Introduction
Bone marrow lesions (BMLs) of the knee are common subchondral bone defects that can be found in some fluid-sensitive MRI’s sequences [T2/proton density with fat suppression and short tau inversion recovery (STIR)] as an hyperintensity area or an edema-like signal (black arrow) [1]. The clinical and radiological meaning of these lesions is still controversial, but BMLs are often correlated with pain and functional impairment of the knee. This kind of alterations on MRI can be a sign of different pathological meanings like bone oedema but also trabecular necrosis, bone cysts,
fibrosis and, moreover, they are an indirect sign of the presence of cartilaginous fragments. The etiopathogenesis of bone marrow lesions involves an alteration of the subchondral bone characterized by oedema but also fibrosis, leukocyte infiltration, increase in vascularity associated with medullary necrosis, bone microfractures and a mineralization deficit: all these processes bring to an anomalous bone remodelling [2,3,4].
Bone marrow lesions of the knee can be divided in two main groups: traumatic and atraumatic. The differential diagnosis includes several conditions: contusions or traumatic fractures, cysts and erosions, developmental chondrosis, immobility
Abstract
Introduction: Subchondroplasty is a percutaneous procedure in which calcium phosphate is injected inside BMLs
(Bone Marrow Lesions) area under fluoroscopic guidance. The main aim of the present cohort study is to evaluate the effects of subchondroplasty associated to knee arthroscopy in reducing pain and improving in knee function in patients suffering from BMLs located on femoral condyles or tibial plateau.
Methods: 30 patients (mean age 65.4 years) were evaluated pre-operatively and at 6 and 12 months after surgery.
Numeric pain Rating Scale (NRS), Knee Society Score (KSS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), International Knee Documentation Committee (IKDC) were evaluated. Secondarily, edema healing and bone structure were controlled at follow-up by x-ray and MRI.
Results: An improvement in all evaluated scores was found at 6 months after surgery compared to the baseline. NRS
changed from a mean value of 7 to 1 at 6 months and to 0.86 at 1 year of follow-up, revealing a marked improvement of pain after the procedure (p<0.0001). Furthermore, IKDC and WOMAC scores showed a statistically significant improvement in knee function at 6 months after subchondroplasty (from 26.96 to 70.10 and from 46.87 to 9.00, respectively), which remained stable after 12 months; KSS in every section (objective, satisfaction and function) raised as well during the follow-up. In three cases the treatment failed and a total knee replacement was performed due to persistence of symptoms.
Conclusions: Subchondroplasty seems to be safe, reliable and effective in pain reduction and knee function
improvements, even though effects at long term still have to be verified.
Level of evidence: II, Prospective cohort study Keywords: BML; MRI; STIR; CRPS; SONK.
Bone marrow lesions in the knee:
early results of patients treated with
subcondroplasty
Pietro Randelli
1,2, Martina Ricci
2,3, Riccardo Compagnoni
1,21) Laboratory of Applied Biomechanics, Department of Biomedical Sciences for Health, Università degli Studi di Milano, Via Mangiagalli 31, 20133 Milan, Italy; 2) 1° Clinica Ortopedica, ASST Centro Specialistico Ortopedico Traumatologico Gaetano Pini-CTO, Piazza Cardinal Ferrari 1, 20122 Milan, Italy.
3) Residency in orthopedic and traumatology, Università degli Studi di Milano, Via Mangiagalli 31, 20133 Milan, Italy; Corresponding author: Riccardo Compagnoni - Via Pini,3 20122 Milano - [email protected]
Archivesof MedicineAnd surgery ofthe universityof Mil An Attribution-NonCommercial-NoDerivatives 4.0
3
and overload, transitory bone oedema syndrome, subchondral insufficiency fractures of the knee (SIFK) and osteonecrosis [5;6].
Traumatic BMLs tend to resolve spontaneously within 2-4 months and include: lesions associated with major traumas, bone contusions, subacute lesions related to overload and sport related repetitive microtraumatism. The most common example of bone contusions is observed in ACL tears: a bone edema can be seen on the lateral femoral condyle about the sulcus and in the posterior and lateral area of the tibial plateau [7]. In overextension injuries, bone contusions are located on anterior portion of proximal tibia and distal femur: they can be an indirect sign of PCL lesions. BMLs are also common in people affected by early or severe osteoarthritis [8,9] and they can be associated with meniscal tears or insufficiency and focal cartilage defects [10;14;15].
Other pathologies which cause BMLs include reversible and irreversible conditions. Among the reversible ones we count Transient osteoporosis (TOP), Regional migratory osteoporosis (RMO) and Complex regional pain syndrome (CRPS), also called Reflex sympathetic dystrophy (RSD) or Algodistrophy. All these conditions present a similar radiological pattern: diffuse hyper-intensity signal in the subchondral bone with blurred edges, that involves the articular surface without damaging it. The differential diagnosis between these conditions is based on age, sex and patient’s clinical history. On the other hand, we have irreversible conditions like Spontaneous osteonecrosis of the knee (SONK), avascular necrosis and post-arthroscopic or cartilage surgery osteonecrosis; among them we can include also Subchondral insufficiency fractures (SIFK) that can become irreversible if the subchondral fragment undergoes true necrosis and a low T1WI signal >4 mm thick is visible on MRI [8;9]. Subchondroplasty
Bone marrow lesions natural course involves persistence of knee pain and functional impairment and eventually partial or total/unicompartmental
knee replacement in some years from the diagnosis. The treatment options include a conservative or a surgical approach, depending on the size of the lesion and the presence of a necrotic area. Lesions larger than 5 cm² can lead to a subchondral bone collapse, so they often require an arthroplasty implantation. Conversely, lesions sized between 3.5 and 5 cm² can regress and even smaller lesions often heal spontaneously, therefore a conservative approach is indicated in lesions smaller than 3.5 cm² that don’t present necrosis. That includes NSAIDs, analgesic drugs, controlled load for 3-8 months. Other specific strategies available are pulsed electromagnetic fields (PEMFs), prostacyclin and bisphosphonates. For example, Iloprost, a prostacyclin analogous, promotes a better tissue perfusion, especially in the bone, it can also reduce pain and favor the regress of bone edema in small lesions, but the pharmacological effects at the base of these phenomena are not clear yet. Bisphosphonates, such as Ibadronate and Neridronate, can inhibit osteoclasts and reduce bone resorption. Clinical results after their use in the treatment of BML are not clear: many studies
Figure 1 - A typical case of bone marrow lesion in femoral condyle
show clinical and radiological improvements when used in osteonecrosis, transient bone marrow lesion syndrome and in CRPS [7,10-12;17]; instead, other studies show no difference between ibadronate and placebo [18]. In case of failure of these therapeutic options, a knee arthroplasty was often performed.
Recently, a new surgical procedure has been introduced into the clinical practice with the aim of reducing pain, avoiding or at least delaying a knee replacement: subchondroplasty. Subchondroplasty is a percutaneous procedure in which calcium phosphate, a biocompatible material very similar to the native bone apatite with osteo-inductive properties, is injected inside BML areas [19]. The goals of subchondroplasty are relieving patient’s symptoms, improving the mechanical strenght of subchondral bone, stimulating bone remodelling to avoid bone sagging and slowing down the arthritic degenerative process in order to postpone arthroplasty. The indications for this procedure include: knee pain for at least 3 months, evidence of a bone marrow lesion on MRI, failure of conservative treatment, presence of located pain in the oedema area. On the other hand, the main contraindications are: pain and functional limitation due to other diseases, ligamentous
laxity, varus/valgus axial deviation greater than 8 degrees, severe osteoarthritis.
The surgical procedure is based on an accurate pre-operative planning: it is very important to measure the lesion size on MRI and calculate its distance to the cortical bone on all the planes. Patient is placed supine with the affected limb elevated compared to the contralateral to allow a better view on intra-operative x-rays. The bone substitute is prepared mixing calcium phosphate granules with 3 cc of saline solution until a homogeneous material is obtained. Under fluoroscopic guidance, led by the pre-operative planning, 5 cc of calcium phosphate solution is then injected through a fenestrate cannula. The procedure is followed by an arthroscopic joint debridement in order to treat concomitant pathologies and eventually remove intra-articular calcium phosphate leakage.
Subchondroplasty has few complications represented by a leakage inside or outside knee joint during injection and failure of the procedure which can be due to inadequate indications such as diffuse osteoarthritis, an error during the surgical procedure or the presence of concomitant defects, not visible on MRI. Treatment in case of failure, which includes the persistence of knee pain and progression of arthritis, involves a total or partial Figure 2 - Pre-operative planning and some images of surgical procedure
5
knee replacement [20;21;22;23]. Material and methods
The main aim of the present cohort study is evaluating the effects of subchondroplasty associated to knee arthroscopy in reducing pain and improving in knee function in patients suffering from bone marrow lesions associated to mild or moderate osteoarthritis. The clinical outcome has been assessed at 1, 6 and 12 months follow-up. Secondarily, edema healing and bone remodelling of the affected areas have been checked at every follow-up by x-ray and MRI.
The inclusion criteria are: presence of atraumatic knee pain and functional impairment for at least 3 months; failure of conservative treatment (including NSAIDs, physical therapy, intra-articular injection with steroids or hyaluronic acid and bisphosphonates); presence of a mild to moderate osteoarthritis (Kellgren-Lawrence grade < 3); presence of BML on a loading area at MRI imaging (femoral condyles and/or tibial plateau); presence of localized pain in the BML area; written informed consent to be included into the study. Exclusion criteria comprehend: knee pain and
functional limitation related to other causes like osteonecrosis, fractures and inflammatory arthritis; the presence of a ligamentous instability; malalignment on the coronal axis greater than 10 degrees in varus/valgus; severe tri-compartmental arthritis (Kellgren-Lawrence grade 4).
Every patient included has been evaluated pre-operatively and then at each follow-up clinically and by MRI. Four validated orthopaedics scores have been used to assess patients’ symptoms and knee function: Numeric pain Rating Scale (NRS) [24]; Knee Society Score (KSS) [25]; Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) [26]; International Knee Documentation Committee (IKDC) [27].
Subchondroplasty procedure has been performed following the previously described technique and followed by an arthroscopic assessment of the intra articular structures’ conditions and the ensure the lack of any calcium phosphate leakage. A final check by x-ray has been performed and the patient could be discharged the day after surgery. Progressive weight bearing with two crutches has been allowed from the first day after the operation and a gradual recovery of complete ROM has been encouraged.
Follow-up (months)
Score
0
1
6
12
P value (0-6)
months
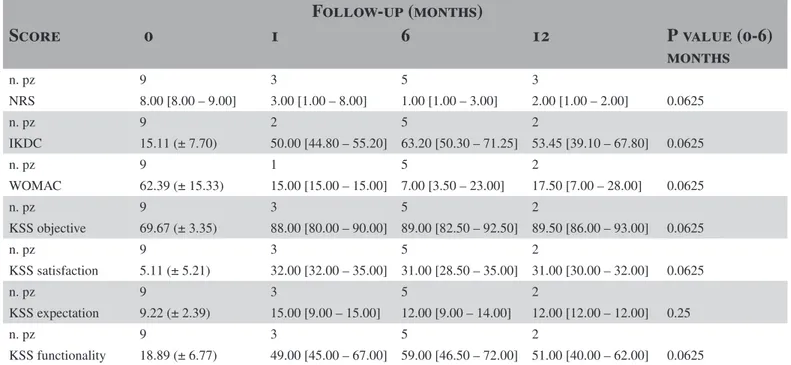
n. pz 9 3 5 3 NRS 8.00 [8.00 – 9.00] 3.00 [1.00 – 8.00] 1.00 [1.00 – 3.00] 2.00 [1.00 – 2.00] 0.0625 n. pz 9 2 5 2 IKDC 15.11 (± 7.70) 50.00 [44.80 – 55.20] 63.20 [50.30 – 71.25] 53.45 [39.10 – 67.80] 0.0625 n. pz 9 1 5 2 WOMAC 62.39 (± 15.33) 15.00 [15.00 – 15.00] 7.00 [3.50 – 23.00] 17.50 [7.00 – 28.00] 0.0625 n. pz 9 3 5 2 KSS objective 69.67 (± 3.35) 88.00 [80.00 – 90.00] 89.00 [82.50 – 92.50] 89.50 [86.00 – 93.00] 0.0625 n. pz 9 3 5 2 KSS satisfaction 5.11 (± 5.21) 32.00 [32.00 – 35.00] 31.00 [28.50 – 35.00] 31.00 [30.00 – 32.00] 0.0625 n. pz 9 3 5 2 KSS expectation 9.22 (± 2.39) 15.00 [9.00 – 15.00] 12.00 [9.00 – 14.00] 12.00 [12.00 – 12.00] 0.25 n. pz 9 3 5 2 KSS functionality 18.89 (± 6.77) 49.00 [45.00 – 67.00] 59.00 [46.50 – 72.00] 51.00 [40.00 – 62.00] 0.0625Statistical analysis of the collected data was performed as follows: every clinical score obtained at each follow-up has been compared to pre-op values through a paired t-test and Wilcoxon matched-pairs signed rank test for paired and not-paired data according with the normality of the data. Values lower than 0.05 (p<0.05) have been considered statistically significant.
Data and results
Data collection started in April 2017 and it is still in progress. Following the inclusion criteria, up to now we have enrolled 9 patients. Demographic characteristics of our patients are reported in table 1.
The mean age of the patients included in the study was about 70 years old, with women predominance (7 females and 2 males). The average Body Mass Index was 27 kg/m². All the bone marrow lesions treated were situated in the medial compartment: 5 patients on the medial femoral condyle, 2 on the medial tibial plateau and 2 patients had a combined lesion.
The preliminary collected data showed an improvement in every score at 6 months after surgery compared to the baseline. In particular, NRS scale changed from a mean value of 8 to 1, revealing a marked improvement of pain after the procedure, even though not statistically significant (p-value 0.0625). Furthermore, IKDC and WOMAC scores showed an improvement in knee function 6 months after Subchondroplasty, from 15.11 to 63.20 and from 62.39 to 7.00 respectively (p-value 0.0625); KSS in every section (objective, satisfaction and function) raised as well during the follow-up, though without statistical significance. Conclusions
The main finding of our study is a satisfying pain reduction and a good functional improvement reported after subchondroplasty procedure associated with arthroscopic debridement. NRS scale showed a marked reduction of symptoms already in an early phase after the procedure and
a further progressive improvement through the follow-up. Pain reduction seems also durable according to the low value registered at 12 months of follow-up. WOMAC and IKDC indicated a severe impairment in knee function before the treatment, while after subchondroplasty procedure, a remarkable increase of the average values associated with the performance of daily activities and joint related symptoms was found. Mean Objective KSS before surgery was about 70, quite elevated because of the strict inclusion criteria which indicate Subchondroplasty only in the absence of joint instability and severe varus/ valgus deviations; anyway, the score was not influenced by the procedure. Regarding Subjective KSS, which investigates knee pain during some activities like walking and climbing stairs, we recorded a little positive variation that can suggest an initial improvement still requiring a longer time to reach an excellent outcome. KSS “expectation” evaluation, the most subjective part of the score and influenced by some external factors, revealed not statistically significant results (p = 0.25). Results at 6 months follow-up present a p value of 0.0625, therefore they are not statistically significant, probably due to the small sample size, but still the collected data are promising for a satisfying clinical outcome after this procedure. Only two patients reached 12 months follow-up so their analysed scores are not representative of the clinical trend of all our patients.
This study presents several limitations. First of all, the lack of a control group does not allow a direct analysis of the effects of subchondroplasty procedure. Another limitation is the absence of standardization in the data collection during the follow-up; the study is still ongoing and only few patients have reached 12 months of follow-up, so our data are still incomplete. Furthermore, during the arthroscopic time after subchondroplasty, a partial meniscectomy was performed in two patients and in one case a high tibial osteotomy was added as a treatment for early osteoarthritis. These procedures can have influenced the results and brought benefits to the patient independently from the investigated treatment.
7
However, our preliminary findings are similar to the ones reported in literature and show that subchondroplasty is a mini-invasive procedure that has good results at short term in the treatment of BML associated with early and moderate osteoarthritis. This procedure can also be considered a safe surgery since we reported only few minor complications. Our patients had remarkable benefit from the procedure and they were satisfied with their outcome. Only one failure was recorded: one patient reported severe pain at 1-month follow-up and after only 3 months from the procedure a total knee arthroplasty was implanted. The failure reason is not clear yet but it could be associated with a severe grade of arthritis. This case allowed to verify that the calcium phosphate injection does not influence a following joint replacement procedure since no complications occurred during and after the implantation.
In conclusion, we can confirm that subchondroplasty is a safe, reliable and effective procedure for the treatment of bone marrow lesions associated with moderate grade of arthritis. The effects at long term still have to be verified. Further studies and more data are necessary to prove the real efficacy and durability of this emerging technique and to better define the inclusion and exclusion criteria in order to better address the patients who could benefit the most from this promising treatment.
Declaration of interests: None declared. References
1. Zanetti M, Bruder E, Romero J, Hodler J (2000) Bone marrow edema pattern in osteoarthritic knees: correlation between MR imaging and histologic findings. Radiology 215(3):835–840.
2. Thiryayi WA, Thiryayi SA, Freemont AJ (2008) Histopathological perspective on bone marrow oedema, reactive bone change and haemorrhage. Eur J Radiol 67(1):62-67.
3. Madry H, van Dijk CN, Mueller-Gerbl M (2010) The basic science of the subchondral bone. Knee Surg Sports Traumatol Arthrosc 18(4):419–433.
4. Bretlau T, Tuxoe J, Larsen L, Jorgensen U, Thomsen
HS, Lausten GS (2002) Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc 10(2):96–101.
5. Roemer FW, Frobell R, Hunter DJ, Crema MD, Fischer W, Bohndorf K, Guermazi A (2009) MRI-detected subchondral bone marrow signal alterations of the knee joint: terminology, imaging appearance, relevance and radiological differential diagnosis. Osteoarthr Cartil 17(9):1115–1131.
6. Scher C, Craig J, Nelson F (2008) Bone marrow edema in the knee in osteoarthrosis and association with total knee arthroplasty within a three-year follow-up. Skelet Radiol 37(7):609–617.
7. Bartl C, Imhoff A, Bartl R (2012) Treatment of bone marrow edema syndrome with intravenous ibandronate. Arch Orthop Trauma Surg 132(12):1781–1788.
8. Compagnoni R, Lesman J, Ferrua P, Menon A, Minoli C, Gallazzi M, Domżalski M, Randelli P. (2020) Validation of a new topographic classification of bone marrow lesions in the knee: the six-letter system. Knee Surg Sports Traumatol Arthrosc. amsudoi: 10.1007/ s00167-020-05957-y.
9. Lecouvet FE, van de Berg BC, Maldague BE, Lebon CJ, Jamart J, Saleh M, Noel H, Malghem J (1998) Early irreversible osteonecrosis versus transient lesions of the femoral condyles: prognostic value of subchondral bone and marrow changes on MR imaging. Am J Roentgenol (AJR) 170(1):71–77.
10. Kraenzlin ME, Graf C, Meier C, Kraenzlin C, Friedrich NF (2010) Possible beneficial effect of bisphosphonates in osteonecrosis of the knee. Knee Surg Sports Traumatol Arthrosc 18(12):1638–1644. 11. Meier C, Kraenzlin C, Friederich NF, Wischer T, Grize L, Meier CR, Kraenzlin ME (2014) Effect of ibandronate on spontaneous osteonecrosis of the knee: a randomized, double-blind, placebo- controlled trial. Osteoporos Int 25(1):359–366.
12. Baier C, Schaumburger J, Gotz J, Heers G, Schmidt T, Grifka J, Beckmann J (2013) Bisphosphonates or prostacyclin in the treat- ment of bone-marrow oedema syndrome of the knee and foot. Rheumatol Int 33(6):1397–1402.
13. Kraus VB, Feng S, Wang S, White S, Ainslie M, Graverand MP, et al. (2013) Subchondral bone trabecular integrity predicts and changes concurrently with radiographic and magnetic resonance imaging-determined knee osteoarthritis progression. Arthritis
Rheum. 65(7):1812-21.
14. Tanamas SK, Wluka AE, Pelletier JP, Pelletier JM, Abram F, Berry PA, Wang Y, Jones G, Cicuttini FM. (2010) Bone marrow lesions in people with knee osteoarthritis predict progression of disease and joint replacement: a longitudinal study. Rheumatology (Oxford). 49(12):2413-9.
15. Scher C, Craig J, Nelson F. (2008) Bone marrow edema in the knee in osteoarthrosis and association with total knee arthroplasty within a three-year follow-up. Skeletal Radiol. 37(7):609-17.
16. Thiryayi WA, Thiryayi SA, Freemont AJ. (2008) Histopathological perspective on bone marrow oedema, reactive bone change and haemorrhage. Eur J Radiol 67(1):62-67.
17. Jager M, Tillmann FP, Thornhill TS, Mahmoudi M, Blondin D, Hetzel GR, Zilkens C, Krauspe R (2008) Rationale for prostaglandin I2 in bone marrow oedema—from theory to application. Arthritis Res Ther 10(5):R120.
18. Laslett LL, Dore DA, Quinn SJ, Boon P, Ryan E, Winzenberg TM, Jones G. (2012) Zoledronic acid reduces knee pain and bone marrow lesions over 1 year: a randomised controlled trial. Ann Rheum Dis 71(8):1322–1328.
19. Cohen SB, Sharkey PF. (2012) Surgical treatment of osteoarthritis pain related to subchondral bone defects or bone marrow lesions: subchondroplasty. Tech Knee Surg 11(4):170–175.
20. Farr J, Cohen SB. Expanding applications of the subchondroplasty procedure for the treatment of bone marrow lesions observed on magnetic resonance imaging. (2013) Oper Techn Sport Med 21(2):138– 43.
21. JY, O’Malley MJ, Matsen Ko LJ, Cohen SB, Sharkey PF. (2016) Knee Arthroplasty After Subchondroplasty: Early Results, Complications, and Technical Challenges. J Arthroplasty. 31(10):2188-92. 22. Jungbluth P, Hakimi M, Grassmann JP, Schneppendahl J, Kessner A, Sager M, et al. (2010) The progress of early phase bone healing using porous granules produced from calcium phosphate cement. Eur J Med Res 15(5):196–203.
23. Bonadio, M. B., et al. (2017). “Subchondroplasty for treating bone marrow lesions in the knee-initial experience.” Rev Bras Ortop 52(3):325-330.
24. Hartrick CT, Kovan JP, Shapiro S. (2003) The
numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract 3(4):310–6.
25. Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH. (2012) The new Knee Society Knee Scoring system. Clin Othop Relat Res. 470(1):3-19.
26. Salaffi F, Leardini G, Canesi B, et al. (2003) Reliability and validity of the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index in Italian patients with osteoarthritis of the kneed. Osteoarthritis Cartilage. 11(8):551-560.
27. Padua R, Bondi R, Ceccarelli E, Bondi L, Romanini E, Zanoli G, Campi S. (2004) Italian version of the International Knee Documentation Committee Subjective Knee Form: cross-cultural adaptation and validation. Arthroscopy. 20(8):819-23.
28. Nakamae A, Engebretsen L, Bahr R, Krosshaug T, Ochi M (2006) Natural history of bone bruises after acute knee injury: clinical outcome and histopathological findings. Knee Surg Sports Traumatol Arthrosc 14(12):1252–1258.