ContentslistsavailableatScienceDirect
International
Journal
of
Surgery
Case
Reports
jo u r n al ho me p a g e :w w w . c a s e r e p o r t s . c o m
Ante
situm
liver
resection
with
inferior
vena
cava
replacement
under
hypothermic
cardiopolmunary
bypass
for
hepatoblastoma:
Report
of
a
case
and
review
of
the
literature
Roberta
Angelico
a,
Annalisa
Passariello
b,c,
Michele
Pilato
d,
Tommaso
Cozzolino
b,
Marcello
Piazza
e,
Roberto
Miraglia
f,
Paolo
D’Angelo
g,
Mariella
Capasso
c,
Maria
Cristina
Saffioti
a,
Daniele
Alberti
h,
Marco
Spada
a,∗aDepartmentofAbdominalTransplantationandHepatobiliaryandPancreaticSurgery,BambinoGesùChildren’sHospitalIRCCS,Rome,Italy bDepartmentofTranslationalMedicalScience,UniversityofNaples“FedericoII”,Naples,Italy
cDepartmentofPediatricOncology,OspedaleSantobono-Pausilipon,Naples,Italy
dCardiacSurgeryandHeartTransplantationUnit,DepartmentfortheTreatmentandStudyofCardiothoracicDiseasesandCardiothoracicTransplantation,
IRCCS–ISMETT(MediterraneanInstituteforTransplantationandAdvancedSpecializedTherapies),Palermo,Italy
eDepartmentofAnesthesiaandIntensiveCare,IRCCS–ISMETT(MediterraneanInstituteforTransplantationandAdvancedSpecializedTherapies),
Palermo,Italy
fRadiologyService,DepartmentofDiagnosticandTherapeuticServices,IRCCS–ISMETT(MediterraneanInstituteforTransplantationandAdvanced
SpecializedTherapies),Palermo,Italy
g“GiovanniDiCristina”Children’sHospital,PediatricHematologyandOncology,Palermo,Italy hDepartmentofPediatricSurgery,“SpedaliCivili”Children’sHospital,Brescia,Italy
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received13February2017 Receivedinrevisedform4June2017 Accepted5June2017
Availableonline13June2017
Keywords: Hepatoblastoma
Inferiorvenacavatumoralthrombi Antesitumliverresection
Hypothermiccardiopolmunarybypass
a
b
s
t
r
a
c
t
INTRODUCTION:Hepatoblastomawith tumourthrombi extendingintoinferior-vena-cava andright atriumareoftenunresectablewithanextremelypoorprognosis.Thesurgicalapproachistechnically challengingandmightrequiremajorliverresectionwithvascularreconstructionandextracorporeal circulation.However,whichisthebestsurgicaltechniqueisyetunclear.
PRESENTATIONOFCASE:A11-months-oldboywasreferredforarighthepaticlobemass(90×78mm) suspiciousofhepatoblastomawithtumoralthrombiextendingintotheinferior-vena-cavaandtheright atrium,bilaterallunglesionsandserumalpha-fetoproteinlevelof50.795IU/mL.After8monthsof chemotherapy(SIOPEL2004-high-risk-Protocol),thelunglesionswerenolongerclearlyvisibleandthe hepatoblastomasizedecreasedto61×64mm.Thus,antesitumliverresectionwasplanned:afterhepatic parenchymaltransection,hypothermiccardiopulmonarybypasswasstartedandenblocresectionofthe extended-righthepaticlobe,theretro/suprahepaticcavaandthetumoraltrombiwasperformedwith concomitantcoldperfusionoftheremnantliver.Theinferior-vena-cavawasreplacedwithanaorticgraft fromablood-groupcompatiblecadavericdonor.Thepost-operativecoursewasuneventfulandafter8 monthsoffollow-upthechildhasnormalliverfunctionandanalpha-fetoproteinlevelandisfreeof diseaserecurrencewithpatentvasculargraft.
CONCLUSIONS:Wereportforthefirsttimeacaseofantesituliverresectionandinferior-vena-cava replacementassociatedwithhypothermiccardiopulmonarybypassinachildwithhepatoblastoma. Herein,weextensivelyreviewtheliteratureforhepatoblastomawiththumoralthrombiandwedescribe thetechnicalaspectsofantesitumapproach,whichisarealisticoptioninotherwiseunresectable hepa-toblastoma.
©2017TheAuthors.PublishedbyElsevierLtdonbehalfofIJSPublishingGroupLtd.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abbreviations:HLB,hepatoblastoma;IVC,inferiorvenacava;FAP,familialadenomatouspolyposis;LT,livertransplantation;PV,portalvein;TVE,totalhepaticvascular exclusion;UVC,uppervenacava;PRE-TEXT,pretreatmentextentofdisease;POST-TEXT,posttreatmentextentofdisease;SIOPEL,SociétéInternationaled’Oncologie Pédiatrique-EpithelialLiverTumorStudyGroup.
∗ Correspondingauthorat:DepartmentofAbdominalTransplantationandHepatobiliaryandpancreaticSurgery,Bambino,GesùChildren’sHospitalIRCCS,Piazza Sant’Onofrio4,00146Rome,Italy.
E-mailaddresses:[email protected](R.Angelico),[email protected](A.Passariello),[email protected](M.Pilato),[email protected]
(T.Cozzolino),[email protected](M.Piazza),[email protected](R.Miraglia),[email protected](P.D’Angelo),[email protected]
(M.Capasso),Mcristina.saffi[email protected](M.C.Saffioti),[email protected](D.Alberti),[email protected](M.Spada).
http://dx.doi.org/10.1016/j.ijscr.2017.06.008
2210-2612/©2017TheAuthors.PublishedbyElsevierLtdonbehalfofIJSPublishingGroupLtd.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
CASE
REPORT
–
OPEN
ACCESS
R.Angelicoetal./InternationalJournalofSurgeryCaseReports37(2017)90–96 91 1. Introduction
Hepatoblastoma (HBL) is the most common paediatric liver tumouranditoccursusuallyinthefirst3yearsoflife.Theincidence ofHBLhasincreasedintherecentyearsupto1.5casespermillion, anditis frequentlyassociated withlowbirth weightorgenetic anomalies. Themanagement ofHBL hasimpressively improved duetocombinedneoadjuvantchemotherapyandliverresection orlivertransplantation(LT),increasingtheoverall5-yearssurvival
rateupto75%[1].Theriskstratificationwiththepre-treatment
extentofdisease(PRE-TEXT)system,theworldwidemulticentre
trialsexperienceandthemultidisciplinarymanagement,improved
HBLprognosisandsurgicalresectability[2].However,HBLwith
tumourthrombiextendedintotheinferiorvenacava(IVC),withor
withouttheinvolvementoftherightatrium,mayresultchallenging
todefinethebestsurgicaltechnique.
Differentsurgicalprocedures,mainlyreportedinadults,have
beenproposedforlivertumourwithIVCinfiltration,includingtotal
hepaticvascularexclusion(TVE)[3].Thesetechniquesareeffective
to control haemorrhage and air embolism during liver
resec-tion,but maycauseseverehepatic ischemia/reperfusioninjury,
hemodynamicinstabilityandpotentialrenalinjury.Recently,liver
resectionunderhypothermicliverperfusionwithcytoprotective
solution(includinginsitu,exsituorantesitumtechniques)hasbeen
proposedforpreventingischemicliverinjury [4].Yet,no
expe-rienceofantesitumliverperfusionassociatedwithhypothermic
cardiopulmonarybypasshasbeenreportedinchildren.
Hereinwereportasuccessfulcaseofantesituliverresection
andIVCreplacementunderhypothermiccardiopulmonarybypass
(CPB),performedina21months-oldmalewithHBLandtumour
thrombiintotheIVCandrightatrium.
ThecurrentcasehasbeenreportedinlinewiththeSCARE
cri-teria[5].
2. Casereport
The patient was a 11-months old child referred for right
upper quadrant abdominal mass. He was born on term (birth
weight of 2.470kg) and had a familial history of
adenoma-touspolyposis(FAP).Atthetime ofadmission,thepatientwas
asymptomaticwithnormalvitalsigns,butphysicalexamination
revealedhepatomegaly,abdominalbloatingandumbilicalhernia.
Theultrasonography(US)showedalargehepaticmass(10cmin
diameter)intherightliver.Serumalpha-fetoprotein(AFP)level
was50.795 IU/mL.Liver function, coagulation,serum B-human
chorionicgonadotropin,blood cellcount,thyroidfunctionwere
withinnormallimits,exceptfortheevidenceofthrombocytosis
(805.000/UL).Computedtomography(CT)showedamassofthe
righthepaticlobe, 90×78mmin sizeextendingin segmentIV,
withdyshomogeneityandcalcifications.Thetumourdisplaced
pos-teriorlytherightkidney,dislocatedtheaortaandtheIVCtothe
leftside,stretchingtheceliactrunkandthesuperiormesenteric
artery(Fig.1).Tumoralthrombiwaspresent,extendingfromthe
righthepaticveinintotheIVCuptotherightatrium.Bilaterallung
lesions,suspiciousforHBLmetastases,werefoundaswell.Heart
involvementwasconfirmedbyechocardiography,whichdetected
a2.6cmechoicmassthroughthetricuspidvalve.
APRE-TEXTIIIstaging(P0,V3,M1)withlungandatrium-cava
metastasisattheoutsetwasdefined.Thechildunderwent
neoad-iuvantchemotherapy(SIOPEL2004highriskprotocol;cyclesA1-3
andcycleB)for 8months:3cycleswithcisplatin(70mg/m2,9
dosesadministered)anddoxorubicin(30mg/m2,6doses);4cycles
withcarboplatin(6mg/Kg,4doses)anddoxorubicin(0.83mg/Kg,
10 doses); and 2 cycles with carboplatin (25mg/Kg, 2 doses),
vincristine(0.05mg/Kg,5doses)and5-fluorouracil(33mg/Kg,6
doses).Duringthetreatment,thechildpresentedtransientsevere
thrombocytopeniaandoneepisodeofsepsissuccessfullytreated
withantibiotics.AfterneoadiuvanttherapyAFPdecreasedto879
IU/mL.CTscanshowedsizereductionoftheHBL(61×64mm),still
involvingtheIVCastherightandmiddlehepaticvein.Aleft
acces-soryhepaticarteryfromtheleftgastricarteryandareplacedright
hepaticarteryarisingfromthesuperiormesentericarterywere
documented;lunglesionswerenolongerclearlyvisible.
Cavogra-phydocumentedretrohepaticIVCinfiltrationbyHBL(Fig.2).After
multidisciplinary team meeting (involvingsurgeons, oncologist,
anaesthesiologistandradiologist),thesmallpatientwasproposed
for anextended rightliverresection,withIVCand intracardiac
thrombusremoval,whichwasperformedbyaseniorliver
trans-plantationandhepato-biliary-pancreaticsurgeon.
2.1. Surgicalprocedure
Thepatientwasplaced in supinepositionand theabdomen
wasexploredthroughabilateralsub-costalincisionwithxyphoid
extension.Therewasnoevidenceofascitesorperitonealmetastasis
andintraoperativeUSdocumentedthatthetumourdidnotinvolve
theleftlateralsegmentoftheliver.TheArantius’ligamentwas
dis-sectedandthelefthepaticveinwaslooped.Aftercholecystectomy,
thecommonbileduct,therighthepaticarteryandtheanteriorand
posteriorbranchesoftherightportalvein(PV)wereligatedand
divided.TheleftPVandthelefthepaticarterieswereidentified
andlooped.TheRexrecesswasthenexposedandvesselsfor
seg-mentIVweredivided.Parenchymaltransection,alongthelineof
thefalciformligament,wasperformedviaananteriorapproach,
using thehangingmanoeuvre with“notouchapproach”of the
tumour.Biliaryandvascularstructuresweredividedbetweenclips
ortie.Pringlemanoeuvrewasnotused.Avessellooparoundthe
IVCabovetherenalveinswasthenplaced.
Thexiphoidincisionwasextendeduptothejugulumwitha
mediansternotomyandthepericardialsacwasopened.After
sys-temic heparinization,theascending aorta,the uppervena cava
(UVC)andtheinfra-renalIVCwerecannulatedandclamped,and
theextracorporealcirculationwithCPBwasstarted.Body
temper-ature wasreduced to28◦C,in ordertoprotect theorgans.The
diaphragmwasincisedverticallydowntowardthesuprahepatic
IVCandthediaphragmaticveinsweredivided.Afterclampingthe
lefthepaticarteriesandthePV,theleftPVwascannulatedthough
therightPV stump.The lefthepatic veinwasdivided andante
situhypothermicliverperfusionwithCelsiorsolution(4◦C)was
started.Theliverwasfurthercooledwithiceonhissurface.After
divisionoftherighttriangularligament,anen-blocresectionofthe
extended-righthepaticlobe(segmentsI+IV-VIII),oftheretro-and
supra-hepaticIVCandoftheneoplasticthrombus(extendingfrom
therighthepaticveintotherightatrium)wasperformed(Fig.3).
The IVC was reconstructed with a fresh aortic graft from
cadaveric donor withidentical blood group.The aortic conduit
wasend-to-endanastomosedwiththerightatrium(throughthe
diaphragmaticostium)andinferiorlywiththesupra-renalIVCby
5/0prolenecontinuousrunningsutures.Theneo-IVCwasopened
immediatelybelowthediaphragmaticostiumandend-to-side
tri-angularanastomosiswasperformedbetweenthelefthepaticvein
andtheneo-IVCby6/0prolene.After40minofhypothermicliver
perfusion,theportalflushwasinterrupted.UVC,IVC,aorta,left
hep-aticarteriesandPVwerede-clamped,andtheleftlateralsegment
wasreperfused.Thepatientwasgraduallyrewarmedand,once
hemodynamicstabilityandgoodhaemostasiswereconfirmed,the
CPB was weaned off, after a total time of 71min. Roux-and-Y
end-to-sidehepaticojejunostomywith6/0PDSwasperformedfor
biliaryreconstruction.Beforethoraco-abdominalclosure,
Doppler-USestablishedagoodflowthroughtheneo-IVC,lefthepaticvein,
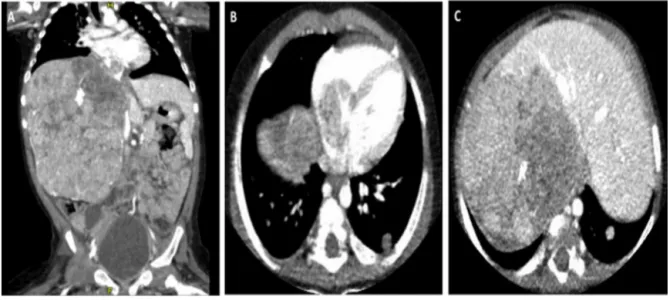
Fig.1.ComputerTomographyimagingatpresentation.
ComputerTomographyimagingatdiagnosisshowing:A)righthepaticlobemasswithcalcifications(90×78mm);B)lungmetastasisandtumoralthrombiinvadingthe inferiorvenacavaandtherightatriumtroughtherighthepaticvein;c)tumourmassintherightextendedlobeoftheliver.
Fig.2.Tumoralstagingafterneoadjuvantchemotherapyandpreoperativeassessment.
Imagingofhepatoblastoma(HBL)afterneoadjuvantchemotherapy(SIOPEL2004HRprotocol):A-B)CTscanshowingHBLintheextended-rightlobeofliverwithtumoral thrombiintotherighthepaticveinandtherightatrium;C)cavographyshowingtumoralthrombiinfiltratingandcompressingtheretrohepaticinferiorvenacavaand retroperitonealcollaterals.
10min,withabloodlossof200ml(videoofthesurgicaltechnique canbefoundinsupplementarymaterials).
Theresectedliverspecimenweighted210g.Thetumour mea-sured8×9cm. HistologicaldiagnosiswasHBL,mixedepithelial andmesenchymaltype,withteratoidfeatures,invadingthe hep-aticvenoussystemextensively.Thesurgicalmarginswereclear fromtumour.
2.2. Post-operativeoutcome
Thechildhadanuneventfulpost-operativecourseandwas dis-chargedafter23daysfromsurgery.
After4months,astagingCTscanshowedabsenceofdisease recurrenceandgoodliverperfusion,withpatentaorticgraft(Fig.4).
After12monthsoffollow-upthechildisingoodclinicalcondition
withnormalliverfunctiontestandanAFPlevelof1.1UI/mL.
3. Discussion
HBListhemostcommonprimarypaediatriclivertumour,with
greaterfrequencyamongmales.Themainsymptomsinclude
dis-comfortduetotheabdominalmassandlossofappetite,associated
withgeneralized fatiguesecondary toanaemia. Most HBLsare
sporadic,butsomeareassociatedwithgeneticabnormalitiesand
malformations, such as trisomy 18, Beckwith-Wiedemann
syn-drome, or FAP [1]. HBL should be suspected in patients aging
between6monthsand3yearsoldinthepresenceofanhepatic
tumourwiththrombocytosisandhighAFPlevels,whichwereall
presentinourcase.Histologically,HBLhasbeenclassifiesinthe
epithelialtype,whichisthemostcommonand presentswitha
combinationof mixedembryonaland fetalpatterns,and inthe
mesenchymaltype,whichoccurswithorwithoutteratoidfeatures.
CASE
REPORT
–
OPEN
ACCESS
R.Angelicoetal./InternationalJournalofSurgeryCaseReports37(2017)90–96 93
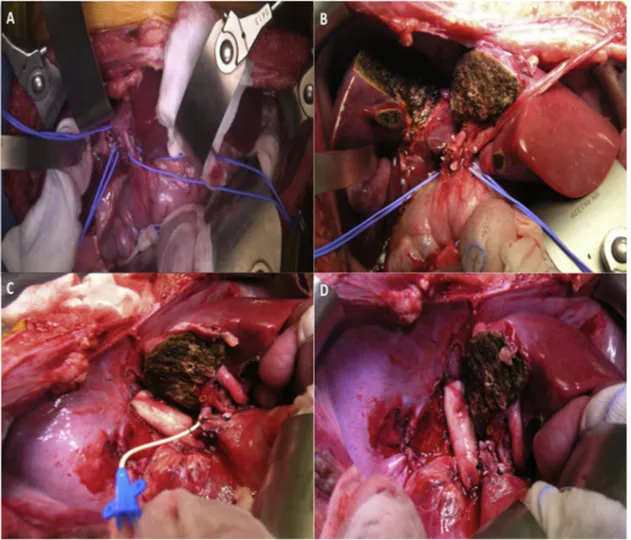
Fig.3. Technicalaspectsofantesitumliverresectionandinferiorvenacavareplacement.
IntraoperativeviewofA)hepatichilumdissection;B)parenchymaltransection,onthelineofthefalciformligamentviaanteriorapproach;C)antesituhypothermicliver perfusionwithCelsiorsolution(4◦C)throughtherightportalveinstumpandinferiorvenacavareplacementwithdonoraorticconduit(notethediaphragmaticostium resectedandreconstructed);D)finalviewofen-blocresectionoftheextended-righthepaticlobe(segmentsI+IV-VIII),theinferiorvenacavawithtumuralthrombiandthe diaphragmaticostium.
histologicalcomponents,andonlyrarelycomposedofasingle his-tologicaltype.Mesenchymalelementshavebeenassociatedwith animprovedprognosisinpatientswithadvanceddisease,asitwas inourcase[2].
ThePRE-TEXTsystemallowstostageandstratifytheriskof
HBLandtodefineitsprognosisandsurgicalresectability.Although
60%of tumoursare unresectableat presentation,HBLis highly
chemosensitive and up to85% of cases become operable after
neoadjuvantchemotherapy[2].
Thebestchemotherapyforadvanced tumoursis still
contro-versial.Theplatinum-basedchemotherapeuticregimenshavebeen
essentialinimprovingpatientsurvivalinadvancedHBL.The
Chil-dren’sOncologyGroup(COG)recommendscisplatin,5-fluoruracil
andvincristine,associatedwithdoxorubicinforintermediateand
high-risk patients, while the SociétéInternationale d’Oncologie
Pédiatrique-EpithelialLiverTumorStudyGroup(SIOPEL)
recom-mendsinveryhigh-riskpatientscisplatinintensificationtherapy
(SIOPEL-4protocol)[2].
In thecurrent case the SIOPEL4 protocolwas used
accord-ingly with presence of metastatic disease and major vascular
invasion. Since tumour remained unresectable at the first CT
re-evaluation withhighAFP levels,he receivedadditional
pre-operativechemotherapybeforesurgerywasattempted(datanot
shown).
CompletesurgicalremovalofHBL,byresectionorLT,remains
theonlytreatmentachievinglong-termsurvival.LT playsa key
roleinthemanagementofchildrenwithlargeandmultifocalHBL,
butequivalentlong-termdisease-freesurvivalhavebeenrecently
achievedwithlargenon-anatomicorextendedliverresection,
pro-videdthatcompletemacro-andmicro-scopictumourresectioncan
beachieved[6].
Although it must becarefully considered on a case-by-case
basis, multidisciplinaryposttreatmentextentofdisease
(POST-TEXT)tumourevaluationandintraoperativeliverinspectionare
essentialtodefinethebesttherapeuticmanagement.Inthissense,
promptreferraltoacenterwithexpertiseinbothpaediatricLTand
extremeresectionmustbeconsideredthegoldstandardincare
giving.POST-TEXTtumoursthatspareatleast1branchofthe
por-talveinand1hepaticveinshouldalwaysbeevaluatedforliver
resection.Whenvenousobstruction,encasement,and/orinvasion
ofthemainportalveinorbifurcationortheIVCorall3hepaticveins
arepresent,thetumourisclassifiedunresectableandintendedto
transplantation[2].
InthiscaseweoptedforamajorliverresectionwithIVC
recon-structionbecauseofevidenceoflungmetastasisandpresenceof
leftlateralliverfreeofdiseasewithadequateremnantlivervolume.
Hepaticresectionavoided exposingtheyoungboytolong-term
immunosuppression.
TumourthrombiinthehepaticveinsandIVCwithan
exten-sionuptotheatriumareassociatedwithhighriskofpulmonary
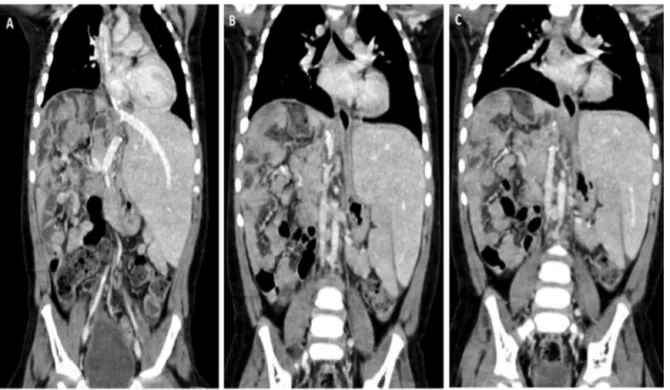
Fig.4.ComputerTomographyimagingaftersurgery.
ComputerTomographyscanafter4monthsfromsurgeryshowingpatentlefthepaticveinanastomosis(A)andretrohepaticcavareplacementwithaorticgraftfromcadaveric donor(B,C).
congestiveheartfailureandspreadofsystemicmetastasisandare mainlyreportedinadultswithhepatocellularcarcinoma[3].
Despitesurgicaltreatmentseemstoremaintheonlyeffective
therapeuticoption,thereisnoestablishedmanagementforsuch
cases.In1966,Heaneyetal.firstlyproposedtheTVEoftheliver[7].
TVEiseffectiveincontrollinghaemorrhageandairembolism,but
causesseverehemodynamicdisturbancescharacterizedby>30%
decreaseinmeanarterialpressure,>50%decreaseofcardiacindex
andsevereischemicliverdamage,inparticularinsmallremnant
liverafterneoajuvantchemotherapy[3].Evenitisnotmandatory,it
isadvisabletouseTVEincombinationwithCPBinordertoreduce
hemodynamicinstabilityandpotentialrenalinjury,inparticular
whenprongedTVEisrequired.
In1981,Einetal.describedthefirstsuccessfullyuseofCPB
asso-ciatedwithhypothermiccardiocirculatoryarrestin6childrenwith
rightatrialtumoralthrombi[8].However,theprocedureswere
associatedwithhighpost-operativehaemorrhageandmicroscopic
residualtumour(R1).Later,furtherreportsofmajorHBL
resec-tionsusingtheCPBhavebeenreported,assummarizedinTable1.
Manycaseshavebeenassociatedwithmajorcomplicationssuchas
post-operativedeadforpulmonaryembolism(possiblyrelatedto
tumoralthrombispreadingduringlivermobilization)[9];ischemic
cholangiopathyrequiring subsequent LT [10]; residual tumoral
thrombiinmajorvessels[6].
To reduce ischemic damage related to TVE and cellular
metabolismduringthisphase,theconceptofhypothermic
preser-vation,byliverperfusionwithcytoprotectivesolutionscombined
withcoolingoftheorgan’ssurface,hasbeeninvestigated.In1974,
Forneretal.describedthefirstinsituhypothermicliverperfusion
duringmajorliverresection,wherehypothermiawasinducedby
liverperfusionviathearterialandportalsystemwithcoldRinger’s
solution(4◦C)[11].However,incaseoftumourslocatedonthe
posteriorsideoftheliverandinvadingtheIVC,insituhypothermic
liverpreservationmaynotbesufficienttoexposetheretro-hepatic
venacava.Consequently,in1990Pichlmayretal.proposedtheex
situliverperfusion[12],wheretheliveriscompletelyremoved
fromthepatient, cooledwithice and perfusedwithcold
solu-tiononthebacktable;afterthebenchsurgerytheremnantliver
isreimplantedorthotopically.Later,in1991Hannounetal.[13]
introducedtheantesitumliverresectioncharacterizedbyno
hepa-toduodenalligamentdivision,coldliverperfusion,TVEanddivision
ofthesupra-hepatic IVC, whichallows therotationoftheliver
aroundthecoronaryaxiswithoptimalexposureofthehepaticveins
confluenceandtheretro-hepaticIVC.Belghitietal.describedthe
modifiedantesitumtechniqueinwhichtheIVCiscutaboveand
belowtheliver,permittingabettermobilizationoftheliver[14].A
recentreviewofhypothermicantesituresectionintumourofthe
hepatocavalconfluencesuggeststhatthis approachiseaserand
saferthentheexsitutechnique,withanacceptablemorbidityand
mortalityrate[4].
Tothebestofourknowledge,thecurrentreportisthefirstcase
ofantesitumliverresectionandIVCreplacementwithhypothermic
CPBforHBLinayoungchild.Sincethetumourwasinvolvingthe
extendedrightlobeoftheliverwiththeretro-hepaticIVCandthe
rightatrium,theCPBwasneeded.Anteriorapproachtotheliver
wasadoptedperformingparenchymaltransectionwith“notouch
technique”ofthelesion,toavoidtumoralembolization.Moreover,
toreducetheriskofbleedingduringthisphase,liverresectionwas
completedbeforeeparinizationandCPB,differingfromprevious
reports.Themodifiedantesitumtechniquepermittedtoexpose
optimallytheretro-hepaticcavabycuttingtheIVCaboveandbelow
theliver,tomobilizetheliveranteriorlyandtoreducetheischemia
liverinjuryoftheremnantsegmentsbyPVperfusion.Furthermore,
wedidn’tdividetheliverhilum,avoidingtheriskofhepaticartery
thrombosis.
Sofar,thelargestseriesoftheantesitumliverresectionwas
reportedbyRaabetal.:outof24,oneadultpatienthadHBL[15].
AuthorsadoptedanormothermicveinbypassandIVC
reconstruc-tionwasperformedwithautologoussaphenous;however,details
regardingtheoutcomeoftheHBLpatientarenotavailable.
Inthecurrentreportasimpletrombectomywasnotfleasible
sincethetumoralthrombiinfiltratedtheIVCwall.Therefore,
retro-hepaticIVCresectionandinterposition ofgraftwereneededto
pri-CASE
REPORT
–
OPEN
ACCESS
R.Angelicoetal./InternationalJournalofSurgeryCaseReports37(2017)90–96 95
Table 1 Literature reports of liver resection and cardiopolmunary bypass for hepatoblastoma with inferior vena cava tumoral thrombi. Report Year Cases Age (months)/Gender Type of vascular infiltration Metastatic disease* Neoadjuvant chemotherapy Adjuvant chemotherapy Type of liver resection IVC reconstruction CPB (type, min) Outcome Ein et al. [8] 1981 6** 8–15 yrs/4M, 2F NA None None Yes (5/6) NA None Hypothermic 20 ◦C, 43–75 min 2 died/2 Alive NED, 2 alive with lung metastasis Mestres et al. [9] 1991 1 36/M RA None DOXO + CIS None Right hepatectomy Transatrial trombectomy Hypothermic 20 ◦C, 146 min Died for polmunary embolism (day 23) Lautz et al. [10] 2011 1 96/F RA None VCR, CIS, 5FU VCR, CIS, 5FU Non anatomical resection Transatrial trombectomy Yes Alive, NED (LT for ischemic cholangiopathy) Fuchs et al. [6] 2016 2 NA IVC-RA None Platinum- based Yes NA 1:prothesis;1:pericardial patch Yes Died for tumoral thrombi recurrence Current case 2016 1 11/M IVC-RA Lungs CBCDA, 5FU, VCR, DOXO – Ante situm liver resection (right hepatectomy) Fresh aortic graft from cadaveric compatible donor Hypothermic, 71 min Alive, NED Abbreviations : CBCDA , Carboplatin; CIS , Cisplatin; CPB , cardiopolmunary bypass; DOXO , doxorubicin ; IVC , inferior vena cava; NA , non available; NED , non evidence of disease; RA , right atrium; VCR , vincristine; 5FU , F-fluoro-uracil. *Distant metastatic disease with the exception of vascular infiltration of IVC and right atrium. **In this case series, indications for surgery included: hepatoblastoma (n = 4), rabdomyosarcoma (n = 1), hepatocarcinoma (n = 1).
maryrepairorpatchingwithbovine’spericardiumorautologous peritoneumincaseoflimitedIVCinvolvement.Extensivevenous involvement requiressubstitutionwithsynthetic,autologousor heterologousfreshorcriopreservatedgraftconduit.Nodefinitive dataexistsinfavourofonetechniquecomparedtotheothers[16].
Inouryoungpatient,wepreferredtheinterpositionofagraftfrom
acompatiblecadavericdonortoreducetheriskofvesselcollapse
andtoavoidlong-termanticoagulation.
Inconclusion,althoughthesignificanceofourdataislimitedby
thecase-reportnatureofoursurgicalpractice,thecurrentcase
sug-geststhatantesitumliverresectionisfeasibleinchildrenwithliver
tumoursconsideredunresectablebyconventionalsurgeryorwhen
LT is contraindicatedor consideredas a secondline-treatment.
TheuseofhypothermicCPBissafeandallowsexpandingsurgical
indicationswhenprolongedTVEwithcomplexvessel
reconstruc-tionareneeded.Patientselection,preoperativeevaluationofthe
liverfunctionandanatomyaswellasintraoperativeassessment
areessential toachievegood outcome.Our findingsjustify
fur-therinvestigationstoidentifytheoptimalsurgicalmanagement
forchildrenwithlargeandcentrallylocatedlivertumours.
Conflictsofinterest
Noconflictsofinterest
Funding
Thisresearchdidnotreceiveanyspecificgrantfromthe
found-ingagenciesinthepublic,commercial,ornot-for-profitsectors.
Ethicalapproval
Notapplicable
Consentdeclaration
Writteninformedconsentwasobtainedfromthepatientfor
publicationofthiscasereportandaccompanyingimages.Acopy
ofthewrittenconsentisavailableforreviewbytheEditor-in-Chief
ofthisjournalonrequest.
Authorcontribution
-RobertaAngelico–Datacollection,analysis,reviewofthe
litera-tureandwrotemanuscript
-AnnalisaPassariello–Oncologicalmanagement,intellectual
con-tent,reviewoftheliterature
-PilatoMichele–Performedthecardiothoracicsurgery,
intellec-tualcontent
-CozzolinoTommaso–Oncologicalmanagement,datacollection,
reviewoftheliterature
-PiazzaMarcello–Oncologicalmanagement,analysisand
inter-pretation,intellectualcontent
-MiragliaRoberto–Datacollection,analysisandinterpretation
-D’AngeloPaolo–Oncologicalmanagement,analysisand
inter-pretation
-CapassoMariella–Analysisandinterpretation,intellectual
con-tent
-SaffiotiMariaCristina–Datacollection,analysisand
interpreta-tion
-AlbertiDaniele–Planningofsurgicalstrategy,intellectual
conti-nent
-SpadaMarco–Performedtheabdominalsurgery,draftthework,
Guarantor MarcoSpada.
AppendixA. Supplementarydata
Supplementarydataassociatedwiththisarticlecanbefound,in theonlineversion,athttp://dx.doi.org/10.1016/j.ijscr.2017.06.008. References
[1]D.C.Aronson,R.L.Meyers,Malignanttumorsoftheliverinchildren,Semin. Pediatr.Surg.25(5)(2016)265–275.
[2]P.Czauderna,B.Haeberle,E.Hiyama,A.Rangaswami,M.Krailo,R.Maibach, etal.,TheChildren’sHepatictumorsInternationalCollaboration(CHIC):novel globalraretumordatabaseyieldsnewprognosticfactorsinhepatoblastoma andbecomesaresearchmodel,Eur.J.Cancer52(2016)92–101.
[3]A.W.Hemming,K.L.Mekeel,I.Zendejas,R.D.Kim,J.K.Sicklick,A.I.Reed, Resectionoftheliverandinferiorvenacavaforhepaticmalignancy,J.Am. Coll.Surg.217(1)(2013)115–124(Discussion124–125).
[4]A.Mehrabi,H.Fonouni,M.Golriz,S.Hofer,M.Hafezi,N.N.Rahbari,etal., Hypothermicantesitumresectionintumorsofthehepatocavalconfluence, Dig.Surg.28(2)(2011)100–108.
[5]R.A.Agha,A.J.Fowler,A.Saetta,I.Barai,S.Rajmohan,OrgillDPandtheSCARE group.theSCAREstatement:consensus-basedsurgicalcasereportguidelines, Int.J.Surg.34(2016)180–186.
[6]J.Fuchs,S.Cavdar,G.Blumenstock,M.Ebinger,J.F.Schäfer,B.Sipos,etal., POST-TEXTIIIandIVhepatoblastoma:extendedhepaticresectionavoidsliver transplantationinselectedcases,Ann.Surg.(August(5))(2016)(Epubahead ofprint).
[7]J.P.Heaney,W.K.Stanton,D.S.Halbert,J.Seidel,T.Vice,Animproved techniqueforvascularisolationoftheliver:experimentalstudyandcase reports,Ann.Surg.163(1966)237–241.
[8]S.H.Ein,B.Shandling,W.G.Williams,G.Trusler,Majorhepatictumor resectionusingprofoundhypothermiaandcirculationarrest,J.Pediatr.Surg. 16(3)(1981)339–342.
[9]C.A.Mestres,K.Prabhakaran,O.A.Adebo,C.K.Kum,C.N.Lee,Combined resectionofhepatoblastomaandintracavalrightatrialextensionwith profoundhypothermiaandcirculatoryarrest,Eur.J.Cardiothorac.Surg.5(12) (1991)657–659.
[10]T.B.Lautz,T.Ben-Ami,N.Tantemsapya,Y.Gosiengfiao,R.A.Superina, SuccessfulnontransplantresectionofPOST-TEXTIIIandIVhepatoblastoma, Cancer117(9)(2011)1976–1983.
[11]J.G.Fortner,M.H.Shiu,D.W.Kinne,D.K.Kim,E.B.Castro,R.C.Watson,etal., Majorhepaticresectionusingvascularisolationandhypothermicperfusion, Ann.Surg.180(1974)644–652.
[12]R.Pichlmayr,H.Grosse,J.Hauss,G.Gubernatis,P.Lamesch,H.J.Bretschneider, Techniqueandpreliminaryresultsofextracorporealliversurgery(bench procedure)andofsurgeryontheinsituperfusedliver,Br.J.Surg.77(1990) 21–26.
[13]L.Hannoun,Y.Panis,P.Balladur,E.Delva,J.Honiger,E.Levy,etal.,Exsitu in-vivoliversurgery,Lancet337(1991)1616–1617.
[14]J.Belghiti,B.Dousset,A.Sauvanet,E.Lipinska,J.Aschehoug,F.Fekete, Preliminaryresultswith‘exsitu’surgeryforhepatictumors:analternative betweenpalliativetreatmentandlivertransplantation?Gastroenterol.Clin. Biol.15(1991)449–453.
[15]R.Raab,H.J.Schlitt,K.J.Oldhafer,A.Bornscheuer,H.Lang,R.Pichlmayr, Ex-vivoresectiontechniquesintissue-preservingsurgeryforliver malignancies,LangenbecksArch.Surg.385(3)(2000)179–184.
[16]N.N.Vladov,V.I.Mihaylov,N.V.Belev,V.M.Mutafchiiski,I.R.Takorov,S.K. Sergeev,etal.,Resectionandreconstructionoftheinferiorvenacavafor neoplasms,WorldJ.Gastrointest.Surg.27(4)(2012)96–101(4).
OpenAccess
ThisarticleispublishedOpenAccessatsciencedirect.com.ItisdistributedundertheIJSCRSupplementaltermsandconditions,which
permitsunrestrictednoncommercialuse,distribution,andreproductioninanymedium,providedtheoriginalauthorsandsourceare