Address for correspondence: Luca Santini, MD
Division of Cardiology
University Hospital of Tor Vergata Viale Oxford, 81
00133 Rome, Italy [email protected]
Clinical
Investigations
An Increased Endothelial-Independent
Vasodilation Is the Hallmark of the Neurally
Mediated Syncope
Luca Santini, MD, PhD; Ambrogio Capria, MD, PhD; Valentina Brusca, MD;
Arianna Violo, MD; Francesca Smurra, MD; Iside Scarf `o, MD; Giovanni B. Forleo, MD, PhD; Lida P. Papavasileiou, MD; Mauro Borzi, MD; Francesco Romeo, MD, FESC, FACC Division of Cardiology, Internal Medicine Department (Santini, Brusca, Smurra, Scarf `o, Forleo, Papavasileiou, Borzi, Romeo) and Division of Internal Medicine, Internal Medicine Department (Capria, Violo), University of Rome ‘‘Tor Vergata,’’ Rome, Italy
Background: The neurally mediated syncope (NMS) is sustained by complex cardiac and vascular reflexes, acting on and amplified by central autonomic loops, resulting in bradycardia and hypotension.
Hypothesis: Our aim was to assess whether the pathophysiology of NMS is also related to an abnormal peripheral vasoreactivity.
Methods: We evaluated by ultrasound the flow-mediated vasodilation (FMD) and the nitrate-mediated dilation (NMD) in 17 patients with NMS, induced by drug-free tilt test in 6 subjects and by nitrate-potentiated tilt test in the other 11 cases; the syncope was classified as vasodepressive (VD) in 8 cases, cardioinhibitory (CI) in 7, and mixed in 2.
Results: The FMD was not different from controls (10.2± 4.5 vs 11.4 ± 3.9, P = ns), with normal recovery times; the NMD was greater in fainting subjects than in controls (26.7± 7.3 vs 19.0 ± 3.6, P < 0.05), with higher values in VD than in CI syncope (31.1± 7.0 vs 23.1 ± 5.0, P = ns); compared to controls, subjects with NMS showed normal recovery times after FMD but longer recovery times after nitrate administration (13.0± 5.6 vs 6.3 ± 0.7 minutes, P < 0.05).
Conclusions: The evaluation of endothelial function supports evidence that NMS is characterized by a marked and sustained endothelial-independent vasodilation, in the presence of a normal FMD; vascular hyperreactivity in response to nitrate administration is particularly overt in vasodepressive syncope and can explain the high rate of responses to nitrate administration during tilt test.
Introduction
The pathophysiologic mechanisms of the neurally mediated syncope (NMS), consisting of a transient loss of conscious-ness and postural tone, are complex and seem to involve changes in the autonomic and vascular tone, resulting in a reflex bradycardia with a marked hypotension, debated to be active or passive in origin.1 – 4
Head-up tilt test is a powerful, low-risk method able to identify patients affected by an NMS; a positive response to the tilt test, reproducing the syncope, may explain the pathophysiologic cardiovascular mechanism specific for each patient. Patients experiencing a syncope driven by a deep reflex bradycardia or asystolia may be treated by cardiac pacing, which seems to be more effective than β-blockade for the prevention of syncopal recurrences in
The authors have no funding, financial relationships, or conflicts of interest to disclose.
highly symptomatic vasovagal fainters with relative brady-cardia during tilt-induced syncope.5 On the other hand,
pharmacologic therapy was shown to be disappointing in subjects with vasodepressive (VD) syncope, providing only a poor reduction of the recurrence of clinical events.6,7
Recent studies have focused on mechanisms of the peripheral circulatory regulation in subjects affected by NMS. Both invasive and noninvasive methods have been used to identify an active or passive mechanism driving to the peripheral vasodilation8 – 11; several articles have
underlined the central role played by the endothelium for the regulation of the vascular tone, justifying the study of endothelial function in subjects with a history of syn-cope using a direct, noninvasive method.12 – 15 We tested
the hypothesis that subjects with a tilt-induced syncope, especially if occurring after nitrate administration, may present an abnormal vascular reaction, independently of the response to the flow-mediated vasodilation (FMD); further-more, we evaluated the clinical implication of the endothelial function at 2-year follow-up in these subjects.
Received: July 8, 2011 Accepted: September 11, 2011
Clin. Cardiol. 35, 2, 107–110 (2012)
107
Published online in Wiley Online Library (wileyonlinelibrary.com)Methods
We evaluated 17 consecutive outpatient subjects, age 35.8± 16.0 years (8 men and 9 women), referred to our Department of Cardiology for a recent recurrent syncopal spell and with a positive response to the tilt table test. No patient was receiving pharmacologic therapy. All patients were nonsmokers and free from cardiovascular, immuno-logic, and neurologic diseases, as assessed at the clinical investigation, standard 12-lead electrocardiogram (ECG) and 24-hour ambulatory ECG, Doppler echocardiogram, and electroencephalogram. The results obtained by the study of the endothelial function in these patients have been com-pared with those coming from the same study performed in a control group consisting of 15 healthy subjects (9 men and 6 women) free from syncopal attacks, age 39.9± 12.5 years.
Head-up Tilt Test
The subjects underwent tilt testing in the morning in a quiet room, after overnight fasting, at a room temperature of 22◦C, recording the systodiastolic blood pressure with a sphygmomanometer at 5-minute intervals and monitoring the cardiac rhythm with a 12-lead ECG device (Esa Ote P80 Power; Esa Ote Biomedica, Castenaso, Italy); the procedure was carried out using an electronically controlled tilt table, with a footboard support (VDE 0551; Ferrox C.I.A.R., Codogn ´e [TV], Italy), upright at 60 degrees for 30 minutes; if the passive tilt test phase was negative, each subject received 300µg of sublingual nitroglycerine spray (Natispray; Teofarma, Pavia, Italy), continuing the test for 15 more minutes; head-up tilt test was stopped at the induction of the syncope, and the observed responses were classified using the Vasovagal Syncope International Study (VASIS) criteria, as mixed (VASIS-1), cardioinhibition (VASIS-2A), severe cardioinhibition/asystole (VASIS 2-B) or pure vasodepression (VASIS-3).16 – 19
Endothelial Function Study
Endothelial function was studied using ultrasound tech-nique according to current guidelines, and the evaluation was performed 2 days after the head-up tilt test. The brachial artery reactivity was assessed in the morning, in a fasting, resting, and supine state; patients maintained clinostatic position for 20 minutes, at a room temperature of 22◦C. The imaging of the brachial artery, 2 to 5 cm above the antecubital fossa, was obtained with a high-resolution ultra-sonographic device equipped with a 10-MHz linear-array transducer (Agilent ImagePoint Hx; Agilent Technologies, MA). The left brachial artery was scanned over a longitu-dinal section, obtaining good-quality frames synchronized on the R wave of the ECG. The blood flow velocity of the brachial artery was measured by pulsed-wave Doppler sig-nal, placing the sample volume in the center of the artery; peak flow rate echo-Doppler measurements were performed on the brachial artery at rest, during reactive hyperemia, and after sublingual nitrate administration. Measurements of the artery internal diameter were taken from the anterior to the posterior wall at the interface between media and intima or to the hardest echo (‘‘M’’ line), at end diastole; the ultrasound transducer was maintained on the brachial
artery by a dedicated stereotactic probe-holding device. In our laboratory, the inter- and intraobserver variability of diameter measurements was <3%.
The endothelium-dependent FMD was assessed by measuring the maximal increase in the internal diameter of the brachial artery during reactive hyperemia evoked by the release of a cuff inflated to 250 mm Hg for 5 minutes on the upper arm, distal to the measurement site. After cuff deflation, the maximal peak flow rate was measured at 15’’ and 30’’; the changes in brachial artery diameter were continuously recorded and were measured each 30’’ for 6 minutes until each patient recovered the basal values and were reported as a percentage of the baseline. Reference normal values for FMD were≥5%.14,15
After a rest period of 15 minutes, baseline measurements (diameter and flow velocity) of the brachial artery were repeated, and the endothelium-independent vasodilatation was evaluated by sublingual administration of 300µg of nitroglycerine (Natispray); thereafter, the diameter of the brachial artery was measured every 30 seconds until each patient recovered the basal values; the changes in brachial artery diameter were reported as percentage of basal values. Reference normal values for nitrate-mediated dilation (NMD) were≥10%.15,16Investigations were in accordance
with the Declaration of Helsinki.
Statistical Analysis
Data are expressed as mean ± standard deviation if not otherwise stated. Obtained variables were tested for normal distribution by the Kolmogorov-Smirnov test. The values obtained in each group and the differences between measurements were analyzed by paired or unpaired Student ttest or by analysis of variance for repeated measurements, followed by the Bonferroni test; the Wilcoxon test was used when otherwise appropriate. Linear regression analysis with Pearson correlation coefficient was used to investigate the relationship between variables of interest. Results were considered statistically significant if P < 0.05; differences between fainting subjects and controls were calculated with the unpaired t test; differences within each group, in different conditions, were calculated with paired ttest. In all tests, statistical significance was defined as P < 0.05.
Results
The NMS, induced by tilt test, in our 15 patients, was classified as cardioinhibitory (CI) in 7 cases (VASIS-2A in 4 and VASIS-2B in 3), VD in 8 (VASIS-3), and mixed in 2 cases (VASIS-1); all but 1 of the subjects with VD syncope were women and were significantly younger than CI patients, (21.9± 4.6 vs 49.7 ± 11.8 years, P < 0.05).
Compared to the controls, patients showed lower basal values of systolic blood pressure (113.2± 14.8 vs 125.7± 7.3 mm Hg, P < 0.05), diastolic blood pressure (60.0± 8.8 vs 78.7 ± 3.2 mm Hg, P < 0.05), with similar heart rate values (66.4± 9.2 vs 68.2 ± 9.8 bpm, P = ns).
The drug-free tilt test phase induced the syncope in 6 subjects, at 19.5± 7.3 minutes of passive standing (CI in 3 cases and VD in 3); the other 11 patients developed syncope during the nitroglycerine-potentiated phase, at
108
Clin. Cardiol. 35, 2, 107–110 (2012) L. Santini et al: Endothelial function in NMSPublished online in Wiley Online Library (wileyonlinelibrary.com) DOI:10.1002/clc.20990 2011 Wiley Periodicals, Inc.
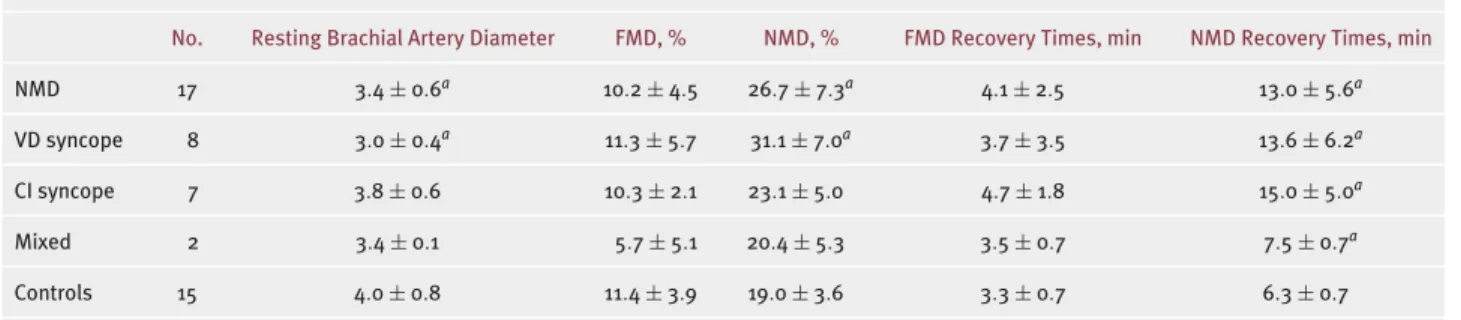
Table 1. Results of Endothelial Function Study in Population and Controls
No. Resting Brachial Artery Diameter FMD, % NMD, % FMD Recovery Times, min NMD Recovery Times, min
NMD 17 3.4± 0.6a 10.2± 4.5 26.7± 7.3a 4.1± 2.5 13.0± 5.6a
VD syncope 8 3.0± 0.4a 11.3± 5.7 31.1± 7.0a 3.7± 3.5 13.6± 6.2a
CI syncope 7 3.8± 0.6 10.3± 2.1 23.1± 5.0 4.7± 1.8 15.0± 5.0a
Mixed 2 3.4± 0.1 5.7± 5.1 20.4± 5.3 3.5± 0.7 7.5± 0.7a
Controls 15 4.0± 0.8 11.4± 3.9 19.0± 3.6 3.3± 0.7 6.3± 0.7
Abbreviations: CI, cardioinhibitory; FMD, flow-mediated vasodilation; NMD, nitrate-mediated dilation; VD, vasodepressive.aP < 0.05.
11.6± 3.6 minutes after drug administration, classified as VD in 5 cases, CI in 4, and mixed in 2.
The ultrasound assessment of the endothelial function showed resting values of brachial artery diameter lower in syncope patients than in controls (3.4± 0.6 vs 4.0 ± 0.8 mm, P < 0.05); lower values of the brachial artery diameter were recorded in VD than in CI (3.0± 0.4 vs 3.8 ± 0.6 mm, P < 0.01) and mixed syncope (3.0± 0.4 vs 3.4 ± 0.1, P= ns); subjects with CI syncope had similar values of the brachial artery diameter compared to the controls (3.8± 0.6 vs 4.0± 0.8 mm, P = ns) (Table 1).
The FMD was within the normal range in NMS subjects, with poor and not significant differences compared to the controls (FMD= 10.2 ± 4.5 vs 11.4 ± 3.9, P = ns), as well as between patients with CI and VD syncope (10.3± 2.1 vs 11.3± 5.7, P = ns); the poorer FMD (5.7 ± 5.1) was recorded in the mixed NMS, and 1 of these subjects had increased low-density lipoprotein cholesterol with overt endothelial disfunction, characterized by an FMD <5%.
In the subjects with NMS, the normal FMD values were paired to a poor increase of the recovery time after reactive hyperemia, compared to controls (4.1± 2.5 vs 3.3 ± 0.7 minutes, P= ns) (Table 1).
The endothelial independent vasodilation, assessed with the NMD, was significantly higher in fainting subjects than in controls (26.7± 7.3 vs 19.0 ± 3.6, P < 0.05), with a higher vasodilation in VD patients than in CI (31.1± 7.0 vs 23.1± 5.0, P = ns), as well as in VD vs mixed NMS (31.1± 7.0 vs 20.4 ± 5.3, P < 0.05); furthermore, the NMS patients showed a long-lasting passive vasodilation after nitroglycerine administration, with higher recovery times that were significantly longer in NMD than in controls (13.0± 5.6 vs 6.3 ± 0.7 minutes, P < 0.05), irrespective of the VASIS classification (Table 1).
Statistical analysis showed a correlation between resting brachial artery diameter and age (r= 0.705, P < 0.01), but we did not find a correlation between age of the fainting patient and his or her FMD (r= 0.364, P = ns) or between FMD and NMD values (r= 0.049, P = ns).
We implanted a permanent dual-chamber pacemaker in 2 of the 3 subjects, who were both more than 40 years old, with a head-up tilt test positive for a VASIS-2B CI syncope, according the recommendations for the prevention of syncopal recurrences in highly symptomatic vasovagal fainters with a marked CI response during tilt-induced syncope.6 At the 2-year follow-up, both of them were free
from new episodes of syncope and reported improvement
in quality of life. The other 15 patients followed a usual conservative treatment; the 2-year follow-up was obtained in 11 patients, and 3 of these reported a recurrence of syncope, without other significant cardiovascular events; the other 4 patients were lost to follow-up, including the women with an impaired response to the FMD.
Discussion
We found that the hallmark of patients with NMS is a marked and sustained endothelial-independent vasodilation, in the presence of a normal FMD; the vascular hyperreactivity that characterizes the response to the nitrate administration is particularly overt in subjects with a VD syncope and can partially explain the high rate of responses to the nitrate administration during the tilt test. Furthermore, all the syncopal subjects show a greater and longer than normal response to the nitrate administration, irrespective of the type of tilt-induced events, stated according to the VASIS classification, and unrelated to the basal brachial artery diameter, age, and levels of the FMD; we found an abnormal FMD, indicative for endothelial dysfunction, only in 1 hypercholesterolemic women, with a head-up tilt test positive for a mixed syncope.
The head-up tilt test is currently used to induce the syncope, allowing the identification of the pathophysiologic underlying mechanism. The syncope represents the diagnostic end point of the tilt test, but it may not always be induced by the drug-free test; to increase the sensitivity of this test, current protocols recommend pharmacologic stimulation with nitroglycerine or isoproterenol.17 – 19
The cardiovascular response observed during this provocative test is characterized by the presence of a marked hypotension, typical of these patients, spontaneously occurring and amplified by nitroglycerine administration, which could be similar to the ultrasound pattern found at the evaluation of the endothelial dysfunction.12,13
We found that the nitrate administration induced in all patients a higher endothelium-independent vasodilation, regardless of the type of neuromediated syncope induced by the tilt test; the vascular response to the nitrate admin-istration was more pronounced, but without any statistically significant difference, in subjects with VD syncope.
Our patients showed a marked hypersensitivity to the sublingual nitrate administration that seems to be typical of these subjects and is further expressed by a longstand-ing endothelial-independent vasodilation, with prolonged
Clin. Cardiol. 35, 2, 107–110 (2012)
109
L. Santini et al: Endothelial function in NMS Published online in Wiley Online Library (wileyonlinelibrary.com) DOI:10.1002/clc.20990 2011 Wiley Periodicals, Inc.recovery time compared to the controls and without any correlation with the VD or CI mechanism observed at the head-up tilt test.
The deep vasodilator response to the nitrate administra-tion, reported to occur in skeletal muscle district during the vasovagal syncope, seems to be typical of the NMS and likely is a dose-independent phenomenon20,21; this phenomenon
indeed seems to suggest an abnormal vascular reactivity that could explain the poor efficacy of the pharmacologic therapy in this setting of patients. All the drugs tested, even using several targets to counteract the reflex response or to enhance the vasoconstriction, were usually reported to be poorly effective.1,2,22,23
The lower basal values of brachial artery diameter recorded in the subjects with a VD syncope seem to be due to the prevalence of young women, as compared to those patients with a CI syncope15,24; moreover, we cannot
exclude the possibility that some of our patients have a marked vasoconstrictive tone at rest, followed by a deep vasodilation after the nitrate administration.
The finding of nitrate overactivity, recorded in most of the fainting subjects, may also suggest the possible action of some still poorly assessed nitrergic mechanisms in the pathogenic pathway of NMS, with complex and poorly known interactions between the endothelial function and the autonomic nervous system.25 – 27
Conclusion
The evaluation of endothelial function supports evidence that the NMS is characterized by a marked and sustained endothelial-independent vasodilation, in the presence of a normal FMD; the vascular hyperreactivity in response to the nitrate administration is particularly overt in the VD syncope and can explain the high rate of responses to the nitrate administration during the head-up tilt test. The small number of observed patients does not allow to draw a conclusion regarding the role of the endothelial-dependent and independent vasodilation in the NMS. Further studies, involving a greater number of patients, will clarify if an overt peripheral vascular hyperreactivity to the nitrate administration could be used as a marker to detect patients likely to experience an NMS but unable or not capable to perform the head-up tilt test, so that the evaluation of the endothelial function could be used also to integrate the noninvasive diagnostic procedures.
References
1. Grubb BP. Neurocardiogenic syncope. N Eng J Med. 2005;352: 1004–1010.
2. Kapoor WN. Syncope. N Eng J Med. 2000;343:1856–1862. 3. Mosqueda-Garcia R, Furlan R, Tank J, et al. The elusive
patho-physiology of neurally mediated syncope. Circulation. 2000;102: 2898–2906.
4. Benditt DG. Neurally mediated syncopal syndromes: pathophysio-logical concepts and clinical evaluation. Pacing Clin Electrophysiol. 1997;20:572–584.
5. Ammirati F, Colivicchi, F, Santini M, et al. Permanent cardiac pacing versus medical treatment for the prevention of recurrent vasovagal syncope: a multicenter, randomized, controlled trial. Circulation.2000;104:52–57.
6. Task Force for the Diagnosis and Management of Syncope; European Society of Cardiology (ESC); European Heart Rhythm
Association (EHRA); Heart Failure Association (HFA); Heart Rhythm Society (HRS); Moya A, Sutton R, Ammirati F, et al. Guidelines for the diagnosis and management of syncope. Eur Heart J.2009;30:2631–2671.
7. Chen LY, Benditt DG, Shen W. Management of syncope in adults: an update. Mayo Clin Proc. 2008;83:1280–1293.
8. Sneddon J, Couniham P, Bashir Y, et al. Impaired immediate vasoconstrictor responses in patients with recurrent neurally mediated syncope. Am J Cardiol. 1993;71:72–76.
9. Lewis WR, Smith ML, Carlson MD. Peripheral sympathoinhibition precedes hypotension and bradycardia during neurally medi-ated vasovagal syncope (Abstract). Pacing Clin Electrophysiol. 1994;17:II–747 (Abstract).
10. Ziegler MG, Echon P, Wilner KD. Sympathetic nervous with-drawal in the vasodepressor (vasovagal) reaction. J Auton Nerv System.1986;17:273–278.
11. Sra JS, Murthy V, Natale A, et al. Circulatory and catecholamine changes during head-up tilt testing in neurocardiogenic (vasova-gal) syncope. Am J Cardiol. 1994;73:33–37.
12. Takase B, Akima T, Uehata A, et al. Endothelial function and peripheral vasomotion in the brachial artery in neurally mediated syncope. Clin Cardiol. 2000;23:820–824.
13. Galetta F, Franzoni F, Plantinga Y, et al. Endothelial function in young subjects with vaso-vagal syncope. Biomed Pharmacother. 2006;60:448–452.
14. Widlansky ME, Gokce N, Keaney JF Jr, et al. The Clinical Implication of Endothelial Dysfunction. J Am Coll Cardiol. 2003;42:1149–1160.
15. Corretti MC, Anderson TJ, Benjamin EJ, et al; International Brachial Artery Reactivity Task Force. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002; 39:257–265.
16. Brignole M, Menozzi C, Del Rosso A, et al. New classification of haemodynamics of vasovagal syncope: beyond the VASIS classification. Europace. 2000;2:66–76.
17. Ammirati F, Colivicchi F, Biffi A, et al. Head-up tilt testing with low-dose sublingual isosorbide dinitrate; a simplified time-saving approach for the evaluation of unexplained syncope. Am Heart J. 1998;135:671–676.
18. Fitzpatrick AP, Theodorakis G, Vardas P, et al. Methodology of head-up tilt testing in unexplained syncope. J Am Coll Cardiol. 1991;17:125–130.
19. Bartoletti A, Alboni P, Ammirati F, et al. ‘The Italian Protocol’: a simplified head-up tilt testing potentiated with oral nitroglyc-erin to assess patients with unexplained syncope. Europace. 2000;2:339–342.
20. Timoteo AT, Olivera M, Feliciano J, et al. Head-up tilt testing with different nitroglycerin dosages: experience in elderly patients with unexplained syncope. Europace. 2008;10:1091–1094.
21. Almquist A, Goldenberg IF, Milstein S, et al. Provocation of bradycardia and hypotension by isoproterenol and upright posture in patients with unexplained syncope. N Engl J Med. 1989;320:346–351.
22. Dendi R, Goldstein DS. Meta-analysis of nonselective versus beta-1 adrenoceptor-selective blockade in prevention of tilt-induced neurocardiogenic syncope. Am J Cardiol. 2002;89: 1319–1321.
23. Schroeder C, Birkenfeld AL, Mayer AF, et al. Norepinephrine transporter inhibition prevents tilt-induced pre-syncope. J Am Coll Cardiol.2006;48:516–522.
24. Moe I, Hoven H, Hetland E, et al. Endothelial function in highly endurance-trained and sedentary, healthy young women. Vasc Med.2005;10:97–102.
25. Dietz NM, Engelke KA, Samuel TT, et al. Evidence for nitric oxide mediated sympathetic forearm vasodilatation in humans. J Physiol. 1997;498:531–540.
26. Lepori M, Sartori C, Duplain H, et al. Interaction between cholin-ergic and nitrcholin-ergic vasodilation: a novel mechanism of blood pressure control. Cardiovasc Res. 2001;51:767–772.
27. Ruiz A, Sinigaglia S, Hermes R, et al. Role of nitric oxide in young patients with vasovagal syncope. Europace. 2010;12:987–990.
110
Clin. Cardiol. 35, 2, 107–110 (2012) L. Santini et al: Endothelial function in NMSPublished online in Wiley Online Library (wileyonlinelibrary.com) DOI:10.1002/clc.20990 2011 Wiley Periodicals, Inc.