Clinical
Paper
Trauma
Intraoral
extra-mucosal
fixation
of
fractures
in
the
atrophic
edentulous
mandible
A. Benech,M. Nicolotti,M. Brucoli,F. Arcuri:Intraoralextra-mucosalfixationof fracturesintheatrophicedentulousmandible.Int.J.OralMaxillofac.Surg.2013;42: 460–463.#2012InternationalAssociationofOralandMaxillofacialSurgeons. PublishedbyElsevierLtd.Allrightsreserved.
A.Benech,M.Nicolotti,M.Brucoli, F.Arcuri
A.O.U.MaggioredellaCarita`,Universityof EasternPiedmont,Novara,Italy
Abstract. Atrophyofthemandibleleadstoadecreaseinthebonemass,makingit morevulnerabletofractures.Adirectrelationshiphasbeendemonstratedbetween theheightoftheboneintheareaofthefractureandtheincidenceofpostoperative complicationsofbonehealing.Basicprinciplesoffracturemanagementinboth edentulousandnonedentulouspatientsareopenreductionandinternalfixationwith osteosynthesisofthefracturetoachieverestorationintermsofaestheticsand functionality.Severalauthorshavediscussedtheadvantagesanddisadvantagesof thetransoralandextraoralapproaches.BetweenJanuary2007andJune2011,13 patientsaffectedbybilateralfracturesofatrophicmandiblesweretreatedby extra-mucosalintraoralstabilizationwithsatisfactoryresults.Thisapproachreducesthe risksofdamageofthemarginalismandibulaenervewithlowoperationtime,while avoidingunsightlyscars.
Key words: extramucosal osteosynthesis; mandibularfracture;atrophicedentulous mand-ible.
Acceptedforpublication13November2012 Availableonline24January2013
Atrophy of the mandible leads to a decreaseinthebonemass,makingitmore vulnerabletofractures.Maxillaryatrophy can be considered as the end stage of edentulism (total teeth loss). Treatment of fractures in old patients with bone atrophyarecharacterizedbyhigh morbid-ity due to local and general factors. A directrelationship between theheightof theboneintheareaofthefractureandthe incidence ofpostoperativecomplications ofbonehealinghasbeendemonstrated.1
Themostcommonsiteoffractureinthe edentulous mandibles is the mandibular body.Fibrousunionornonunionoccurs most frequently at this site, especially whentheamountoftheresidualmandible
is less than 20mm (particularly <10mm).2
Basic principles of fracture manage-mentinbothedentulousandnon edentu-lous patients are open reduction and internal fixation with osteosynthesis of thefracturetoachieverestorationinterms of aesthetics and functionality. Several authors have discussed the advantages and disadvantages of the transoral and extraoralapproaches.Thepurposeofthis study was to introduce the authors’ approachtofracturesoccurringinatrophic mandibles. Theirpreoperativehypothesis was that extra-mucosal intraoral osteo-synthesiscanachieveadequate mandibu-lar restorationintermsofaesthetics and
functionality. The specific aims were to review the surgical outcomes of this approach.
Materialsandmethods
Acase series study was designed anda sampleofpatientsaffectedbyfracturesof theatrophicmandiblewasenrolled. Inclu-sion criteria were bilateral fracture of atrophic mandibular body, edentulism, andboneheightlessthan20mm.Patients wereexcludediftheyhadpreviously trea-tedoruntreatedmandibularfractures.
Causesoffracturesincludedaccidental fallsinsixcases;threepatientshadfallen tothe ground after a syncope; and four Int.J.OralMaxillofac.Surg.2013;42:460–463
http://dx.doi.org/10.1016/j.ijom.2012.11.013,availableonlineathttp://www.sciencedirect.com
patients had been involved in a motor vehicle accident. Two patients had no associated systemic comorbidities, eight hadhypertension,twohaddiabetes asso-ciatedwithhypertension,andonepatient reportedhypertensionandaprevious tran-sient ischaemic attack. Despite these comorbidities, all patients were able to undergogeneralanaesthesia(Table1).
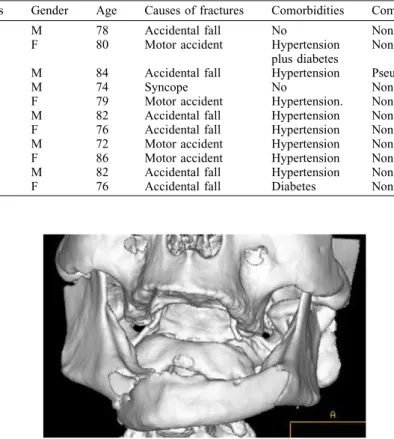
Allpatientshadedentulousandatrophic mandibles. The maximum height ofthe mandibularbody,measuredoncomputed tomography(CT)scanslides,was16mm. The average height was 11.5mm (min 8.5mm; max14mm)atthesite of frac-ture.Thetimeofsurgicaltreatmentafter injury rangedfrom 1to6 days,withan averagetimeof3.5days. Orthopantomo-graphywasthefirstleveldiagnostic ima-ging technique. The second level investigation was a mandibularCT scan toanalysethedegreeoffracture displace-mentandtheheightoftheatrophicbody (Fig.1).
Patients who underwent surgery were dischargedfromthemaxillofacial depart-mentonthesecondpostoperativedaywith 6 days’ antibiotic therapy (amoxicillin 875mg plus clavulanic acid 125mg) twiceadayandpainmedicationifneeded. Duringthepostoperativefollow-up,which lasted 40days ormore, the patient was checked onceaweek.8weeksafter sur-gery the patients underwent orthopanto-mography to verify the stability of osteosynthesisaftertheformationof pri-mary callus.Once ithadbeenconfirmed that bony union had occurred, the plate was removed from each patient under localanaesthesia(optocain20mg/mlplus adrenalin1:100,000).
Surgicaltechnique
Theosteosynthesisproposedis basedon the application of a preformed extra-mucosalreconstruction plate.The opera-tionisperformedundergeneral anaesthe-sia following the usual procedure of induction.Thestepsoftheoperationare simple andeasily repeatable.Inthe first step,ashort(about3cm)bilateral muco-sal incision is performed, followed by subperiosteal dissection of the lateral aspectofthemandibularangles toallow insertionoftheendportionsofthe osteo-synthesisplatepreviouslymodelledonthe shapeofthemandibulararch.Theplateis fixed to the mandibular angles by one bicortical screw oneach side. Theplate usedbelongstoalockingsystem2mmin diameter(Fig.2).
Thesecondstepisthemanualreduction ofthefracturedbodyanditsstabilization.
Theaccuracyofthereductionisverified by intraoperativeradiography.If doubts remain, a small mucosal window can be produced to examine the alignment of bone fragments. Once the correct reduction is obtained, the bone frag-ments are locked to the plate by one or two transmucosal titanium screws at thesymphysisandtwoadditionalscrews at the mandibular angles (Fig. 3). The surgical incisions are sutured. The operative time usually ranges from 35 to 75min.
The removal of the plate is usually performed atpostoperative week9. Lat-eralscrewsareremovedwithanangulated screwdriveraftersubperiostealdissection alongtheterminalpartoftheplate. Ante-rior extramucosal screws are easily removed by the appropriate screwdriver (Fig.4aandb).
Results
13 patients (8males; 5 females) witha meanageof79years(range72–86years) Intraoralextra-mucosalfracturefixationinatrophicmandible 461
Table1. Characteristicsofthepatientswhounderwentextra-mucosalintraoralosteosynthesis.
Patients Gender Age Causesoffractures Comorbidities Complications
A.P. M 78 Accidentalfall No None
B.B. F 80 Motoraccident Hypertension
plusdiabetes
None
D.V. M 84 Accidentalfall Hypertension Pseudarthrosis
F.A. M 74 Syncope No None
B.F. F 79 Motoraccident Hypertension. None
B.C. M 82 Accidentalfall Hypertension None
C.N. F 76 Accidentalfall Hypertension None
L.P. M 72 Motoraccident Hypertension None
O.D. F 86 Motoraccident Hypertension None
G.Z M 82 Accidentalfall Hypertension None
D.U. F 76 Accidentalfall Diabetes None
Fig.1. CTscan.3Dreconstructionofadoublefractureinanatrophicmandible.
mettheinclusioncriteria.Theywere hos-pitalized inthemaxillofacial department of the Novara Major Hospital between January2007andJune2011.Twopatients didnotaccepttheproposedsurgical pro-tocol, so in both cases an extraoral approachwithinternalfixationwasused. 11 patients were treated surgically by extra-mucosalosteosynthesis.
One patient,initially treated by extra-mucosal fixation, was converted intoan extraoral approach. She developed a mycoticinfectionaroundtheplate, resis-tanttotherapywithfluconazole150mg/ dayandoralwashingwithnystatinthree timesadayfor14days.Mucosalburning and pain reported by the patient were
intolerable,sotheplatewasremoved dur-ing the fourth week after surgery. The patient continued antimycotic therapy and the symptoms regressed in 6 days. The early plate removal led to pseudar-throsis. Bilateral submandibular access wasperformedtoapplya2.0mmlocking reconstruction plate with satisfactory resultsintermsofaestheticsand function-ality.Shecomplainedofatransient reduc-tion of function of the right marginalis mandibulaenerve,butthisregressed spon-taneouslyin5months.
Three patients complained of perma-nentfooddebrisintheholesoftheplate and between the plate and the gingival mucosa.Intwocasestherewasamucosal
ulcerofthelipcorrespondingtotheupper edgeoftheplate.
Radiographyperformed 8 weeksafter surgeryshowedgoodalignmentwithbone consolidationinninecases.Inonepatient, bonyconsolidationafter8weekswasnot satisfactoryon the leftside.The patient was reassessed after 1 month and bony unionwasstable.Theremovaloftheplate wasperformedatweek9inninepatients. Inonecase(thecasepreviouslydescribed) it was removed at week 13. No major intraoperative surgical complications wereseeninanypatient.
Discussion
Physicians have described many techni-quesfortreatingmandibularfracturesbut onlyinthesecondhalfofthe20thcentury, followingthedevelopingofradiographic methods and surgical instruments, have theresultsoftreatmentbeenimproved.3
Thedevelopmentofopenreductionand rigid internal fixation has notled to the abandonmentoftheinitialideaofexternal fixation.Severalsurgeonsuseanexternal mandibularfixator following recommen-dations by Spiessl4 regarding infected pathological fractures, heavy comminu-tions, the emergency care ofopen frac-turesinpolytraumacases,andbridgingof defectsuntil secondaryreconstruction.
According to the literature, external fixatorsareneitheremployedinfractures ofnon-tooth-bearingsegments,norinthe edentulous and atrophic mandible. Until now,application ofexternalfixators has beenfocusedontranscutaneous systems. The authors’ aim is to introduce a less bulkyextra-mucosaldevice withan effi-cacy comparabletoan internal plate for atrophic/edentulousfracturedmandibles.
Load-bearing osteosynthesis is indi-catedinthetreatmentof atrophic/edentu-lous mandible fractures; currently the locking reconstruction plate is recom-mended.Theplatemust belongenough toplacescrewsinadequatebone.
When dealing withbilateral fractures, theplatemustspanfromangletoangle, covering the entire vestibularsurface of the mandible. At least three screws on eithersideofthemandible,attheangles, arerecommended5–7except for cases of severeatrophyinwhichtheriskofnerve damageandthepoorquantityandquality ofboneforcesthesurgeontoreducethe numberofthescrews(Fig.4a).
The platecovers the whole vestibular faceofthemandibular bodyandplaysa fundamentalroleinsharingthe biomecha-nicalmastication forces. In2011, Wood etal.,5describedeightpatientstreatedbya 462 Benechetal.
Fig.3. Intraoperativeviewshowingextramucosalfixationoftheplate.
Fig.4. (a)Radiographicimageofthefractures.(b)Radiographicimageofhealingafterremoval
transmucosalfixationoftheplateoverthe alveolarridge.Thetechniquedescribedin the present paper is based on the same principlesbutdiffersinthepositionofthe plate.Thevestibularcortexofthe mand-ible allows a more accurate and easier adaptationoftheplatewithbetter resolu-tionofthefractures.
Causes of delayed healing in treated fracturesoftheatrophic/edentulous mand-ible are multiple. There is lack of bone which is generallycortical witha lower healing potential. There are no teeth, whichhelptoreducethefractures.Often, the patients are elderly and medically compromised.Theauthorsthinkitis pos-sibletoreducedisplacedfractures ofthe edentulousmandiblebyclosed manipula-tionofthebonefragmentsinahigh per-centageofcases.
Insummary,the authorsconsider that the use of a 2.0mm locking system as extra-mucosalfixatorisagoodoptionfor thetreatmentoffracturedatrophic mand-ibles.Thissystem,originallydesignedas aninternalfixator,offersmechanicaland biologicaladvantages.It guarantees ade-quatestabilitywhilepreservingblood sup-plytothe boneandmucosa.Theoretical disadvantagesarecontaminationwith pos-sibleinfectionandanimperfectalignment ofthebonesegments.Serious complica-tions such as non-union or fracture of hardware have been widely reported in the standard management of atrophic mandiblefractureswithratesrangingfrom 4% to 20%.6 Theextra oralroute often causesanundesirablescar,andthe
possi-bilityofinjuringthemandibularbranchof the facial nerve is always present, asso-ciated withthepotentialcreationof sali-vary fistulas. This technique reduces operativetime, whileobtainingadequate fixation.Thisisimportantinpatientwith comorbidities who are not suitable for prolongedgeneralanaesthesia.
Inconclusion,thepatientstreatedwere satisfied,particularlywiththerapid posi-tioning and removal of the plate. They were also able to eat a soft diet with minimal discomfort immediately after surgery. Although the submandibular approach is still the gold standard for thetreatmentofatrophicmandibularbody fractures,itextendstheoperatingtimeand can increase surgical complications. For these reasons this peculiar approach to treat atrophic mandibular fractures can beavalidalternative. Funding None. Competinginterests Nonedeclared. Ethicalapproval Notrequired. References
1. Wittwer G, Adeyemo WL, Turbani D, PloderO.Treatmentofatrophicmandibular
fractures based on the degree of atrophy-experiencewithdifferentplatingsystems:a retrospectivestudy.J OralMaxillofacSurg 2006;64:230–4.
2. LuhrHG,ReidickT,MertenHA.Resultsof treatmentoffracturesoftheatrophic edentu-lousmandiblebycompressionplating:a ret-rospectiveevaluationof84consecutivecases. JOralMaxillofacSurg1996;54:250–4. 3. TomaVS,MathogRH,TomaRS,MelecaRJ.
Transoralversusextraoralreductionof mand-iblefractures:acomparisonofcomplication rates and other factors. Otolaryngol Head NeckSurg2003;128:215–9.
4. Spiessl B. A¨ ussere Schienung: fixateur externe.In:SpiesslB,editor.Osteosynthese desunterkiefers,manualderAOprinzipien. BerlinKap:Springer;1988.p.S67–92.4.2.2. 5. WoodGA,CampbellDF,GreeneLE. Trans-mucosalfixationofthefracturededentulous mandible. Int J Oral Maxillofac Surg 2011;40:549–52.
6. KunzC,HammerB,PreinJ.Fracturesofthe edentulousatrophicmandible:fracture man-agement and complications. Mund Kiefer Gesichtschir2001;5:227–32.
7. Bradley JC. Age changes in the vascular supply of the mandible. Br Dent J 1972; 132:142–4.
Address:
FrancescoArcuri
A.O.U.MaggioredellaCarita`
UniversityofEasternPiedmont
‘‘A. Avogadro’’ C.soMazzini18 28100Novara Italy Tel:+3903213733895 E-mail:[email protected]