebetween the
first
and the secondtumor
and overall survivalwas found [p<0.001) (Figure n 2). From the data
it
followsthat
the
presence of a histological concordance betweenfirst
and second neoplasmis a
positive prognostically factor vis-a-vis collision forms.Discussion
The prevalence
oflong
surwivor cancer patients has increased due to rising incidence and improving survival [11-13]. Second and higher-order malignancies now comprise about 18.00/oin
the USA [14]. Therefore, there is an increasing need
to
deter-mine therisk
of secondprimary
cancer developmentprovid-ing an appropriate
surveillance andbehaviour
advicesI
i.e.smoking
cessation). Cancerpatients
havean
increasedrisk
for further primary
tumors andthis might
be expectedto
be raised due to improvement of overall survival, on the one hand,and
dueto
the persisting
effectsof
genetic and behaviouralrisk
factors (such as tobacco use, excessive alcohol intake, andobesity), genetic predisposition, environmental determinants, host effects and side-effects of medical therapies (chemo- and
radiotherapy) [15].
An important theory
often usedto
explainthe
occurrence fomultiple
malignancies is the " Slaughter's concept of fieldcan-cerization". This
latter
statesthat
exposureto the
same car-cinogenic agents increases the chance of multiple tumorsIA IB IIA
IIB
IIIA
IIIB
IV
Nl3
4 J 5t2
I 5Lymph
node status NO N+ NO N1 N2 26l7
26 Jt4
60,5 ?q5 60,5 7,0 32,6 *N0: no lymphnode metastasis++ N+: hilar or mediastinal (homolateral and controlateral)
Iymph-node metastasis
Interestingly, 46.5% presented
with
early
stage disease, i.e.stage IA-llA. In our opinion, this seems to be related to cancer
follow-up programs (laboratory and radiology) allowing
anearly detection of second lung tumors in cancer patients.
3 patients, due to the presence
ofan
advanced disease,under-went to
fine-needle transthoracic lung biopsy. In the remain-ings, apuìmonary
lobectomy wasperformed
in
30
patients(69.8o/o), a segmentectomy in 4 (9.3o/o) and a wedge resections
in
6
(74.00/o) (Tablen.3).
Lung-sparing resectionswere
re-ferred to patients
with
unsuitable respiratory volumes orwith
Jacobs Publishers
4
Figure n.1: Disease free interval (from the first primary tumor to lung cancer] vs overall survival.
0
,00 nn
Qverall survival
Figure n.2. Effect of histological concordance/discordance on overall.
50,00
100,00
150,00Overal! sur\rival
200.00 0E
.= L=
gt (u§
3 E C' Cluster time of f ÉCUrfÉnr:e .7! '- ,73-108 08 .72-truncated 08-lruncatec.l 0E-truncaled , - 'ADK+Carcinoma ,-'ADK+other l Carcinoma+otlìer ADK+ADK-Iruntrated ADK+Carcinoma-truncsled ADl{+other-truncated Careincma+other-truncsted Carcinoma+soreinoma-truncatedFirst vs second primary histology
E
.= L=
vl (u g fit:
J E L) 0-
+- -l{
-"+
++
+-,
Cite this orticle: Felice Mucilli. Second Primary Lung Cancer: A Cuuent Problem in Long-Suruivor Cancer Patients. J I Concer Sci Res. 2016, 2(1): 028. I I I I I I I I I I I +
t
+ ,00Jacobs Publishers
5
[16].
Infact,after
thetreatment
of aprimary
tumol
the risk
of developing a second
primary
neoplasm increases [17]with
a ratethat
variesfrom
4.2o/oto
28.4o/o. Secondprimary
lungcancers (SPLCs) may present as synchronous
and
metachro-nous lesions, according toMartini
and
Melamed'scriteria
[5]or Antakli's
ones [6]. The incidence of these lesions presentspeculiarities:
in
fact,while
for the previous ones has been ob-served a plateau phasein
terms
of incidence;for the
latters,the trend appears increasing [18].
Synchronous
tumors
are significantly
rarer than
metachro-nous
tumors
[19]; as reported, the incidenceofa
synchronous secondprimary
lung cancer varies from 0,26 to 7,33o/o 120,211.The criteria for defining a second primary tumor have changed over time. Historically,
Martini
Melamed'scriteria
[5]
and
An-takli's
ones[6]
represent
the
first
attempt
to
systematizeand
define
a
secondprimary
tumor. Nowadays,two
panelsof rules are
widely
used:the
rules of the SurveillanceEpide-miology and End Results (SEER) Program 122) and those
de-veloped by the International Association of Cancer Registries (IACR) and
the International
Agencyfor
Researchon
Cancer (IARCJ 123,241. The SEER system takes account of histology, site, laterality and latency time from thefirst
tumor; while, the second includes only atumor
to an organ. Diagnosticsensitiv-ity
has increased due to the adoption ofworldwide
screeningprogrammes 125,261and the improvement of medical imaging technologies [27].
Most patients
with
SPLC present an early-stage disease [28].The reasons can be attributed, as reported by Shields et al [29],
in
a reguÌar and systematic follow-up for cancer patientsaim-ing not only in identifying a recurrence or a metastatic spread,
but also the onset of a second
primary
lung cancerin
its earlystages.
ln
our studywe
reportedthe
majorityof
patients
with
sec-ond
primarylungtumors
exhibits
a 36-months survivalratescomparable to patients
with first primary
lung cancer [Figuren.4); Therefore
it
would seem that thefirst
neoplasm doesnot
interfere
with
the patient outcomes, but this latter is sublectedto independent factors as the clinical stage and the early onset of a second
primarytumor
[p <0.001).Koppe et al. [30] did not find any difference in survival between patients
with first
NSCLC and patientswith
a secondprimary
tumor
foundin
folÌow-up period. This circumstance suggeststhe prognosis of NSCLC patient
with
previous malignancies ismore conditioned by the natural
history
of NSCLC rather thanby the previous one.
Liu et al. [31] showed that the median survival of patients
with
a lung cancer as a second
primary
malignancy was better thanthe general lung cancer population. HoweveL data are contro-versial. One explanation
for
the comparatively good survival,for
example, is the greaterproportion
of patientsin
Stage Ior
early stages.
The prevalent sites of a
first primary
cancerin
relation to NS-CLC are clinicallyimportant in
orderto
facilitate effective fol-low-up and to stay alert for second malignancies. In this study,the most frequent sites of
the
first
primary
cancerwere
col-orectum, breast,lung and the urinary tract in order of frequen-cy. Duchateau et al. [32], instead, reported the most frequentlydiagnosed double cancers were in the lungs, the head and neck
region, and the
urinary tract;
while, Liu et al.[31]
reported aclosed association among
lung
cancer;upper airway
tumorsand colorectal
cancer.Identification
of the "risk
period"
as well as the prevalent site of relapsing malignancies could help physicians to define programs of surveillance for survivors. Inthe present study, 38,640lo (n.17) of the second
primary
malig-nancies occurred
within
5 years. Most SPLCs were diagnosed 5 years or later after diagnosis of the firstprimary
cancer whichis
somewhatsimilar to two
retrospective studieson
surgi-cal patients
developing metachronous SPLC[33-35].
Histologically, we found the concordance between histological types present a better prognosis, although
this
evidence doesnot
find
acceptancein
the case of double epidermoid tumors.As reported by Shen et al. [36] in this latter the highest rates of genetic recombination (microsatellite alterations, loss of het-erozygosis) cause a sort
of
"synergic" biological resistance.In Literature, excellent results in terms of survival are
report-ed
for
patients undergoing resection of a SPLC[37].
Surgicaltreatment, whenever feasible,
is
considered
the
modalityof
choice
for
the
management of patientswith
secondpri-mary lung cancers [38,39]. The type and extent
ofsurgery
areunder discussion.
Zuin
et
aÌ
[40] reported that
lobectomyfor
metachronous
and
synchronous second
primary
lungcancer exhibited a statistically significant positive association
with
survival rate. By contrast,other
surgicalseries
report-ed that
type
of
resection (sublobar vs.
more extensive)for metachronous second
primary
lung cancer did notpredict
survival
135,47,421. Zuin etal
[a0]
observed no difference in recurrence rates between patients who underwent lobectomy (3.3o/o) and those who underwent sublobar resection (5%)for
metachronous and synchronous second
primary
lung cancers.Conclusions
Second
primary
malignanciesare
a
common
occurrence in long-survivor cancer patients. Epidemiological characteristics(high
prevalence
of
early
stage cancer)
and
the
use
ofnew
technologiesallow
effective diagnostic classification. We believe that a secondprimary
lung cancer should be treated asa
first
cancer; becauseit
is atumor with
its own naturalhisto-ry. Therefore, surgery, whenever is possible, is the standard
of
treatment.
Jacobs Publishers 6
Conflict of
interest:
The authors have noconflict
of interest to be disclosed.Ethical standard:
Thearticle
is in
accordancewith
ethicalstandards.
12. Maddams
f,
Brewster D, Gavin A, Stewardf, Elliott
J et al.Cancer prevalence in the United Kingdom: estimates
for
2008. Br J Cancer.2009,707:547-547.
13. Forman D, Stockton D, Moller H, Quinn M, Babb P et al.
Can-cer prevalence in the UK: results from the EUROPREVAL study.
Ann Oncol. 2003, 1.4:
648-654.
Research
involving human participants and
or
animals:
The article does not contain any research
with
humanpartici-pants performed by the authors
Informed
consent: For this type of study, no formal consent isnot required. It is an anonymous one.
References
1. f emal A, Siegel R, Ward E. Cancer statistics, 2008. CA Cancer
I Clin. 2008,
58(2):7L-96.
2.
Navada S,Lai
P, Schwartz AG, Kalemkerian GP. Temporaltrends
in
small cell lung cancer: analysis ofthe
national
Sur-veillance
Epidemiology
and
End-Results (SEERJ database[abstract 7082].
I
Clin
Oncol. 2006,24(785J: 3845.3. Sher
I
Dy GK, Adjei AA.Small cell lung cancer. Mayo ClinProc. 2008, 83(31: 35s-367.4.
Adebonojo SA,Moritz
DM, Danby CA. The results of modernsurgical therapy for
multipl primary
lung cancers. Chest. 1997,712
693-707.5.
Martini
N, Melamed MR.Multiple primary lung
cancers. JThorac Cardiovasc Surg. 1975, 70:606-612.
6.
Antakli
I,
Schaefer RF, Rutherford JE. Secondprimary
lungcancer. Ann ThoracSurg. 1995,
59:863-867.
7. Burns DM. Changing rates of adenocarcinoma of the lung. Chem Res Toxicol. 201,4, 27
{8):
1330-1335.9. fanssen-Heijnen ML, Coebergh JW. The changing epidemiol-ogy
of lung
cancerin
Europe. Lung Cancer.2003,2(\:
2a5-258.
10. Toh CK. The changing epidemiology of lung cancer. Meth-ods Mol Biol. 2009, 472: 397 -471..
11. Parkin DM, Bray F, FerlayJ, Pisani P. Global cancer statistics,
2002.CA Cancer
j
Clin. 2005, 55: 74-108.14. Travis LB, Demark Wahnefried W, Allan fM, Wood ME, Ng AK. Aetiology, genetics and prevention ofsecondary neoplasms in adult cancer survivors. Nat Rev Clin Oncol. 2013, 10[5J: 289-301.
15. Curtis RE, Freedman DM, Ron E, Ries LAG, Hacker DG et al. New malignancies among cancer survivors: SEER Cancer
Reg-istries,
7973-
2000. NIH Publ. No. 05-
5302. Bethesda, MD:National Cancer Institute, 2006.
1.6. Braakhuis BJ, Tabor
MB
Kummer fA.A
geneticexplana-tion of
Slaughter'sconcept
of
field cancerization: evidenceand clinical implications. Cancer Res. 2003,
63:7727-7730.
17. Ikeda
Y
Saku M, Kawanake H, Nonaka M, Yoshida K. Fea-tures of secondprimary
cancer in patientswith
gastric cancer. Oncology 2003,65:7\3-777.
18. Haraguchi S, Koizumi K, Hirata T. Surgical tratment of
meta-chronous
non
small celllung
cancer.Ann
ThoracCardiovasc-Surg. 2010,16
319-325.19. Sulkes
A,
Naparstek
Y
Shalit
M,
Kopolovic
f.
Secondprimary
lung
carcinoma. J Surg Oncol. 1980, 15: 375-380.20. Ferguson MK, DeMeester TR,
Deslauriers
l,
Little
AG,Pi-raux M et al. Diagnosis and management of synchronous lung
cancers. I Thorac Cardiovasc Surg. 1985, 89: 378-385.
21. Deschamps C, Pairolero PC, Trastek VF, Payne WS.
Multiple
primary
lung cancers. Results of surgical treatment. J Thorac Cardiovasc Surg. 1990, 99(5): 7 69-777; discussion 777 -778.23. IARC/ENCR/IACR Working Group:
International
rulesfor
multiple primary
cancers. Asian PacificI
Cancer Prev 2005, 6:704-706.
24. International Agency for Research on Cancer: International
Rules
for Multiple
Primary Cancers (lCD-OThird
Edition).ln-ternal Report
No.2004/02.
Lyon: IARC, 2004.25. The NHS cancer screening programmes website.
Cite this article: Felice Mucilli. Second Primary Lung Cancer: A Current Problem in Long-Survivor Cancer Patients. I I Cancer Sci Res. 201.6, 2(1): 028.
Compliance
with
ethical standards
B. Medenica M, Medenica M, Bojovié O, Soldatovié I,
Durutovié
22. Adamo MB, fohnson CH, Ruhl JL, Dickie LA.201'2 SEERPro-I. Changing trends
in
incidence of lung cancer byhistological
gram Coding and Staging Manual. NIH Publication number 12Jacobs Publishers 7
26. Moser K, Sellars S, Wheaton M, Cooke J, Duncan A et al.
Ex-tending the
age rangefor
breast screeningin
England:pilot
study to assess the feasibility and acceptability of randomiza-tion. J Med Screen.
2071,78:96-702.
27. Chopra A, Ford A, De Noronha R, Matthews S: Incidental
findings
on positron
emissiontomography/CT
scans
per-formed
in
the
investigation
of
lung
cancer.
Br
J
Radiol2072,
85:e229-e237 .28. Ishigaki T, Yoshimasu T, Oura S, Ota F, Nakamura R et al. Surgical Treatement for Metachronous Second
Primary
Lung Cancerafter
Radical Resectionof
Primary
Lung Cancer. AnnThoracCardiovasc Surg. 2013, 1, -4.
29. Shields TW. Postoperative lung cancer surveillance. Who, what, when, and why? Chest. 1997, '1.7'1.:11-12.
30. Koppe Ml, Zoetmulder FA, van Zandwijk N. The prognostic significance
of
a previous malignancyin
operable non-smallcell lung cancer. Lung Cancer.
2007,32:47-53.
31. Liu YY, Chen YM, Yen SH, Tsai CM, Perng RP. Multiple
prima-ry
malignancies involvinglung
cancer-clinical characteristicsand prognosis. Lung Cancer.
2002,35:.189-794.
32. Duchateau CS, Stokkel MP Second
primary
tumorsinvolv-ing non-small cell lung cancer: prevalence and its influence on
survival. Chest. 2005, 1,27 : 71,52-1,t58.
33. Doddoli
C, ThomasB
Ghez O. Surgical managementof
metachronous
bronchial
carcinoma. EurI
Cardiothorac Surg.2007,79
899-903.34. Lee BE,
Port
fL,
Stiles
BM.TNM
stageis the
most
im-portant
determinant
of
survival
in metachronous lungcan-cer. Ann Thorac Surg.
2009,88:
1100-1105.35. Aziz TM, Saad RA, Glasser
f.
The managementof
secondprimary
lung cancers. A single centre experiencein
15 years. Eur I Cardiothorac Surg.2002,27:527-533.
36. Cheng Shen, Xin Wang, Long Tian, Guowei Che.
Microsat-ellite
alterationin multiple primary
lung cancer. J Thorac Dis. 207a, 6Q.0): 1499-1 505.37. Haraguchi S, Koizumi K, Hirata T. Surgical tratment of
meta-chronous non small cell
lung
cancer. Ann ThoracCardiovasc-Surg. 2010, 1.6: 379-325.38. Loukeri AA, Kampolis CF, Ntokou A, Tsoukalas G, Syrigos K. Metachronous and synchronous
primary lung
cancers:di-agnostic aspects, surgical treatment, and prognosis. Clin Lung Cancer. 2075, 76(7): 75-23.
41. Battafarano RJ, Force SD, Meyers BF,
Bell
J, Guthrie TJ et al. Benefits of resection for meta chronous lung cancer.I
Tho-rac Cardiovasc Surg. 2004, 127 : 836-842.42.van
RensMl
Zanen
P,de
la
Rivière
AB,
Elbers
HR,van Swieten HA et al. Survival after resection of metachronous
non-small cell
lung
cancerin
727 patients. Ann Thorac Surg.2001,77:309-3 13.
Cite this article: Felice Mucilli. Second Primory Lung Cancer: A Cureent Problem in Long-Suruivor Cqncer Patients. J J Cancer Sci Res.2016,2(1):028.
39. Hamaji M,
Ali
SO,Burt
BM.A
meta-analysisof
resectedmetachronous second non-small cell lung cancer. Ann Thorac Surg. 20 1 5,
99(4):
147 0-1.47 8.40.

![Figure n.1: Disease free interval (from the first primary tumor to lung cancer] vs overall survival.](https://thumb-eu.123doks.com/thumbv2/123dokorg/4966453.53404/4.897.80.819.169.1117/figure-disease-interval-primary-tumor-cancer-overall-survival.webp)