Gut 1996; 38:894-898
Antineutrophil
cytoplasmic antibodies
in
sera
from
colectomised ulcerative
colitis patients and
its
relation
to
the
presence
of
pouchitis
M Esteve,J Mallolas,JKlaassen, A Abad-Lacruz, FGonzalez-Huix, ECabre, FFernandez-Bafiares, X Bertran, E Condom, J Marti-Rague, M AGassull
Departmentof Gastroenterology, Hospital Universitari 'Germans Trias i Pujol', Badalona, Catalonia, Spain MEsteve JMallolas JKlaassen ECabre FFemrndez-Bafiares XBertran M AGassull Department of Gastroenterology, Hospital de Sant Llorenq,Viladecans, Catalonia, Spain AAbad-Lacruz Department of Gastroenterology, Hospital 'Josep Trueta', Girona, Catalonia, Spain FGonzalez-Huix Departmentof Pathology,Ciutat Sanitaria Universitaria deBellvitge, L'Hospitalet, Catalonia, Spain ECondom Departmentof Surgery,Ciutat Sanitaria Universitaria deBellvitge, L'Hospitalet, Catalonia,Spain J Marti-Rague Correspondenceto: DrM AGassull,Hospital
Universitari 'Germans Triasi Pujol', CarreteradelCanyet
s/n,08916Badalona,Spain. Acceptedforpublication
13 December1995
Abstract
Background-Fewstudies have evaluated
the influence of colectomy on
anti-neutrophil cytoplasmic antibody (ANCA)
positivity in ulcerative colitis (UC). In small series ofpatients it has been
sug-gestedthat ANCApositivityin UCmight
bepredictivefordevelopment ofpouchitis
aftercolectomy.
Aimns-To
assess theprevalence ofANCAinUC patients treatedby colectomy anda Brooke's ileostomy(UC-BI)orilealpouch
anal anastomosis (UC-IPAA), and the
relation between the presence ofANCA,
the type ofsurgery, and the presence of
pouchitis.
Subjects-63UCpatientstreatedby
colec-tomy (32 with UC-BI and 31 with
UC-IPAA), 54UC,and24controls.
Methods-Sampleswere obtainedatleast
two years after colectomy. ANCA were
detected by indirect immunofluorescent assay.
Results-There were no differences between patients with
(36/3%)
orwithoutpouchitis
(35O0%)
and between patientswith UC
(550/),
UC-BI(40.6%),
andUC-IPAA
(35.40/o).
However, ANCA preva-lence significantly decreases in the whole group ofoperated patients (38-0%)com-pared with non-operated UC (p=0.044). Conclusions-Theprevalenceof ANCA in
operated patients was significantly lower than innon-operated UC, suggestingthat it mightbe related eitherto the presence
of inflamed or diseased tissue. ANCA
persistence is not related to the surgical procedure and itshould not be used as a marker forpredictingthe developmentof
pouchitis.
(Gut 1996;38:894-898)
Keywords: ulcerative colitis,proctocolectomy,ileal pouch anal anastomosis,antineutrophil cytoplasmic
antibodies,pouchitis.
Ulcerative colitis (UC) and associated condi-tions suchasprimarysclerosing cholangitisare
some of the diseases in which antineutrophil cytoplasmic antibodies (ANCA) have been
described.1-3 UC associated ANCA
(UC-ANCA) most commonly show an immuno-fluorescenceperinuclearpattern. Althoughnot
universally accepted,3 cytoplasmic and mixed ANCA
patterns
have been described associ-atedtoUC.±8
On theotherhand,becausetheantigenic specificity of UC-ANCA is
unknown,'
3 910theyarereferredto asatypical ANCAorx-ANCA bysomeauthors.1-3Few studies have specifically evaluated the influenceofcolectomyonANCA positivity in
UC.4
711-4 As well as only dealing with a small series ofpatients,noneof them includesa large number of cases with Brooke's
ileostomy,whicharethe onlyonesthatmaybe
considered absolutely free of disease. On the otherhand, all these seriesreport ahigh preva-lence of ANCA in patients with pouchitis
(80-100%).4
711-13 Based on the results of thesestudies it has beensuggestedthatANCA assessmentinUCmaybeuseful in predicting the development of pouchitis in patients undergoingIPAA.2Theaims of this studywere (a) toassessthe prevalence of ANCA in UC patients treated withcolectomy and eitheraBrooke'sileostomy or ileal pouch anal anastomosis, and (b) to determine the relation between thepresence of ANCA, thetypeofsurgeryperformed, and the presenceofpouchitis.
Methods
PATIENTS ANDCONTROLS
Ulcerativecolitispatients treated withcolectomy One hundred and forty eight patients with a
diagnosis of UC have had a colectomy since 1973 in three of four hospitals takingpart in thestudy. The diagnosishad been established
by the Lennard-Jones clinicopathological
criteria.15
Patientswithahistoryof indetermi-nate colitis were excluded from the study. Based onthe information available, 92 of114patients livinginCatalonia (31 895
kM2)
could becontactedbyphoneandaskedtoparticipateinthe study. Sixty three of them agreedto be included.ThirtytwohadaBrooke'sileostomy
(UC-BI) (15 male, 17female;43 years (range: 23-76)) and 31 hadanilealpouchanal anasto-mosis (UC-ANCA) (18 male, 13 female; 34 years (range: 24-61)). Thetechnique of IPAA includedmucosectomyofthe anorectal stump in five patients, whereas a staple ileal pouch analanastomosiswasperformedinthe remain-ingcases. In allpatients atwo loop J reservoir
wasmade.
Disease controls
Fifty four UC patients who had not had an
operation(35male,19female;40years(range:
Antineutrophil cytoplasmicantibodies inserafrom colectomisedulcerativecolitispatientsand its relationtothepresenceofpouchitis
TABLEI Clinical characteristics of the ulcerative colitis patients Patients Activity Inactive 21 Mild 21 Moderate 11 Severe 1 Extent Proctitis 16
Leftsided colitis 28
Pancolitis 10 Extraintestinalmanifestations 5 Treatment No treatment 12* Salicylates 37 Corticosteroids 8 Azathioprine 7 Corticosteroid refractory 13
*First episode. Time elapsed from diagnosis:4months (0-25).
19-74)), living in Catalonia, attending the
'Hospital Universitari Germans Trias i Pujol'
were included in the study. The diagnostic
criteriawerethesame asabove.
Healthy controls
Twenty four volunteers, living in the same geographical area (11 male, 13female;43years
(range: 23-72)) actedas ahealthycontrols.
CLINICALASSESSMENT
In all patients a complete clinical assessment wasperformed at the time of blood sampling
for ANCA detection. In non-operated UC
patients this included: activity and extent of the disease, current treatment, time from
diagnosis, extraintestinal manifestations, and outcome. The activity of the disease was assessed by means of the Truelove index.16
Table I shows the clinical characteristics of the non-operated UC patients. The assess-mentofUCpatients treated withacolectomy
included: time from diagnosis and surgery,
TABLE I Pouchitis diseaseactivityindex(PDAI)1415
Criteria Score
Clinical Stoolfrequency:
Usualpostoperative stoolfrequency 0 1-2Stools/day>postoperativeusual 1 3Ormorestools/day>postoperative usual 2
Rectalbleeding:
Noneorrare 0
Presentdaily 1
Faecal urgencyorabdominal cramps:
None 0 Occasional 1 Usual 2 Fever(temperature >37.8°C: Absent 0 Present 1 Endoscopicinflammation Oedema 1 Granularity 1 Friability 1
Lossofvascularpattern 1
Mucous exudate 1
Ulceration 1
Acutehistological inflammation
Polymorphonuclear leucocyteinfiltration:
Mild 1
Moderate+cryptabscess 2
Severe+cryptabscess 3 Ulceration per low power field(mean):
<25% 1
25-50% 2
>50% 3
extraintestinal manifestations, previous and currenttreatment, andpostoperativeoutcome.
Eight patients
with UC-BI wereprevious
UC-IPAA that had failed. Theprimaryreason
forpouchexcisionwaschronicpouchitis resis-tant to medical treatmentin twopatients and fistula and
pelvic sepsis
in sixpatients.Four of the secondgroup also had chronic continuouspouchitis.
None of thesepatients hadindeter-minate or Crohn's colitis. In UC-IPAA
patients, the degree of pouch inflammation
was assessed by means of the modified
Moskowitzindex17 18(TableII).Pouchitiswas defined as a score equal or greater than 7. Eleven of 31 UC-IPAA patients fulfilled this criterionatthetime ofinclusion.
Previous history of confirmed pouchitis
was also recorded. Four of 11 patients with
pouchitisatthetime ofinclusion hadhistoryof chronic continuous pouchitis resistant to medical treatment. Table III shows clinical data of UCpatients treated witha
colectomy.
Some UC-IPAA patients were taking more
than one drug. None of thepatients included hadprimarysclerosingcholangitis.
ANTINEUTROPHIL ANTIBODIES DETECTION Serumwasobtained of allpatientsand controls. Inoperated patients, sampleswere obtained at least two years after colectomy. ANCA were detectedusinganindirectimmunofluorescence microscopy detection method. Commercially
available slides containing cytospin smears of
human ethanol fixed neutrophils (INOVA
Diagnostic, SanDiego, CA) were used as sub-strate. Diluted serum samples in phosphate
buffered saline (PBS) were incubated on the slides for 30minutes. Afterwashing in PBS, the slides were incubated again for 30 minutes with fluorescein conjugated rabbit
immuno-globulins to human immunoglobulin G
(DAKO, Copenhagen, Denmark) at a pre-determined optimal dilution of 1/100 in PBS. Slides were washed in PBS twice, mounted in
glycerol, and read immediately under fluores-cence microscopy at 400X (Axioplan, Zeiss, Germany).
Slides were read by two independent
observers who were unaware of the clinical
diagnosis. Control ANCA positive and nega-tive sera and PBS were included in each test batch. A serum was considered positive for ANCA when a clear perinuclear fluorescence at a 1:20 dilution was observed or when a
TABLEIII Clinicalcharacteristics oftheUC patients
treatedwithacolectomy
UC-IPAA UC-IPAA UC-BI pouchitis nopouchitis
Years fromdiagnosis 14(4-36) 6(2-34) 7(2-24)
Years fromsurgery 9(2-16) 4(2-9) 4(2-9) Clinicalscore* - 2(0-4) 0(0-3) Endoscopicscore* - 4(3-6) 0(0-3) Histologicalscore* - 2(1-5) 1(0-3) Global score* - 8(7-11) 3(1-6) Treatment (patients): No treatment 32 3 14 Salicylates 0 2 3 Local corticosteroids 0 3 0 Antibioticst 0 4 5
*Pouchitisdiseaseactivityindex;tmetronidazole/tetracyclines.
Esteve,Mallolas,Klaassen,Abad-Lacruz, Gonzdlez-Huix, Cabre,Ferndndez-Baniares, Bertrdn,Condom,Marti-Rague,Gassull cytoplasmic staining was observed at a 1:40
dilution. The second cut off dilution was chosen to eliminate unspecific cytoplasmic positivity yielded by some negative sera. All negative sera and those given as positive by onlyone observer were retested blindly. Serum samples given as positive by only one observer induplicate assay were considered as negative. Positive ANCA samples were titrated to a dilution of 1/1280.
To differentiate positive ANCA from anti-nuclear antibodies (ANA) that mimic ANCA, allpositive sera were tested with HEp-2 cells andrat liversections, which are highly sensitive for ANA detection. All ANA positive sera with stronger titres than that observed in neutrophil slides were considered as ANCA negative. This occurred in four patients (three non-operated and one operated) and one healthy
control.
All assays were performed at the Research Laboratories of the Hospital Universitary
'Germans Trias iPujol'.
STATISTICAL ANALYSIS
Comparison of the frequencies between
patients with or without pouchitis were
analysed usingthetwotailx2andYates's cor-rection.ThefrequenciesbetweenUC,UC-IB,
and UC-IPAAwerecompared usinga twotail
X2
and thecomparison
betweenoperated
andnon-operated UC patients was performed using aleftsided Fisherexact test.Titreswere
compared using the Kruskal-Wallis test. The
Spearmanrank correlation coefficientwasused to determine associations between titres and the time elapsed from surgery. The resultsare
expressedbymeansof median andfrequencies
with their range and 95% confidence intervals (CI), respectively. The statistical procedures
were performed using the programs of the Biomedical DataProcessing, BMDP (BMDP,
Statistical Software, Los Angeles, California,
1986).
The positivity of ANCA was significantly
higherin all groups studied compared with the healthy control group (p<0 0001).
Relationbetween ANCApositivity andthe presenceofpouchitis
In patients with UC-IPAA, there were no differences inANCA positivity between those with (36-3% (CI: 109 to 69.2)) or without
pouchitis (35.0% (CI: 15.5 to 59.2)) (p=0.720).
Two offour(CI: 6.7 to 93.2%) patients with chronic continuous pouchitis andfour of eight UC-IPAA failure (CI: 15.7 to 84.3%) were ANCApositive.
As the percentage of ANCA positive
patients was thesameasthose with orwithout pouchitis, theywere considered together and compared with both patients treated with a colectomy and non-operated UC patients to
determine the influence of a Brooke's
ileostomyuponANCApositivity.
Relation between ANCA positivity and thetype
ofsurgeryperformed
There were no differences inANCApositivity between patients with UC-BI (40-6% (CI: 23.7 to59.3)) andUC-IPAA (35.4% (CI: 19.2 to54.6)) andnon-operated UC patients (55% (CI: 41-4 to 69.1)) (p=0 154).
Because there were nosignificant differences between both groups ofoperatedpatients,they were considered together (both UC-BI and
UC-IPAA) and compared with UC
non-operated patients to determine if colectomy
decreases ANCA positivity. There was a
significant decrease in ANCA prevalence in operatedpatients-38.0%(CI: 26.1 to 512)
-compared with non-operated UC (55%)
(p=0044).
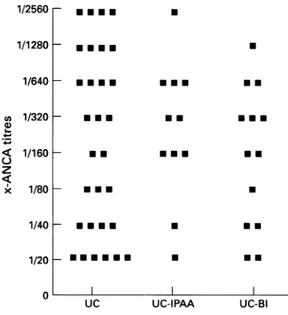
The Figure shows the titres ofANCA and
UC, UC-BI, and UC-IPAA. There were no
differences in ANCA titres between groups
ETHICALCONSIDERATIONS
The studywas performed in accordance with the 1975Declarationof Helsinki ethical
guide-lines and was approved by the Research and EthicalCommittees of theHospitals.
Results
Table IV shows the numberof ANCApositive patients and controls in the groups studied. TABLEIV Number and percentageofANCApositive patients
Positive Negative
Ulcerative colitis 30(55.5%)* 24
UC-BI 13(406%)t 19
UC-IPAA withpouchitis 4(36.3%)A 7
UC-IPAA withoutpouchitis 7(35/0%)§ 13
Healthycontrols 0 24
UC-BI=totalproctocolectomy plusBrookesileostomy,
UC-IPAA=proctocolectomyplusilealpouchanal anastomosis. *26p-ANCA; 1c-ANCA;3mixedpattern,t11p-ANCA;
2mixedpattern,t3 p-ANCA;1mixedpattern,§6 p-ANCA; 1mixedpattern. 1/2560r 1/1280H 1/640
h
CO a) . x 1/320H 1/160[ 1/80H 1/40h
m a ma a a m m a a a ma am* *-ma* m a a a 1/20- a aaUaE ma* a aEa *-m aE m aa a a a a m UC UC-IPAA *-UC-BITitresofANCA innon-operatedukerativecolitispatients
(UC), patientstreated withacolectomy plusilealpouch
anal anastomosis(UC-IPAA)andpatientstreated witha
colectomy plusBrooke'sileostomy (UC-BI).
n
Antineutrophil cytoplasmic antibodiesin serafromcolectomised ulcerative colitis patients and its relationtothe presence ofpouchitis
(p=0755). There was also no correlation
betweenthe timeelapsed fromsurgeryand the titresof ANCA (r=-0098).
Discussion
There is no agreement about those immuno-fluorescence ANCA patterns that should be considered associated with UC. Some labora-tories haveconsidered that allUC-ANCAare of the perinuclear
type,9
19-21 whereas others also include those less frequentcases showing eitherdiffuse cytoplasmicormixedpattern.4-8
Weshare thissecond viewas,until the specific antigen(s) are identified, it does not seem
reasonable to exclude any type of ANCA pattern when an unequivocal
immunofluores-cencestaining is found.
Oneof the aims of this studywastoassess if removal of the colon results in a decline of ANCA inUC patients andif there isarelation tothetype ofsurgeryperformed. The percent-ageof ANCApositivityinourUCnon-operated patients
(55%/o)
issimilarto otherreports,622 23 and is within the range described in publishedreports(40-80%).4-. 19-25Whetherorno circu-lating ANCApersist longtermafter colectomy inUC patientsisnotwellestablished. Although
most studies have reported the persistence of
ANCA after
surgery,47
11-1325 there are some reports of postoperative ANCAdisappear-ance.14
26 However,moststudiesincludeasmall number ofpatientsandnoneof them includesa largenumberofcaseswith Brooke's ileostomy. Although there are no data about the time course of ANCA behaviour after colectomy, wethought thattwo years might be a reason-ableperiodof timeforassessing ANCA clear-ance, assuming that they are related to the presenceof diseased tissue. We havenotfound a significant difference in ANCA positivitybetweennon-operated UC patients,thosewith
UC-BI, and those with UC-IPAA, showing
that these antibodiespersistin the serum ina
high percentage of UC operated patients long term after colectomy. However, we found a
significant decrease of ANCApositivity when both groups of operated patients were con-sideredtogether (thatis,increasing twofold the number of operated patients). This finding
mightdisclose theexistence ofaweak relation between ANCA positivity and inflammation,
ashas been shown insome
studies.6
26 Infact,our non-operated patients showed a
non-significant trend towardsa greaterpercentage of ANCApositivityin those with activeversus
inactive UC (63% v 43%; p=0.13), and in those with extensive disease versus proctitis
(6/3%
v31%; p=007).Analternative explana-tion would be that ANCA clearance after colectomy was a very slow process taking more than two years and a prospective and paired assessment before and aftersurgery in15 UCpatients foundasignificantdecrease in ANCA titres a mean oftwo years after
colec-tomy.14
In our study, no differences between groups with respect to ANCA titres, or any relation between the titres of ANCA and the time elapsed from surgery were found. However,asthiswas not apaired comparison,interindividual differences in the ability of antibody production may have prevented the discoveryof such differences.
Inthisserieswefoundasimilar frequency of ANCA positivity between those patients with and without pouchitis. In contrast, several studies have reported a higher prevalence of ANCA in patients with
pouchitis.4
711-13However, most of them include a small
number of patients with pouchitis or it is not well defined, or
both.4
11-13 In thisregard, todistinguish between relapsing and chronic continuous pouchitis may be relevant. In the largest reported series, in which all patients with pouchitis had chronic inflammation resistant or dependent on medical treatment, frequency of ANCA positivitywas
100%.7
The authors suggest that the strong relationbetween ANCA and pouchitis would be
related to a specific disease pattern (chronic continuous pouchitis) ratherthan to themere presence of
inflammation.7
In the remaining studies, it is not stated if those patients with pouchitis had relapsing orchronic continuous disease. However, a recentstudy published as anabstract,showedthat thosepatientswithout pouch inflammationatinclusion, but withpre-vious episodes of pouchitis, had a
33.30/o
of ANCApositivity.12
Thisfigure issimilartothe percentagefound in ourpatientswithpouchi-tis, mostof themhavingrelapsingdisease. On the other hand, in our series two of four chronic resistant pouchitis and four of eight IPAAfailures hadpositiveANCA.
Takenas awhole,all these data suggest that ANCA would notpredict the development of relapsing pouchitis, and thestrong association between ANCA positivity and chronic con-tinuous pouchitis deserves further confirma-tion. However, even if a 100% association
(sensitivity) could beconfirmed, the low
speci-ficity of ANCA for chronic continuous
pouchitis7
will make the use of this markerdoubtfulas apredictorof this condition. Although all these queries could be only answeredbymeansofalongitudinal study, its
practicabilityseems tobequestionable. Sucha
study would be very long lasting, taking into accountthatpouchitismayappear aslateas 10 years after
surgery.27
28 In the case of chronic continuous pouchitis, an event occurring inonly
5%/o
of the totalIPAA,28
thegreatnumberofpatients to be included would be an addi-tionaldifficulty.
Inconclusion, ANCApersistinahigh
pro-portion of UC patientsafter colectomy and its presence is not related to the type ofsurgery
performed. The lower percentage found in
operated patients suggests that ANCA
positivity might be related to the presence of eitherinflamedordiseasedtissue. On theother hand, ANCA positivity in UC should not be used as a marker for predicting the develop-ment ofpouchitis and, at present, it does not seemagoodparameterfordeciding thetypeof surgerytobeperformedinUCpatients.
Partof thisstudyhas beenpresentedasaposteratthe95th Annual Meeting of the American Gastroenterological
Association held in SanDiegoinMay 1995,andpublishedas anabstract inGastroenterology1995;108:A816.
898 Esteve, Mallolas,Klaassen, Abad-Lacruz, Gonzalez-Huix, Cabre,Femrnndez-Bafnares, Bertran, Condom,Marti-Ragu4,Gassull
1 GrossWL,SchmittWH,CsernokE.ANCAandassociated
diseases:immunodiagnostic and pathogenic aspects. Clin ExpImmunol1993;91:1-12.
2 Shanahan F. Neutrophil autoantibodies in inflammatory
bowel disease:aretheyimportant? Gastroenterology1994; 107: 586-9.
3 Gross WL, Hauschild S, Mistry N. The clinical relevance of ANCA invasculitis. ClinExpImmunol1993; 93 (suppl1):
7-11.
4 Patel RT,Stokes R, Birch D, Ibbotson J, KeighleyMRB. Influence of total colectomy on serum antineutrophil
cytoplasmic antibodiesininflammatory boweldisease. Br
J3Surg1994; 81: 724-6.
5 LamproyeA, BelaicheJ, Louis E, Salmon J, Mahieu PH. Anticorps anticytoplasme des polynucleaires neutrophiles (ANCA) dans les maladies inflammatoires du tube
digestif.ActaGastroenterolBelg1994;LVII:171-6. 6 Broekroelofs J, MulderAHL, NelisGF,Westerveld BD,
Cohen TervaertJW, Kallenberg CGM.Anti-neutrophil
cytoplasmicantibodies(ANCA) in sera from patients with
inflammatory bowel disease (IBD). Relation to disease pattern and diseaseactivity.DigDisSCi1994;39: 545-9. 7 Sandborn WJ, Landers (CJ, Tremaine WJ, Targan SR. Antineutrophil cytoplasmic antibody correlates with
chronic pouchitisafter ilealpouch-analanastomosis. Am JGastroenterol1995;90: 740-7.
8 Sung JY, Chan FKL,LawtonJ, LeungJCK, Liew CT,
Leung NWY, et al.Anti-neutrophilcytoplasmicantibodies
(ANCA)andinflammatory bowel diseasein chinese. Dig
Dis SCi 1994;39: 886-92.
9 Ellerbroek PM, Outkerk Pool M, Ridwan BU, Dolman KM, vonBlombergBME, vondem Borne AEGKr,etal.
Neutrophilcytoplasmic antibodies (pANCA)inulcerative colitis.JClin Pathol 1994;47:257-62.
10KanekoK, Suzuki Y,YamashiroY, Yabuta K. Isp-ANCA
in ulcerative colitis directed against b-glucoronidase? Lancet1993;341: 320.
11 Remaux D, Colombel JF, Heresbach D, Duclos B, Chaussade S,BelaicheJ,etal.Antineutrophilcytoplasmic auto-antibodiesin serafrompatientsafterproctocolectomy for ulcerative colitis.Gastroenterology1993;104: A769. 12 Remaux D, Colombel JF, Heresbach D, Duclos B,
Chaussade S, DuclosJ,et al. ANCA andpouchitis in
ulcerative colitis afterproctocolectomywithileoanal
anas-tomosis.Gut 1995; 37: A162.
13 Vecchi M, Gionchetti P, Bianchi MB, Belluzi A, MeucciG, Campieri M,etal.p-ANCA and development ofpouchitis
in ulcerative colitis patients after proctocolectomy and
ileoanalpouch anastomosis.Lancet1994;344:886-7. 14 AitolaP, Miettinen A,MattilaA, Matikainen M,SoppiE.
Theeffectofproctocolectomy on serum antineutrophil cytoplasmic antibodies in patients with ulcerative colitis. Gastroenterology1995; 108: A769.
15 Lennard-Jones JE. Classification of inflammatory bowel
disease.ScandJ7Gastroenterol 1989; 24(suppl 170):2-6. 16Truelove SC, Witts U. Cortisone in ulcerative colitis.
Reportontherapeutic trial.BMJ31955; 2:1041-6.
17 Moskowitz RL,Shepherd NA, Nicholls RJ.Anassessment of inflammation in the reservoir after restorative procto-colectomywith ileoanal ileal reservoir. Dig Dis Sci 1986; 1: 167-74.
18 Sandborn WJ, Tremaine WJ, Batts KP, Pemberton JH,
PhillipsSF.Pouchitisafterileal pouch-analanastomosis:
apouchitis disease activity index. MayoClinProc 1994; 69:409-15.
19 SaxonA, SanahanF, Landers C, Ganz T, Targan S. A dis-tinct subsetofantineutrophil cytoplasmic antibodies is
associatedwithinflammatorybowel disease.JAllergyClin Immunol 1990; 86: 202-10.
20 Oudkerk Pool M, Ellerbroek PM, Ridwan BU, Goldschmeding R,vonBlomberg BME, Pefia AS,etal.
Serum antineutrophil cytoplasmic autoantibodies in
inflammatory bowel disease are mainlyassociated with ulcerative colitis. Acorrelation studybetweenperinuclear antineutrophil cytoplasmic autoantibodies and clinical
parameters, medical and surgical treatment. Gut 1993; 34:46-50.
21 OudkerkPool M, RocaM,RemauxD,BoumaG,PeflaS, ColombelJF,etal.Thevalue ofp-ANCAas aserological marker for ulcerative colitisindifferentEuropeanregions. EurJGastroenterolHepatol1994; 6: 399-403.
22 LeeJCW, Lennard-Jones JE, Cambridge G.Antineutrophil
antibodies in familial inflammatory bowel disease. Gastroenterology 1995;108:428-33.
23 Duerr RH, Neigut DA. Molecularly defined HLA-DR2
allelesinulcerative colitisanantineutrophil cytoplasmic antibody-positive subgroup. Gastroenterology 1995; 108: 423-7.
24 DuerrRH, TarganSR, LandersCJ,LaRussoNF,Lindsay KL, Wiesner RH, et al. Neutrophil cytoplasmic
anti-bodies: alink betweenprimarysclerosing cholangitisand
ulcerative colitis. Gastroenterology 1991; 100: 1385-91. 25 Duerr RH, Targan SR, Landers CJ, Sutherland LLR, Shanahan F. Anti-neutrophil cytoplasmic antibodies in
ulcerative colitis. Comparison with othercolitides and
diarrheal illnesses. Gastroenterology 1991; 100: 1590-6. 26 Rump JA,Worner I, Roth M, Scholmerich J, Hansch M,
Peter HH.p-ANCA of undefinedspecificityinulcerative colitis: correlationtodiseaseactivity and therapy.AdvExp
Med Biol 1993; 336: 507-13.
27Luukkonen P, Jarvinen H, Tanskanen M, Kahri A. Pouchitis-recurrenceoftheinflammatory bowel disease?
Gut 1994; 35: 243-6.
28 SandbomWJ. Pouchitisfollowing ileal pouch-anal
anasto-mosis: definition, pathogenesis, and treatment.