C A S E R E P O R T
Acute onset of retinal detachment after posterior
chamber phakic intraocular lens implantation
Núria Planas Domènech Luís Arias Sergi Prades Octavi Pujol Marc Rubio Jose M Caminal Department of Ophthalmology, Hospital Universitari de Bellvitge, L’Hospitalet de Llobregat, Barcelona, Spain
Correspondence: Núria Planas Domènech Department of Ophthalmology, Hospital Universitari de Bellvitge. Feixa Llarga s/n 08907. L’Hospitalet de Llobregat, Barcelona, Spain
Tel +34 9 3260 7705 Fax +34 9 3260 7981 Email [email protected]
Case report: A 34-year-old man with severe myopia, presented with acute visual loss in his
right eye. This occurred 3 hours after a posterior chamber phakic (PCP) intraocular lens (IOL) implantation, and was associated with a rhegmatogenous retinal detachment. Retinal retachment surgery was performed without complications, with the outcome showing good anatomical and functional results during a 2-year follow-up period.
Discussion: Despite the fact that several authors have described retinal detachments following
PCP IOL implantation in highly myopic patients, there is no evidence that this procedure increases the risk of retinal detachment in these patients. The occurrence of the retinal detachment immediately after the phakic IOL implantation supports the hypothesis that the surgical procedure could induce iatrogenic changes in patients with high myopia, which could increase the incidence of retinal detachment. In contrast to other reports, the interval between the PCP IOL implantation and the retinal detachment was only 3 hours in our patient. We believe this demonstrates the importance of performing a complete preoperative vitreoretinal examination in patients with severe myopia.
Keywords: retinal detachment, phakic intraocular lens, myopia
Introduction
Myopic eyes have a higher incidence of retinal complications compared with emmetropic eyes (Ruiz-Moreno et al 2003; Martínez-Castillo et al 2005). Surgical treatment of high myopia includes; clear lens extraction with intraocular lens (IOL) implantation, anterior or posterior chamber phakic (PCP) IOL implantation, and corneal refractive techniques. We report the case of a retinal detachment after PCP IOL implantation.
Case report
A 34-year-old man with high myopia of -13 diopters (D) in both eyes, underwent a PCP IOL surgery model implantable contact lens (ICL) without complications in both eyes in a private clinical centre. He then presented to the emergency department of Hospital Universitari de Bellvitge with an acute visual loss in his right eye, 3 hours after the surgical procedure.
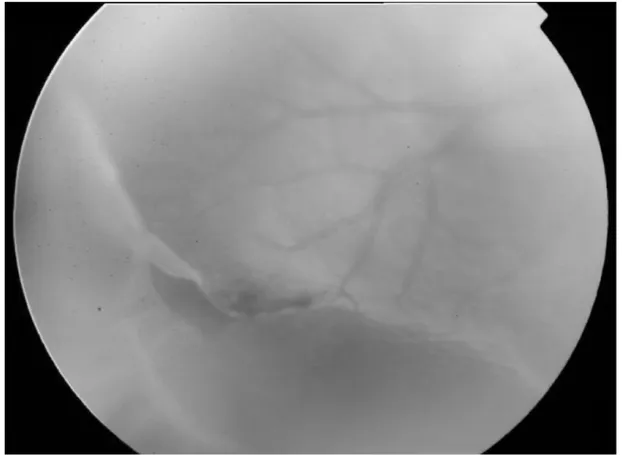
Ophthalmological examination revealed best corrected visual acuity (BCVA) of counting fi ngers at 1 meter in his right eye and 20/32 in his left eye. Anterior segment examination showed a PCP IOL correctly implanted, without any other relevant abnormality (Figure 1). The fundus examination of the right eye showed a retinal detachment from 4 o’clock to 10 o’clock with macula off (Figure 2A), and an equatorial tractional retinal tear located at 9 o’clock next to a lattice degeneration (Figure 2B), without proliferative vitreoretinopathy.
A corrective surgical operation was performed, under retrobulbar anesthesia and sedation, consisting of an encircling band in combination with a posterior vitrectomy.
The subretinal fl uid was drained through the retinal tear with the aid of perfl uorocarbon liquid. Endophotocoagulation was applied around the retinal tear and the vitreous cavity was fi lled with 20% SF6.
The patient was examined at 1 month, 3 months, 6 months, 12 months, and 24 months. In all the follow-up examinations the retina remained totally reattached with a BCVA of 20/50 at 24 months (Figure 3). No cataract forma-tion was noted at any of the follow-up examinaforma-tions.
Discussion
The incidence of retinal detachment in myopic eyes is higher than in emmetropic eyes (Ruiz-Moreno et al 2003; Martínez-Castillo et al 2005). High myopia is a risk factor for rhegmatogenous retinal detachment, generally because of premature vitreous liquefaction, posterior vitreous detachment, major axial length, and an increased prevalence of lattice degeneration (Martínez-Castillo et al 2005). The risk of retinal detachment in myopic eyes has been quoted between 0.71% and 3.2%. This percentage was
determined for myopia greater than -6 D, following research of 1000 myopic eyes (Ruiz-Moreno et al 2003; Martínez-Castillo et al 2005). However, it is unknown if phakic IOL implantation in patients with high myopia induces iatrogenic changes which could increase the incidence of retinal detachment (Ruiz-Moreno et al 2003, 2006; Martínez-Castillo et al 2005).
As mentioned before, in the case presented, the patient underwent the PCP IOL implantation, procedure with good visual results, and a low rate of short-term complications (Martínez-Castillo et al 2005).
A number of papers have studied the incidence and char-acteristics of retinal detachment in patients with high myopia corrected with anterior chamber phakic IOL implantation. However, only a few authors have described cases of retinal detachment in patients with severe myopia corrected with PCP IOL implantation.
Panozzo and Parolini (2001) described four cases of retinal detachment after PCP IOL implantation, and Zaldivar and colleagues (1998) reported one case of retinal Figure 1 Anterior segment photograph showing a posterior chamber phakic intraocular lens implantation.
Retinal detachment in high myopia
Figure 2A Fundus photograph showing a retinal detachment involving the macula.
detachment among 124 PCP IOL implantations, followed up for 11 months after surgery.
The retrospective study of Martínez-Castillo and col-leagues (2005) shows an incidence of retinal detachment of 2.7%, with a mean follow-up of 64.3 ± 10.35 months after PCP IOL implantation. Retinal detachment occurred from 1 to 70 months after PCP IOL implantation and 68.75% of retinal detachments had only one causative break. In the eyes where previous laser photocoagulation had been performed because of the presence of lattice degeneration, retinal tear or retinal hole in the preoperative exam, causative breaks for retinal detachment appeared at new sites and were unrelated to previously treated lesions. The surgical management of retinal detachments with scleral buckling and pars plana vitrectomy was effective. The authors concluded that PCP IOL implantation for surgical correction of severe myopia did not seem to increase the risk of retinal detachment in these patients.
It is, however, concluded that early surgical intervention for the retinal detachment is an important factor for a good visual and anatomical prognosis.
As the patient of this case presented and was operated on in a private centre, we did not know whether he presented with any break in the lattice degeneration, which had not been photocoagulated before the PCP IOL implantation. However, the patient did not report any symptoms of fl oaters or photopsia prior to the refractive procedure. Another aspect we considered is the controversy that exists between different authors regarding the need for prophylactic photocoagulation on predisposing lesions before the refractive procedure.
We are therefore suggesting that the occurrence of the retinal detachment immediately after the phakic IOL implantation supports the hypothesis that the surgical procedure could induce iatrogenic changes in patients with high myopia, which could increase the incidence of retinal Figure 3 Fundus photograph showing a total retinal reattachment at the 24-month follow-up.
Retinal detachment in high myopia detachment. PCP IOL implantation may also induce changes
in the vitreous and therefore increase traction on the retina. In summary, noting a contrast to other reports, and because the interval between the PCP IOL implantation and the retinal detachment, for our patient, was only 3 hours, we believe this demonstrates the importance of performing a complete vitreoretinal examination before refractive surgery in patients with severe myopia.
References
Martínez-Castillo V, Boixadera A, Verdugo A, et al. 2005. Rhegmatog-enous retinal detachment in phakic eyes after posterior chamber phakic intraocular lens implantation for severe myopia. Ophthalmology, 112:580–5.
Ruiz-Moreno JM, Alio JL. 2003. Incidence of retinal disease following refractive surgery in 9,239 eyes. J Refract Surg, 19:534–47.
Ruiz-Moreno JM, Montero JA, de la Vega C, et al. 2006. Retinal detachment in myopic eyes after phakic intraocular lens implantation. J Refract
Surg, 22:247–52.
Panozzo G, Parolini B. 2001. Relationships between vitreoretinal and refractive surgery. Ophthalmology, 108:1663–8.
Zaldivar R, Davidorf JM, Oscherow S. 1998. Posterior chamber phakic intraocular lens for myopia of -8 to -19 diopters. JRefract Surg, 14:294–305.