Arch Orthop Trauma Surg ( 1988) 107: 20-26 Archives of Orthopaedicand Traumatic Surgery © Springer-Verlag 1988
The Role of Macrophages and Giant Cells in Loosening
of Joint Replacement
U E Pazzaglia 1 and J A S Pringle 2
t Clinica Ortopedica dell'Universita di Pavia, IRCCS Policlinico San Matteo, Via Taramelli, 27100 Pavia, Italy
2 Morbid Anatomy Department, Institute of Orthopaedics, London University, Brockley Hill, Stanmore, Middlesex HA 7 4 LP, United Kingdom
Summary Macrophages and foreign-body giant cells
from the bone-cement interface of loosened joint re-placement were assayed for direct bone resorption in an in vitro experimental model Human osteoclasts from giant cell tumors and experimental animal os-teoclasts were used as controls Macrophages and giant cells were not capable of resorbing the bone under experimental conditions, but osteoclasts are It is suggested that macrophages and giant cells in loosened implants may initiate bone resorption, re-moving the extra-cellular barrier that normally pro-tects mineral crystals from osteoclastic recognition.
Zusammenfassung Makrophagen und Fremdk 6
rper-riesenzellen von der Knochen/Zementgrenze gelok-kerter Gelenkendoprothesen wurden hinsichtlich der direkten Knochenresorption in einem experimentel-len in vitro-Modell untersucht Als Kontrolexperimentel-len dien-ten Osteoklasdien-ten aus menschlichen Riesenzelltumo-ren und von embryonalen Hiihnerknochen WihRiesenzelltumo-rend Osteoklasten unter den experimentellen Bedin-gungen Knochen resorbierten waren Makrophagen und Riesenzellen dazu nicht in der Lage Es wird angenommen, da 13 Makrophagen und Riesenzellen bei gelockerten Implantaten die Knochenresorption anbahnen, indem sie die extrazellulare Barriere ent-fernen, welche normalerweise die Mineralkristalle dagegen schiitzen von den Osteoklasten als solche er-kannt zu werden.
Loosening of the prosthetic components in total joint replacements is generally recognized as a major com-plication, threatening the long-term results of the im-plant.
Offprint requests to: U E Pazzaglia
Different explanations of loosening have been presented in the past ten years; these include mechanical failure for unequal distribution of stresses at the bone-cement interface; changes of the blood supply pattern to the bone following medullary ream-ing and insertion of bone cement and prosthetic com-ponents l 26 l; foreign body reaction to particulate from prostheses materials l 29, 30 l; allergic reaction to soluble ions released from prosthetic components l 23, 27 l; and development of a synovial-like mem-brane at the bone-cement interface l 13 l.
One or more of these may be implicated in each individual case of loosening; in addition other factors as yet unidentified may also play a part Besides more of these factors cannot be excluded to be operating contemporaneously or successively What-ever the etiology may be, all cases of loosening share a common aspect, namely the loss of bone stock around the implant.
There is a general agreement about the statement that bone resorption in vivo is a cell-mediated pro-cess and osteoclasts are the cells specifically commit-ted.
There is now also a large body of evidence in favour of the view that osteoclasts are derived from a marrow stem cell l 1-3, 11, 14, 19, 21, 28 l and mono-nuclear histiocytes are the more likely candidate. Moreover macrophages have been reported to be capable of resorbing bone l 22, 24 l.
Because around loosened prostheses mac-rophages are observed in significant numbers follow-ing the production of foreign body particles or in the synovial-like membrane and they are found in the critical site, namely at the bone-cement interface, we have assayed the capacity of these cells to resorb di-rectly the bone in an experimental system which has been proved to be effective in testing osteoclastic ac-tivity l 8, 20 l.
Material and Methods
Tissue specimens were obtained from 5 patients who under-went revision surgery of total joint replacement Data regard-ing the patients included in the study are summarized in Table 1 Operation was required because of pain and radiographic evidences of bone stock loss around the implant In one case the entire proximal end of the femur was resected and avail-able for the study.
Infection was excluded by intraoperative aerobic and anaerobic cultures and by histological evaluation of the
speci-mens Soft tissue from the bone-cement interface was proces-sed for routine histology, embedded in paraffin and sections stained with haematoxylin-eosin.
Specimens of the same tissue were placed in HEPES buf-fered medium 199 (Flow) and stored at 4 °C and utilized for tis-sue culture within 3 hours from the excision.
Each specimen was cut in small fragments and scraped with a scalpel blade in Eagle minimum essential medium phosphate free; the medium was then throughly agitated using a glass pipette, aspirated and transferred to 30 mm Petri dishes (Nunc), where 200 glm thick bone slices or glass coverslips were
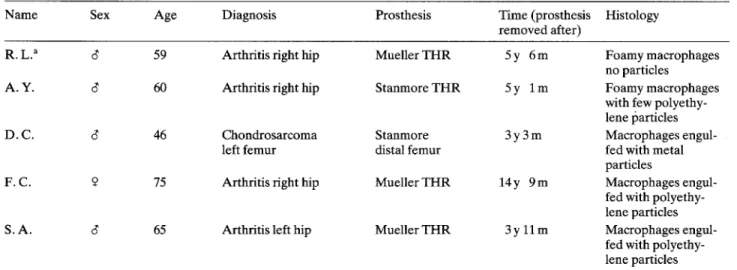
Table 1 Clinical and histopathological data of the patients included in the study
Name Sex Age Diagnosis Prosthesis Time (prosthesis Histology
removed after)
R L a 6 59 Arthritis right hip Mueller THR 5 y 6 m Foamy macrophages no particles
A Y 6 60 Arthritis right hip Stanmore THR 5 y 1 m Foamy macrophages
with few polyethy-lene particles
D C 6 46 Chondrosarcoma Stanmore 3 y 3 m Macrophages
engul-left femur distal femur fed with metal
particles
F C 9 75 Arthritis right hip Mueller THR 14 y 9 m Macrophages engul-fed with polyethy-lene particles
S A 6 65 Arthritis left hip Mueller THR 3 y 11 m Macrophages
engul-fed with polyethy-lene particles a The entire proximal femur was available for the study
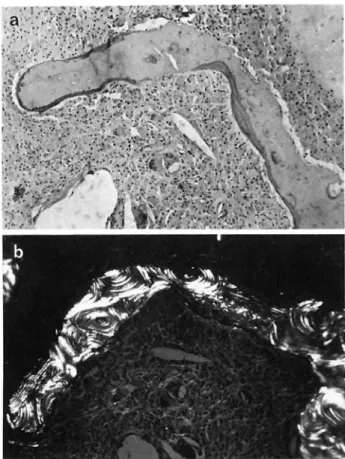
Fig 1 a 2 5 x Radiography of a
transverse section of the proximal femur (R L ) A thick membrane is interposed between the bone and the cement, which has been removed Radiopaque calcium deposits are evident inside the membrane b Acellular material of the membrane, with red cells and calcium crystals deposition in the right bottom corner HE, x 75 c Older foci of calcification surrounded by macrophages A sheet of red cells is present be-tween macrophages HE, x 75
U E Pazzaglia and J A S Pringle: The Role of Macrophages and Giant Cells lying on the bottom Bone slices were prepared from human
femoral cortical bone as described by Chambers et al l 8 l. Petri dishes were incubated for 30 ' at 37 C in an CO 2 in-cubator; then bone slices and coverslips were throughly washed in fresh medium and placed in new Petri dishes con-taining Eagle essential minimum phosphate-free medium (Flow), supplemented with 100 units of penicillin and 100 micrograms of streptomycin (Gibco) for milliliter and 10 per cent fetal calf serum (Gibco).
They were incubated at 37 °C in CO 2 incubator from 5 hours to 7 days Glass coverslips were observed directly in an inverted phase contrast microscope Bone slices were fixed in 2.5 per cent glutaraldehyde in 0 2 cacodilate buffer for 30 ' or placed in Triton X-100 ( 0 1 per cent in distilled water) for 12 hours before glutaraldehyde fixation The slices were then de-hydrated through a gradual ethanol series, critical point dried in C 02, coated with gold palladium by a sputter-coating and examined with a scanning electron microscope (JEOL JSM 35 C) Osteoclasts obtained from human giant cell tumors and from chicken embryos bones were used as controls.
Observations
Histology
A topographic study of the tissue was not possible in that cases where the specimens were curetted from the bone-cement interface on the femoral and acetabular side.
In these specimens histological examination con-firmed the presence of an amorphous and acellular material and of a loose connective tissue, containing numerous macrophages and foreign body giant cells. The histological findings of each case are summarized in Table 1.
Serial sections, comprising the cortical bone and the bone-cement interface membrane, were obtained from the case where the entire proximal femur was resected (Fig 1 a) These will be described in detail.
A marked zonal distribution of various types of tissue was not recognizable; around the cement pre-vailed a connective tissue with various degree of den-sity and thickness of the collagen fibers Scattered areas of an amorphous material and sheet of red cells were also present in the inner part of the connective membrane interposed between the cement and the cortical bone Fragments of necrotic bone and foci of calcification were often observed in this tissue (Fig lb) Aggregates of mononuclear cells with a foamy cytoplasm were occasionally observed be-tween the collagen fibers in this compartment of the membrane (Fig 1 c), while the same cells formed a dense and continous mass in the outer part in contact with the bone The cells here were larger, densely sti-pated, with the same clear and foamy cytoplasm and often multinuclear giant cells were present No bire-fringent polyethylene particles nor opaque metal par-ticles were observed in this case.
Fig 2 a Sheets of macrophages and giant cells near the cortical
bone, which is undergoing resorption HE, x 75 b The same field in polarized light
Fig 3 Macrophages invading the haversian canals of the
corti-cal bone HE, x 100
The bone surface presented with a continous line of resorption pits, interrupting irregularly the osteon lamellar pattern of the cortex (Fig 2) Many osteo-clasts were observed inside their resorption lacunae, while other pits on the same surface were empty; this pattern suggests that bone resorption is carried out
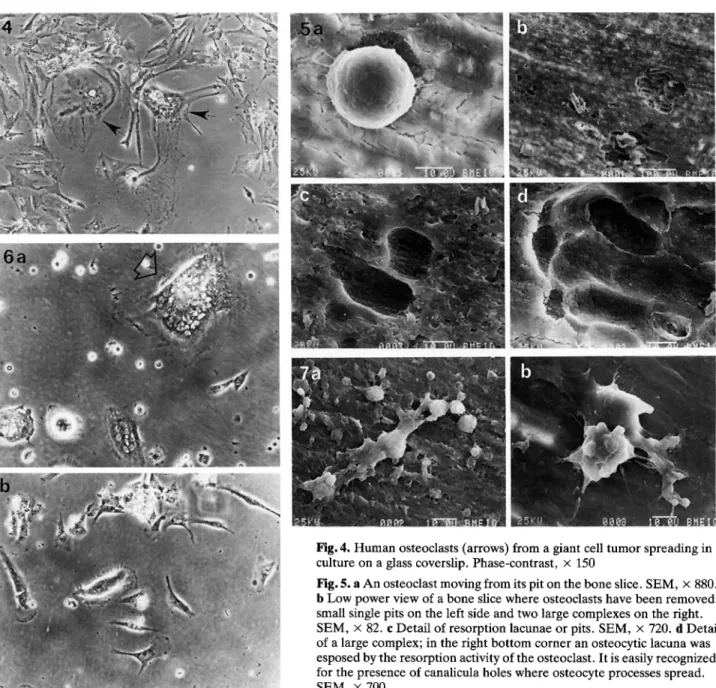
Fig 4 Human osteoclasts (arrows) from a giant cell tumor spreading in culture on a glass coverslip Phase-contrast, x 150
Fig 5 a An osteoclast moving from its pit on the bone slice SEM, x 880.
b Low power view of a bone slice where osteoclasts have been removed: small single pits on the left side and two large complexes on the right. SEM, x 82 c Detail of resorption lacunae or pits SEM, x 720 d Detail of a large complex; in the right bottom corner an osteocytic lacuna was esposed by the resorption activity of the osteoclast It is easily recognized for the presence of canalicula holes where osteocyte processes spread. SEM, x 700
Fig 6 a, b Multinuclear giant cells, macrophages and fibroblasts spreading in culture on a glass coverslip A polyethylene fiber is
present inside the large multinuclear giant cell (arrow) Phase contrast, x 150
Fig 7 a A giant cell spreading on bone slice; the larger globose cells observed nearby are macrophages, the smaller fibroblasts.
SEM, x 570 b A giant cell with the characteristic lobulated dome No sign of erosion or pit is evident beneath it SEM, x 600
discontinously by osteoclasts and corresponds to that observed by Chambers et al l 8 l.
The sheet of foamy cells filled all the crevices of the bone and invaded the haversian canals in the inner part of the cortex (Fig 3).
Cell Culture
Osteoclasts, which are allowed to settle on a sub-strate, adhere to it and spread their cytoplasmatic processes (Fig 4) When they are observed on the
bone slices by SEM they are easily recognized by means of their large size and characteristic shape, with the centre of the body raised as a central dome and flattened pseudopods extending peripherically. The margin of the cell shows thin filopodia which project on the underlying bone surface As soon as after 6 hours osteoclasts are observed to move on the bone surface and it is possible to observe, beneath the cytoplasmatic processes of the cell, the border of a pit, where bundles of fibrillar material are evident in contrast with the smooth appearence of the
rounding bone surface (Fig 5 a) When osteoclasts are removed (treating the bone slices with Triton X-100 before fixation) the surface of the slices presents rounded or oval excavations or pits, whose base is formed by a network of anastomosing and branching bundles of collagen fibrils (Fig 5 b, c) The character-istic features of pits do not allow them to be confused with vascular channels or osteocytic lacunae exposed by the saw in preparing bone slices (Fig 5 d) When osteoclasts are incubated for a longer time the pits do not become larger, but many more pits are formed, often clustered togheter to form complexes
(Fig 5 b, d).
An heterogenous population of cells was obtained from the tissue around implants (Fig 6 a, b); if ob-served in phase contrast on glass coverslips three classes of cells adehered to the substrate:
1 small, mononuclear cells, which spread with one or two thin dendritic processes at opposite poles, giv-ing to the cell a fusiform shape and easily recogniza-ble as fibroblasts
2 larger mononuclear cells (about 20 p ), which spread on the substrate with multiple dendritic pro-cesses all around the cell circumference, giving a globose or stellate appearence when processes are thin These cells were identified as mononuclear his-tiocytes or macrophages
3 very large, (about 200 i), multinuclear giant cells, which spread on the substrate assuming a globose shape or sometime a more irregular stellate or elon-gated shape, with thin filaments or pseudopods pro-jecting from the cell border Birefringent polyethyl-ene fibers were occasionally observed inside the cyto-plasm of these multinucleated giant cells, confirming that they were foreign body giant cells with ingested polyethylene particles (Fig 6 a).
When bone slices were observed with SEM the same three classes of cells were identified by means of their size and shape (Fig 7 a) Foreign body giant cells were in the same size range of osteoclasts, with a lobulated central dome and cytoplasmatic processes spreading around on the bone surface.
No sign of erosion or pit was evident beneath them (Fig 7 b) Bone resorption was neither associ-ated with macrophages or fibroblasts.
Bone slices cultured up to 7 days and pre-treated with Triton X-100 to remove the cells failed to show
any resorption lacunae.
Discussion
All the histological studies of bone-cement interface in loosened prostheses report significative numbers
of macrophages and giant cells in the tissue between the bone and the cement l 9, 10, 12, 16 l When bire-fringent polyethylene or opaque metal particles are found in quantity in the cells cytoplasm there is little doubt about the nature of the stimulus eliciting the macrophagic reaction This is more difficult to ascer-tain when a sheet of macrophages with a foamy cyto-plasm is present, but no particles are observed inside the cell.
Several hypothesis in this case are possible: release of substances which are not observed either with the light and the electron microscopy; these in-clude monomer or barium from the cement and solu-ble ions from the alloy of the stem;
organic material as products of cell death; in this case the amorphous or caseous material constantly ob-served around loosened implants;
bacteria, although this hypothesis is not supported by bacteriological and histological data in many of the cases reported.
Whatever the stimulus to excite the macrophages, they are found in large amount lining the bone sur-face and invading the medullary spaces and haversian canals in the cortex, but they, as well as the foreign body giant cells, are unable to resorb the bone under experimental conditions in which osteoclasts are cap-able of doing so.
The same results were obtained by Chambers and Horton l 7 l with mouse peritoneal macrophages and inflammatory polykaryos Moreover it has been re-cently observed that macrophages own cell surface receptors and antigens different from osteoclasts l 4, 17, 18 l and that they do not respond to hormonal stimuli as osteoclasts do l 7 l.
These observations support the hypothesis that osteoclasts are derived from a marrow stem cell dif-ferent from that which gives origin to macrophages or that the pattern of differentiation is established early on so they are not sharing antigen markers Our re-sults point out that mature macrophages cannot turn into osteoclasts.
Two different population of cells are therefore present around the bone which undergoes resorption in loosened prostheses: one formed by mononuclear histiocytes and foreign body giant cells, specialized in phagocytosis; the other comprising osteoclasts com-mitted to bone resorption l 15 l The aspect of mono-nuclear cells occasionally observed to resorb the bone l 25 l should be regarded as mature mononuclear osteoclasts.
The number of osteoclasts in periprosthetic bone far excedes that observed in normal bone turn-over
and it resembles that observed for example in primary hyperparathyroidism.
But still more striking is the quantity of macro-phages invading the vascular spaces of the bone It is possible therefore to assume that the macrophages play an important role in initiating the process, but that the active resorption is carried out exclusively by osteoclasts.
It has been observed in the 'in vitro' model that osteoclasts do not resorb bone continuously, but they seem to move away when a pit of a certain size has been formed l 8 l Also 'in vivo' bone resorption is a process which is carried out discontinously, with al-ternating phases of resorption and apposition Dur-ing the growth the results of the two processes leads to the definitive form of mature bone It seems un-likely that remodelling of bone could be purely casual and some form of control of resorption and
apposi-tion should exist.
It is known that factors like PTH, CT, 1 25 (OH 2)D 3, PGE 2and steroid hormones can stimulate or depress osteoclastic activity, however the problem here is what kind of spatial control is effective in nor-mal bone turn-over and in local pathological condi-tions like the loss of bone stock in loosening of prostheses It has been suggested that in normal turn-over resident bone cells, namely active and resting osteoblasts, can cause a local change in the properties of the bone removing some barrier, which nature re-mains speculative, and this allows osteoclasts to rec-ognize the bone surface to be resorbed l 5, 6 l Since macrophages and foreign body giant cells are rich of lytic enzymes, as collagenase, proteases and acid hydrolases, and they are observed in contact with the bone surface, we are suggesting a sequence of events where bone resorption is initiated by macrophages which remove the extracellular barrier which nor-mally protects mineral crystals from osteoclastic rec-ognition, while osteoclasts migrate in and commence resorption of the exposed bone.
Acknowledgements During this study dr U E Pazzaglia was
supported by a NATO Senior Fellowship ( 217 18/04 24 9 84) from the National Research Council of Italy The authors are grateful to Mr Muirhead-Allwood, FRCS the Whittington Hospital, for case R L and to drs M J Wilkinson, A Z Mason and G Blum of the Dept of Biomedical En-gineering, Institute of Orthopaedics, for assistance with SEM.
References
1 Ash P, Loutit JF, Townsend KMS ( 1980) Osteoclasts de-rived from haematopoietic stem cells Nature 283: 669-670 2 Barnes DWH, Loutit JF, Sansom JM ( 1975) Histocompatible cells for the resolution of osteopetrosis in microphthalmic mice Proc R Soc Lond Biol 188:501-505
3 Buring K ( 1975) On the origin of cells in heterotopic bone formation Clin Orthop 110:293-301
4 Chambers TJ ( 1979) Phagocytosis and trypsin-resistant glass adhesion by osteoclasts in culture J Pathol 127:55-59
5 Chambers TJ ( 1980) The cellular basis of bone resorption. Clin Orthop 151: 283-293
6 Chambers TJ ( 1981) Phagocytic recognition of bone by macrophages J Pathol 135: 1-7
7 Chambers TJ, Horton MA ( 1984) Failure of cells of the mononuclear phagocyte series to resorb bone Calc Tissue Int 36:556-558
8 Chambers TJ, Revell PA, Fuller K, Athanasou NA ( 1984) Resorption of bone by isolated rabbit osteoclasts J Cell Science 66:383-399
9 Charnley J, Crawford WJ ( 1968) Histology of bone in con-tact with self-curing acrylic cement J Bone Joint Surg lBrl 50:228
10 Charnley J ( 1975) The histology of loosening between ac-rylic cement and bone J Bone Joint Surg lBrl 57:245 11 Fischman DA, Hay ED ( 1962) Origin of osteoclasts from
mononuclear leucocytes in regenerating new limbs Anat Rec 143:329-334
12 Freeman MAR, Bradley GW, Revell PA ( 1982) Observa-tions upon the interface between bone and polymethyl-methacrylate cement J Bone Joint Surg lBrl 64:489-493 13 Goldring SR, Schiller AL, Roelke M, Rourke CM, O'Neill
DA, Harris WH ( 1983) The synovial-like membrane at the bone-cement interface in loose total hip replacements and its proposed role in bone lysis J Bone Joint Surg lAml
65:575-584
14 Gothlin G, Ericsson JLE ( 1973) On the histogenesis of the cells in fracture callus Electron microscopic autoradiog-raphic observations in parabiotic rats and studies on label-led monocytes Virchows Arch Zell Pathol 12:318-329 15 Gothlin G, Ericsson JLE ( 1976) The osteoclast Clin
Orthop 120:201-231
16 Harris WH, Schiller AL, Scholler JM, Freiber RA, Scott R ( 1976) Extensive localized bone resorption in the femur following total hip replacement J Bone Joint Surg lAml 58:612-617
17 Hogg N, Shapiro IM, Jones SJ, Slusavenko M, Boyle A ( 1980) Lack of Fc receptors on osteoclasts Cell Tissue Res 212:509-516
18 Horton MA, Rimmer EF, Moore A, Chamber TJ ( 1987) On the origin of the osteoclasts: the cell surface phenotype of rodent osteoclasts Calc Tissue Int (in press)
19 Jee WSS, Nolan PD ( 1963) Origin of osteoclasts from the fusion of phagocytes Nature 200: 225-227
20 Jones SJ, Boyde A, Ali NN ( 1984) The resorption of bio-logical and non biobio-logical substrated by cultured avian and mammalian osteoclasts Anat Embryol 170:247-256 21 Jotereau FV, le Douarin NM ( 1978) The developmental
relationship between osteocytes and osteoclasts A study using the quail-chick nuclear marker in endochondral ossification Dev Biol 63:253-265
22 Kahn AJ, Stewart CC, Teitelbaum SL ( 1978) Contact-mediated bone resorption by human monocytes in vitro. Science 199:988-990
23 Langlais F, Postel M, Berry JP, Le Carpentier Y, Weill BJ ( 1980) L'intolerance aux debris d'usure des prostheses. Bilan immunologique et anatomopathologique de 30 cas. Int Orthop 4:145-153
24 Mundy GR, Altman AJ, Gondek MD, Bandelin JG ( 1977) Direct resorption of bone by human monocytes Science
U E Pazzaglia and J A S Pringle: The Role of Macrophages and Giant Cells 25 Pazzaglia UE, Ceciliani L, Wilkinson MJ, Dell'Orbo C
( 1985) Involvement of metal particles in loosening of metal-plastic total hip prostheses Arch Orthop Trauma Surg 104: 164-174
26 Rhinelander FW, Nelson CL, Stewart RD, Stewart CL ( 1979) Experimental reaming of the proximal femur and acrylic cement implantation Vascular and histological ef-fects Clin Orthop 141: 74-89
27 Uchida S, Yoshino S, Doi M, Kudo H ( 1980) Side-effects of prosthetic materials on the human body Int Orthop 3:285
28 Walker DG ( 1973) Osteopetrosis cured by temporary parabiosis Science 180:875-876
29 Willert HG ( 1973) Tissue reactions around joint implants and bone cement In: Chapchal G (ed) Arthroplasty of the hip Thieme, Stuttgart
30 Willert HG, Ludwig T, Semlitsch M ( 1974) Reaction of bone to methylmethacrylate after hip arthroplasty (a long term, gross, light-microscopic and scanning electron mi-croscopy study) J Bone Joint Surg lAml 56:1368-1382