Combined valvular procedure in minimally invasive cardiac
surgery
Abstract
OBJECTIVE: Combined valve surgery is associated with an increased perioperative morbidity
and mortality, the benefits of minimally invasive cardiac surgery are well known also in high risk patients. This study aimed to investigate feasibility and safety of minimally invasive (also video assisted) surgery for combined valvulare procedure through right anterolateral minithoracotomy.
METHODS: We retrospectively evaluated 331 consecutive patients with double or triple valve
disease who underwent valve repairs or replacement in minithoracotomy at our istitution between January 2004 and December 2018. The incision was periareoral (video assisted) or around the right breast approximately 5 cm in lenght. Cardiopulmonary bypass was established through femoral artery and vein with a small incision or with the direct cannulation of ascendenig aorta and percutaneous femoral and vein cannulation.
RESULTS: The cohort included 290 patients undergoing mitral and tricuspid valve surgery and 33
patients undergoing mitral and aortic valve surgery, 2 patients undergoing aortic and tricuspid valve surgery and 6 cases of triple valve surgery. In the study group there are 103 male (%) and 228 female (%) with a mean±SD age of 69.6±9.3 years and 70.4±8.9 years, respectively. The preoperative left ventricular ejection fraction was 56.1% ± 8.1% and the Logistic Euroscore was 9.32% ± 7.6%. Median cross-clamp time was 113 minutes [IQR range 95-138 minutes]. The median ICU stay was 1 day [range 1-25 days]; the median hospital stay was 6 days. Fourteen (4.2%) patients underwent surgical re-exploration for bleeding . Cerebrovascular accident occurred in 5 patients (1.5%). Two (0.6%) patients were re-operated on for valve dysfunction. Acute renal dysfunction occurred in 6 (1.8%) patients. Permanent pacemaker implantation was required in 16 (4.8%) patients. In-hospital mortality was 3.3% (n=11). Discharge-at-home rate was 28.3%, while hospital transfer or cardio-respiratory rehabilitation was necessary in 30.5% of case.
CONCLUSION: In patients undergoing double or triple valve surgery, a right mini-thoracotomy on
third or fourth intercostal space approach is associated with a low peri-operative morbidity and good early results.
INTRODUCTION
Over the past two decades, minimally invasive valve surgery techniques have been increasingly adopted with the goal of reducing the invasiveness of the surgical procedure and to offer the same quality, safety, and results as the standard procedure and nowadays is used in many centers as the primary surgical approach for isolated and complex valve operations. With the recent break-through of percutaneous valve interventions, the role of minimally invasive surgery is now more than ever prompted to expand in the practice of daily cardiac valve surgery. Moreover the benefits of a minimally or less invasive approach include a reduced incidence of postoperative atrial fibrillation, a decreased need for blood products, a lower morbidity, an enhanced postoperative recovery, and improved patient satisfaction. Patients with multiple native valve requiring surgical intervention has been associated with increased peri-operative morbidity and decreased long-term survival and this kind of benefits have also been observed in high-risk patients, along with a decrease in operative mortality afforded to elderly and obese patients when compared with conventional median sternotomy. In other high-risk populations, a minimally invasive approach using a right anterior mini-thoracotomy may be a viable alternative to conventional median sternotomy for concomitant valve disease. This single-center study analyze the safety, feasibility, and outcomes of minimally invasive combined-valve surgery performed via a right mini-thoracotomy approach.
METHODS
We retrospectively reviewed 15316 heart operations performed at our institution between January 2004 and December 2018 to identify those patients who underwent combined valve surgery via a minimally invasive right anterior mini-thoracotomy. In all patients, the valvular lesions were documented by diagnostic catheterization and/or echo-cardiography, and all operative reports and echocardiograms were reviewed. The patients’ baseline characteristics, operative variables,and postoperative data were reviewed. The variables selected were based on The Society of Thoracic Surgeons database definitions. All patients were evaluated in the outpatient setting 30 days after operation.
Surgical techniques
Surgery was performed under general anesthesia and defibrillation electrode pads were placed behind the right scapula and on the 5th intercostal space of left anterior axillary line. Cardiopulmonary bypass was established utilizing a femoral platform under transesophageal echo-cardiography (TEE) guidance. Femoral artery cannulation was performed for arterial perfusion. Inferior vena cava (IVC)cannulation was inserted in the femoral vein, and superior vena cava cannulation was performed by the anesthesiologist in the internal jugular vein.
For combined mitral and tricuspid valvulare disease our approach to minimally invasive is performed with video-assisted periareolar incision through 3rd intercostal space access Fig 1-2. For combined aortic and trisupid or for triple valve surgery a 5 cm incision was made through the fourth intercostal space and CPB was established with the direct cannulation of the aorta and percutaneous cannulation of the femoral veinFig 3-4. The ascending aorta was cross-clamped using a Chitwood clamp via a separate stab incision or with Cardiovision clamp. The surgical field was flooded with carbon dioxide at a flow of 2 L/minute. Myocardial protection was achieved using cold cristalloid cardioplegic solution at 4 °C Custodiol via aortic root for 6 minutes. The aortic valve was exposed through an oblique or transverse aortotomy. The decision to implant mechanical prosthetic valve or bio-prosthetic heart valve was influenced by each patient’s demographic and clinical profile but the choice was ultimately left to discretion of each individual patient. The size of pros-thetic valve was based on intra-operative actual measured. The mitral and valve has always been treated with a repair on first approach with annuloplasty and chordal placement or with resection of the posterior leaflet.
Statistical analysis
Variables were checked for normality and summary statistics reported as mean ± standard deviation or median and interquartile rage (IQR) when appropriate. Analysis between group was made using Wilcoxon test or Chi square test when appropriate. A p-value <0.05 was considered statistically significant. All the analysis were conducted using R statistical Software (version 3.11).
RESULTS
From January 2004 to December 2018, a total of 331 patients received combined valvular surgery at Our Center via right mini-thoracotomy. Baseline characteristics are reported in Table 1. Surgical success was achieved in all cases.
Intra-operative characteristics are reported in Table 2. Post-operative results are reported in Table 3. Two-hundred-ninety patients underwent mitral and tricuspid surgery; of those 91 patients were male (31.4%), with a median age was 70.2 years, a BMI of 24.9 and left ventricular ejection fraction (LVEF) of 56.4%. In this group 172 patients received a mitral anuloplasty and 287 tricuspid anuloplasty; cross clamp mean SD was 119 minutes. Only 11 patients were re-explored for bleeding, 2 patients had a stroke and 71 (37%) post-operative atrial fibrillation; none had acute kidney injury. Nine (3.2%) of those patients died in hospital (2 for cardiac events); the median intensive care unit was 2 days.
In another group we have considered 33 patients who underwent mitral and aortic surgery, 11 patients was male (33.3%), the median age was 71 years with a BMI of 25.1±3.6 and LVEF was 54.6%. In this group 31 undergoing in aortic replacement and 19 in mitral anuloplasty, cross clamp mean SD mas 116 minutes. Only 2 patients were re-explored for bleeding, 1 patients had a stroke and 10 (43%) atrial fibrillation; none acute kidney injury. Two (6.7%) of those patients died in hospital; the median intensive care unit was 1.7 days.
Moreover 6 patients underwent in triple valve surgery: all patients was female, the median age was 62.7 years with a BMI 25.5±5.3 and an LVEF of 50.6%. All patients have functional disease, cross clamp mean SD was144 minutes and haven’t been used suturless or rapid deployment valve.
No patients had a cerebrovascular accident and no one was re-explored for bleeding; 2 (40% ) patients experienced atrial fibrillation; none had an acute kidney injury. All patients were alive at 30 days and the median intensive care unit was 2.8 days.
Only 2 patients undergoing in aorto-tricuspid surgery with similar baseline characteristics and similar results, with no dead at 30 days.
DISCUSSION
With progress of cardiac surgery techniques and increasing demand for high-quality life, many minimally invasive approaches have been applied in clinical practice, instead of median sternotomy. At present, minimally invasive procedures for cardiac valve replacement mainly include minimally invasive video-assisted thoracoscopic mitral valve replacement; 2) total thoracoscopic mitral valve replacement; 3) right parasternal approach for aortic valve replacement; 4) right anterior lateral incision for aortic valve replacement through the 2ndintercostal space; 5)upper J-shaped mini-sternotomy for aortic valve replacement;6)right subaxillary mini-thoracotomy for aortic or double valve replacement; 7) small incision under right breast for mitral valve replacement.
The feasibility and safety of minimally invasive also video-assisted double or triple valve surgery through a right mini-thoracotomy has not been investigated extensively. In our center the surgical approch has evolved, today the approach it’s decided based on type of intervention and on the basic charateristic of the patient.
Operative safety is considered the most important factor to evaluate when a patient is considering a mini-mally invasive procedure. Evaluation of the surgical mortality was considered mandatory. One of the most important findings of this study was that patients who underwent minimally invasive multi-valve procedure via right mini-thoracotomy received a similar surgical mortality as patients who underwent conventional multi-valve procedure via full median sternotomy, without adverse events(including repeat valve operation, para-valvular leak, and moderate or severe mitral valve regurgitation following valvuloplasty). This evidence was in line with the results of most of the propensity-matched studies, our study reported demonstrate a very low surgical mortality and intra-opertive complication. Another important finding was that patients who underwent multi-valve procedure via right mini-thoracotomy were less likely to receive postoperative new onset of atrial fibrillation and red cell transfusion by comparison with full median sternotomy. In fact probably the limited heart manipulation particularly in cases of minimally invasive surgery via right thoracotomy, was associated with a reduction in the incidence of postoperative atrial fibrillation. Moreover many studies have reported a lower need for transfusion in minimally invasive cardiac surgery for limited tissue trauma. In this study the postoperattive atrial fibrillation was lower tha 43% in all group of patient and only 14 patients were re-open for bleeding. In literature many
studies describe longer aortic cross clamping and cardio-pulmunary by-pass times in patients who received multi valve procedure in right mini thoracotomy compared to full median sternotomy but in all report a statistically significant increase in cardiopulmonary by-pass related adverse effects was not obeserved. In our experience the mean sd clamp time was between 108-144 minuites and the CPB time was between 170-190 minutes. Shorter ICU stay and post-operative hospitalization time are well demonstrate in literature and also in this study our data confirme this trend demonstrating also a faster rehabilitation. Nevertheless, previous studies have suggested that minimally invasive valve surgery via right mini-thoracotomy is associated with a higher incidence of postoperative cerebro-vascular events. The reason may be that high atherosclerotic burden in the aortic arch and descending aorta may play a crucial role in the incidence of postoperative cerebrovascular accident when using retrograde perfusion, especially in elderly patients. By contrast, this study reported a low incidence of stroke, and for this reason is very important the selection of patients with a preoperative Angio Tac with calcium score to evaluate strategies of cannulation. In fact It is important to keep in mind that minimally invasive surgery for combined mitral and aortic valve procedure via right mini-thoracotomy was not indicated for all patients. Essentially, where patients had no history of sternotomy or thoracotomy and if a computed tomography scan showed more than half of the ascending aorta to be on the right with respect to the right sternal border at the level of the main pulmonary artery, and if the distance from the ascending aorta to the sternum was less than 10cm, they were considered to be suitable candidates. Additionally, another concern with minimally invasive multi-valve sur-gery was that of obtaining adequate exposure. In circumstances where adequate exposure cannot be obtained, minimally invasive surgery may need to be converted to a full median sternotomy. In the present study, adequate exposure of operative filed was obtained in all pa-ients, and no patients required conversion to a median sternotomy.
Conclusion
This single-center, propensity-matched study showed that, in patients requiring combined mitral and aortic valve procedure with or without tricuspid annuloplasty, a right mini-thoracotomy approach may be utilized with acceptable early clinical outcomes. In some categories of patients it may be considered as a feasible alternative to the conventional full sternotomy approac
TABLES
Table 1 - Baseline Characteristics
Aorto-tricuspid Mitro-aortic Mitro-tricuspide
Triple valve surgery N 2 33 290 6 Age 73.32 (7.37) 71.09 (10.55) 70.24 (8.86) 62.74 (7.67) Male 1 ( 50.0) 11 ( 33.3) 91 (31.4) 0 ( 0.0) BMI 27.62 (0.11) 25.11 (3.64) 24.96 (4.04) 25.54 (5.30) BSA 1.71 (0.15) 1.73 (0.18) 1.74 (0.25) 1.70 (0.20) LVEF (%) 55.00 (0.00) 54.67 (9.90) 56.45 (7.80) 50.67 (12.99) Hypertention 2 (100.0) 21 ( 63.6) 167 (57.6) 3 ( 50.0) Diabetes Mellitus type 2 0 ( 0.0) 10 ( 30.3) 27 ( 9.3) 3 ( 50.0) CKD 1 (100.0) 1 ( 3.4) 8 ( 3.8) 0 ( 0.0) Lung Disease 0 ( 0.0) 1 ( 3.0) 7 ( 2.4) 0 ( 0.0) Previous CABG 0 ( 0.0) 0 ( 0.0) 3 ( 1.0) 0 ( 0.0) Arrhytmia - AF/Flutter 1 (100.0) 0 ( 0.0) 22 (40.7) 1 (100.0) - Synus Rhythm 0 ( 0.0) 5 (100.0) 31 (57.4) 0 ( 0.0) - Malignant arrhythmias 0 ( 0.0) 0 ( 0.0) 1 ( 1.9) 0 ( 0.0) Logistis EuroScore (%) 10.93 (5.48) 8.78 (9.12) 9.43 (7.52) 6.39 (5.16)
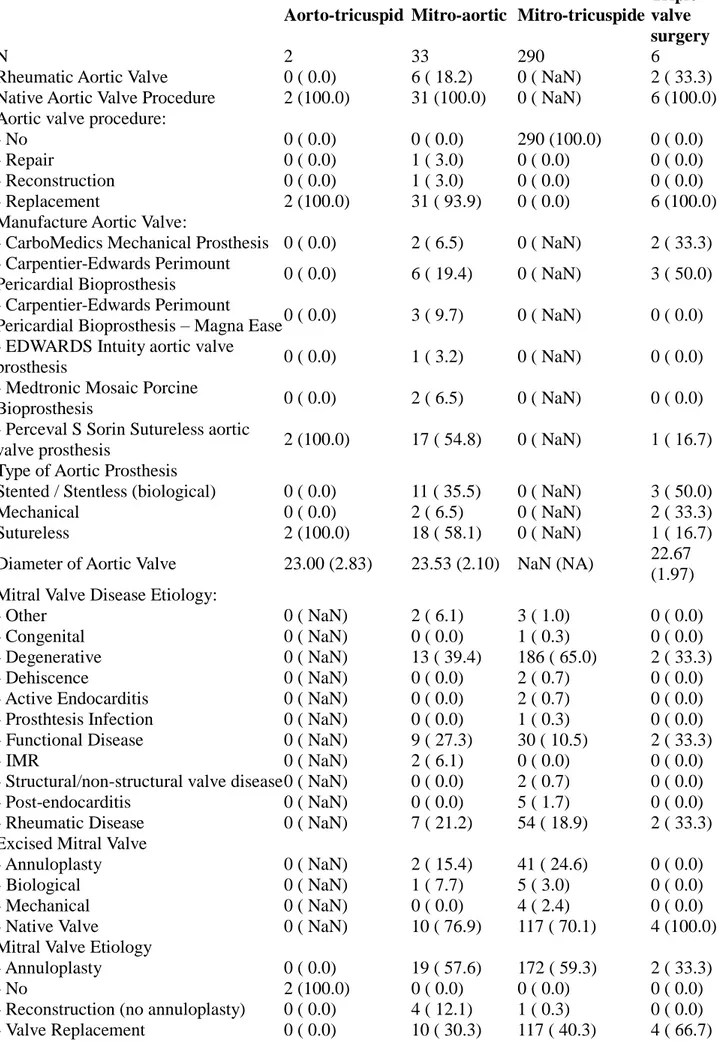
Table 2 - Operative Characteristics
Aorto-tricuspid Mitro-aortic Mitro-tricuspide
Triple valve surgery
N 2 33 290 6
Rheumatic Aortic Valve 0 ( 0.0) 6 ( 18.2) 0 ( NaN) 2 ( 33.3) Native Aortic Valve Procedure 2 (100.0) 31 (100.0) 0 ( NaN) 6 (100.0) Aortic valve procedure:
- No 0 ( 0.0) 0 ( 0.0) 290 (100.0) 0 ( 0.0) - Repair 0 ( 0.0) 1 ( 3.0) 0 ( 0.0) 0 ( 0.0) - Reconstruction 0 ( 0.0) 1 ( 3.0) 0 ( 0.0) 0 ( 0.0) - Replacement 2 (100.0) 31 ( 93.9) 0 ( 0.0) 6 (100.0) Manufacture Aortic Valve:
- CarboMedics Mechanical Prosthesis 0 ( 0.0) 2 ( 6.5) 0 ( NaN) 2 ( 33.3) - Carpentier-Edwards Perimount
Pericardial Bioprosthesis 0 ( 0.0) 6 ( 19.4) 0 ( NaN) 3 ( 50.0) - Carpentier-Edwards Perimount
Pericardial Bioprosthesis – Magna Ease 0 ( 0.0) 3 ( 9.7) 0 ( NaN) 0 ( 0.0) - EDWARDS Intuity aortic valve
prosthesis 0 ( 0.0) 1 ( 3.2) 0 ( NaN) 0 ( 0.0) - Medtronic Mosaic Porcine
Bioprosthesis 0 ( 0.0) 2 ( 6.5) 0 ( NaN) 0 ( 0.0) - Perceval S Sorin Sutureless aortic
valve prosthesis 2 (100.0) 17 ( 54.8) 0 ( NaN) 1 ( 16.7) Type of Aortic Prosthesis
Stented / Stentless (biological) 0 ( 0.0) 11 ( 35.5) 0 ( NaN) 3 ( 50.0) Mechanical 0 ( 0.0) 2 ( 6.5) 0 ( NaN) 2 ( 33.3) Sutureless 2 (100.0) 18 ( 58.1) 0 ( NaN) 1 ( 16.7) Diameter of Aortic Valve 23.00 (2.83) 23.53 (2.10) NaN (NA) 22.67
(1.97) Mitral Valve Disease Etiology:
- Other 0 ( NaN) 2 ( 6.1) 3 ( 1.0) 0 ( 0.0) - Congenital 0 ( NaN) 0 ( 0.0) 1 ( 0.3) 0 ( 0.0) - Degenerative 0 ( NaN) 13 ( 39.4) 186 ( 65.0) 2 ( 33.3) - Dehiscence 0 ( NaN) 0 ( 0.0) 2 ( 0.7) 0 ( 0.0) - Active Endocarditis 0 ( NaN) 0 ( 0.0) 2 ( 0.7) 0 ( 0.0) - Prosthtesis Infection 0 ( NaN) 0 ( 0.0) 1 ( 0.3) 0 ( 0.0) - Functional Disease 0 ( NaN) 9 ( 27.3) 30 ( 10.5) 2 ( 33.3) - IMR 0 ( NaN) 2 ( 6.1) 0 ( 0.0) 0 ( 0.0) - Structural/non-structural valve disease 0 ( NaN) 0 ( 0.0) 2 ( 0.7) 0 ( 0.0) - Post-endocarditis 0 ( NaN) 0 ( 0.0) 5 ( 1.7) 0 ( 0.0) - Rheumatic Disease 0 ( NaN) 7 ( 21.2) 54 ( 18.9) 2 ( 33.3) Excised Mitral Valve
- Annuloplasty 0 ( NaN) 2 ( 15.4) 41 ( 24.6) 0 ( 0.0) - Biological 0 ( NaN) 1 ( 7.7) 5 ( 3.0) 0 ( 0.0) - Mechanical 0 ( NaN) 0 ( 0.0) 4 ( 2.4) 0 ( 0.0) - Native Valve 0 ( NaN) 10 ( 76.9) 117 ( 70.1) 4 (100.0) Mitral Valve Etiology
- Annuloplasty 0 ( 0.0) 19 ( 57.6) 172 ( 59.3) 2 ( 33.3) - No 2 (100.0) 0 ( 0.0) 0 ( 0.0) 0 ( 0.0) - Reconstruction (no annuloplasty) 0 ( 0.0) 4 ( 12.1) 1 ( 0.3) 0 ( 0.0) - Valve Replacement 0 ( 0.0) 10 ( 30.3) 117 ( 40.3) 4 ( 66.7)
Aorto-tricuspid Mitro-aortic Mitro-tricuspide Triple valve surgery Mitral Prosthesis: - Biological 0 ( 0.0) 6 ( 21.4) 60 ( 29.6) 2 ( 40.0) - Mechanical 0 ( 0.0) 4 ( 14.3) 57 ( 28.1) 2 ( 40.0) - No 2 (100.0) 18 ( 64.3) 86 ( 42.4) 1 ( 20.0) Mitral valve prosthesis diamenter: NaN (NA) 29.38 (2.72) 30.83 (3.78) 27.33
(1.03) Tricuspid Valve Procedure:
- Annuloplasty 2 (100.0) 0 ( 0.0) 287 ( 99.0) 6 (100.0) - No 0 ( 0.0) 33 (100.0) 0 ( 0.0) 0 ( 0.0) - Replacement 0 ( 0.0) 0 ( 0.0) 3 ( 1.0) 0 ( 0.0) Excised Tricuspid Valve
- Annuloplasty ring 0 ( NaN) 0 ( NaN) 64 ( 72.7) 0 ( NaN) - Biological 0 ( NaN) 0 ( NaN) 1 ( 1.1) 0 ( NaN) - Native Valve 0 ( NaN) 0 ( NaN) 23 ( 26.1) 0 ( NaN) Tricuspid Valve Etiology:
- Other 0 ( 0.0) 0 ( NaN) 1 ( 0.4) 0 ( 0.0) - Congenital 0 ( 0.0) 0 ( NaN) 1 ( 0.4) 0 ( 0.0) - Degenerative 0 ( 0.0) 0 ( NaN) 22 ( 7.7) 0 ( 0.0) - Functional Diseas 1 (100.0) 0 ( NaN) 258 ( 90.5) 6 (100.0) - Chronic rheumatic disease 0 ( 0.0) 0 ( NaN) 3 ( 1.1) 0 ( 0.0) ProtesiImpiantataTricuspidalica (%)
Anuloplastica anello 2 (100.0) 0 ( NaN) 237 ( 98.3) 4 (100.0) Biologica 0 ( 0.0) 0 ( NaN) 3 ( 1.2) 0 ( 0.0) Homograft 0 ( 0.0) 0 ( NaN) 1 ( 0.4) 0 ( 0.0) CodiceImpiantoValvolaTricuspide (%)
Carpentier-Edwards MC3 0 ( 0.0) 0 ( NaN) 79 ( 28.9) 3 ( 50.0) Carpentier-Edwards Perimount
Pericardial Bioprosthesis 0 ( 0.0) 0 ( NaN) 1 ( 0.4) 0 ( 0.0) Carpentier-Edwards Physio Ring 0 ( 0.0) 0 ( NaN) 9 ( 3.3) 0 ( 0.0) Carpentier-Edwards Physio Ring
(tricuspid) 1 ( 50.0) 0 ( NaN) 76 ( 27.8) 0 ( 0.0) Contour 3D Tricuspid Annuloplasty
Ring – Medtronic 1 ( 50.0) 0 ( NaN) 42 ( 15.4) 2 ( 33.3) Medtronic Future Band 0 ( 0.0) 0 ( NaN) 10 ( 3.7) 0 ( 0.0) Medtronic Mosaic Porcine
Bioprosthesis 0 ( 0.0) 0 ( NaN) 2 ( 0.7) 0 ( 0.0) Simplici-T Annuloplasty System –
Tricuspid Medtronic 0 ( 0.0) 0 ( NaN) 1 ( 0.4) 0 ( 0.0) XXX – Other tricuspid valve 0 ( 0.0) 0 ( NaN) 53 ( 19.4) 1 ( 16.7) Tricuspid Valve Diameter (mean (SD)) 31.00 (4.24) NaN (NA) 30.01 (9.11) 29.60
(0.89) Cec = Sì (%) 2 (100.0) 33 (100.0) 284 ( 99.3) 6 (100.0) Cross Clamp Cross-Clamp 2 (100.0) 33 (100.0) 273 ( 95.5) 6 (100.0) None 0 ( 0.0) 0 ( 0.0) 7 ( 2.4) 0 ( 0.0) Intra-aortic ballon 0 ( 0.0) 0 ( 0.0) 6 ( 2.1) 0 ( 0.0) Cardioplegia (%) Others 0 ( 0.0) 0 ( 0.0) 1 ( 0.4) 0 ( 0.0) Crystalloid 1 ( 50.0) 14 ( 42.4) 199 ( 70.3) 4 ( 66.7)
Aorto-tricuspid Mitro-aortic Mitro-tricuspide Triple valve surgery Warm blood 1 ( 50.0) 19 ( 57.6) 73 ( 25.8) 2 ( 33.3) No 0 ( 0.0) 0 ( 0.0) 10 ( 3.5) 0 ( 0.0) CEC total time (mean (SD)) 173.50 (62.93) 171.79
(107.34) 174.13 (55.32)
190.17 (43.99) Cross clamping total time (mean (SD)) 108.50 (19.09) 116.33 (38.96) 119.74 (38.74) 144.17
(26.15) WeaningCECre-startCEC = Sì (%) 0 ( 0.0) 0 ( 0.0) 9 ( 3.4) 0 ( 0.0) CEClower temperature (mean (SD)) 34.00 (0.00) 33.91 (0.42) 33.18 (3.72) 33.30
(1.19) HCT.lower.in.CEC (mean (SD)) 22.70 (0.71) 23.24 (5.55) 21.30 (8.76) 27.03
(5.20) Trasfusion during Cec = Sì (%) 2 (100.0) 10 ( 32.3) 25 ( 9.2) 0 ( 0.0) WeaningCECInotropi = Sì (%) 0 ( 0.0) 9 ( 30.0) 61 ( 23.0) 0 ( 0.0) Primary indacationIABP (%)
Hemodynamic instability 0 ( NaN) 1 (100.0) 1 ( 20.0) 0 ( NaN) No weaning CEC 0 ( NaN) 0 ( 0.0) 3 ( 60.0) 0 ( NaN) Profilattico 0 ( NaN) 0 ( 0.0) 1 ( 20.0) 0 ( NaN) IABP = Sì (%) 0 ( 0.0) 1 ( 3.6) 6 ( 2.3) 0 ( 0.0) Artery cannulation = Femoral artery (%) 1 ( 50.0) 2 ( 6.5) 71 ( 25.4) 0 ( 0.0) Vein cannulation (%) Right atrium 0 ( 0.0) 0 ( 0.0) 5 ( 1.8) 0 ( 0.0) Bicaval 0 ( 0.0) 0 ( 0.0) 3 ( 1.1) 1 ( 16.7) Femoral vein 1 ( 50.0) 31 (100.0) 256 ( 91.8) 5 ( 83.3) Femoral and jugular vein 1 ( 50.0) 0 ( 0.0) 15 ( 5.4) 0 ( 0.0) Primary incision
= Right minithoracotomy(%) 2 (100.0) 33 (100.0) 290 (100.0) 6 (100.0) Conversion of incision = Yes (%) 0 ( 0.0) 2 ( 6.1) 8 ( 2.8) 0 ( 0.0) Causae of Conversion (%)
Other 0 ( 0.0) 2 ( 6.2) 2 ( 0.7) 0 ( 0.0) Exposition 0 ( 0.0) 0 ( 0.0) 2 ( 0.7) 0 ( 0.0) none 2 (100.0) 30 ( 93.8) 280 ( 97.2) 6 (100.0) Bleeding 0 ( 0.0) 0 ( 0.0) 4 ( 1.4) 0 ( 0.0)
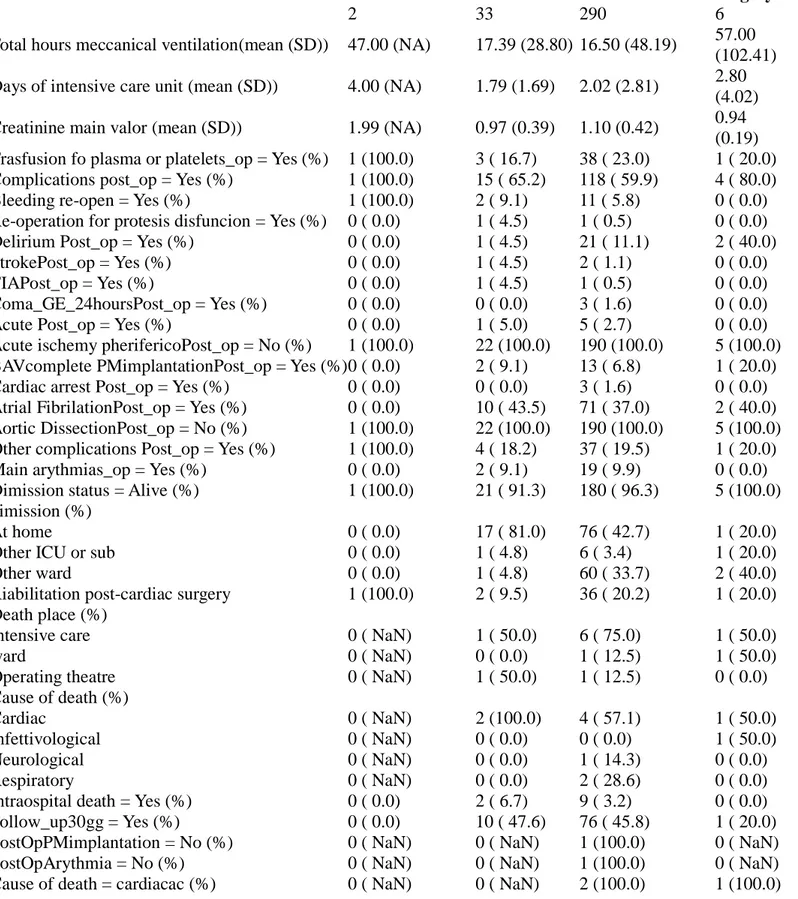
Table 3 - Post-Operative Results
Aorto-tricuspid Mitro-aortic Mitro-tricuspide
Triple valve surgery
n 2 33 290 6
Total hours meccanical ventilation(mean (SD)) 47.00 (NA) 17.39 (28.80) 16.50 (48.19) 57.00 (102.41) Days of intensive care unit (mean (SD)) 4.00 (NA) 1.79 (1.69) 2.02 (2.81) 2.80
(4.02) Creatinine main valor (mean (SD)) 1.99 (NA) 0.97 (0.39) 1.10 (0.42) 0.94
(0.19) Trasfusion fo plasma or platelets_op = Yes (%) 1 (100.0) 3 ( 16.7) 38 ( 23.0) 1 ( 20.0) Complications post_op = Yes (%) 1 (100.0) 15 ( 65.2) 118 ( 59.9) 4 ( 80.0) Bleeding re-open = Yes (%) 1 (100.0) 2 ( 9.1) 11 ( 5.8) 0 ( 0.0) Re-operation for protesis disfuncion = Yes (%) 0 ( 0.0) 1 ( 4.5) 1 ( 0.5) 0 ( 0.0) Delirium Post_op = Yes (%) 0 ( 0.0) 1 ( 4.5) 21 ( 11.1) 2 ( 40.0) StrokePost_op = Yes (%) 0 ( 0.0) 1 ( 4.5) 2 ( 1.1) 0 ( 0.0) TIAPost_op = Yes (%) 0 ( 0.0) 1 ( 4.5) 1 ( 0.5) 0 ( 0.0) Coma_GE_24hoursPost_op = Yes (%) 0 ( 0.0) 0 ( 0.0) 3 ( 1.6) 0 ( 0.0) Acute Post_op = Yes (%) 0 ( 0.0) 1 ( 5.0) 5 ( 2.7) 0 ( 0.0) Acute ischemy pherifericoPost_op = No (%) 1 (100.0) 22 (100.0) 190 (100.0) 5 (100.0) BAVcomplete PMimplantationPost_op = Yes (%) 0 ( 0.0) 2 ( 9.1) 13 ( 6.8) 1 ( 20.0) Cardiac arrest Post_op = Yes (%) 0 ( 0.0) 0 ( 0.0) 3 ( 1.6) 0 ( 0.0) Atrial FibrilationPost_op = Yes (%) 0 ( 0.0) 10 ( 43.5) 71 ( 37.0) 2 ( 40.0) Aortic DissectionPost_op = No (%) 1 (100.0) 22 (100.0) 190 (100.0) 5 (100.0) Other complications Post_op = Yes (%) 1 (100.0) 4 ( 18.2) 37 ( 19.5) 1 ( 20.0) Main arythmias_op = Yes (%) 0 ( 0.0) 2 ( 9.1) 19 ( 9.9) 0 ( 0.0) Dimission status = Alive (%) 1 (100.0) 21 ( 91.3) 180 ( 96.3) 5 (100.0) dimission (%)
At home 0 ( 0.0) 17 ( 81.0) 76 ( 42.7) 1 ( 20.0) Other ICU or sub 0 ( 0.0) 1 ( 4.8) 6 ( 3.4) 1 ( 20.0) Other ward 0 ( 0.0) 1 ( 4.8) 60 ( 33.7) 2 ( 40.0) Riabilitation post-cardiac surgery 1 (100.0) 2 ( 9.5) 36 ( 20.2) 1 ( 20.0) Death place (%)
Intensive care 0 ( NaN) 1 ( 50.0) 6 ( 75.0) 1 ( 50.0) ward 0 ( NaN) 0 ( 0.0) 1 ( 12.5) 1 ( 50.0) Operating theatre 0 ( NaN) 1 ( 50.0) 1 ( 12.5) 0 ( 0.0) Cause of death (%)
Cardiac 0 ( NaN) 2 (100.0) 4 ( 57.1) 1 ( 50.0) Infettivological 0 ( NaN) 0 ( 0.0) 0 ( 0.0) 1 ( 50.0) Neurological 0 ( NaN) 0 ( 0.0) 1 ( 14.3) 0 ( 0.0) Respiratory 0 ( NaN) 0 ( 0.0) 2 ( 28.6) 0 ( 0.0) Intraospital death = Yes (%) 0 ( 0.0) 2 ( 6.7) 9 ( 3.2) 0 ( 0.0) Follow_up30gg = Yes (%) 0 ( 0.0) 10 ( 47.6) 76 ( 45.8) 1 ( 20.0) PostOpPMimplantation = No (%) 0 ( NaN) 0 ( NaN) 1 (100.0) 0 ( NaN) PostOpArythmia = No (%) 0 ( NaN) 0 ( NaN) 1 (100.0) 0 ( NaN) Cause of death = cardiacac (%) 0 ( NaN) 0 ( NaN) 2 (100.0) 1 (100.0)