Crossed
Kirschner's
wires
for
the
treatment
of
anterior
flail
chest: an
extracortical
rib
fixation
Felice
Mucilli,
Pierpaolo Camplese, GiuseppeCipollone,
Decio Di Nuzzo,Luigi Guetti,
MarcoPrioletta,
Mirko
Barone.Department of General and Thoracic Surgery, University Hospital"SS. Annunziata", Chieti, ltaly
jf open Access
§, Publish Free
Journal of Emergency Practice and
Trauma
Volume x, lssue x, 2016, p. x-x
Re(eived: 2 May 20 1 6
A(cepted: 5 June 20 1 6 Publlshed online.23 )uly 2O16
*Corresponding author: Mirko Barone, Department of General and Thoracic Surgery, University Hospital "SS. Annunziata': Vìa
dei Vestini, l,66l0o Chieti (CH),
Italy. Tell: +39087'l 358289; Fax:
+390871 358220; Email: mirSTmb@ libero.it
Competing interests: None.
Funding information: None.
Citation: Mucilli F, Camplese P, Cipollone G, Di Nuzo D, Guetti L,
Prioletta M, et al. Crossed Kirschnert
wires for the treatment of anterior
flail chest: an extracortical rib
fixation. Journal of Emergency Practice and Trauma 201 6; 2(1 ): x-x. doi: 1 0.1 5l 7lljept.2o1 6.1 I
Introduction
Thoracic trauma may be a life-threatening condition. In
the United
States and Europe,mortality
ratesin
chest trauma patients amount upto
607o.In
addition, about aquarter of deaths in polytrauma patients can be attributed
to
thoracicinjury
(1).
An
operative treatmentof
bluntthoracic
injury
is required in less than 1070 ofcases; while in the majority of cases, medical therapy or interventionalprocedures (such as the placement of a chest drainage) are needed.
Flail chest is a severe chest injury with high mortality rates.
In recent reports, it accounts for 9.1o/o (2) ofthoracic
trau-mas with a
mortality
rate of 20o/o-33Vo (3,4). Patients withsevere chest
injury
can developnot only
early dramatichttp://jept.ir
!
ro.rsrzr1"ot.2o16.11OriginalArticle
Abstract
Objective: Thoracic trauma may be a life-threatening condition. Flail chest is a severe chest injury with high mortality rates. Surgery is not frequently performed and, in Literature, data are controversial. The authors report their experience in the treatment of flail chest by an
extracortical internal-external stabilization technique with Kirshner's wires (K-wires).
Methods: From 2010
to
2015, 137 trauma patients (109 males and 28 females) with anaverage age of 58.89+19.74 years were observed. Seventeen (12.4'lo/o) patients presented a
flail chest and of these, 13 (9.497o) with an anterior one. All flail chest patients underwent early chest wall surgical stabilization (within 48 hours from the injury).
Results: ln the general population, an overall morbidity of 21.9o/o (n=30
of
137) and a30-day mortality rate of 5."1%o (n=7 of 137) were observed. By clustering the population according to the treatment (medical or interventional vs surgical), significant statistically differences between the two cohorts were found in morbidity (12.650/ovs.34.48o/o, P=0.002) and mortality rates (1.28olo vs."10.34o/o, P=0.017).ln patients undergoing chest wall surgical stabilization, with an average lnjury Severity Score of 28.3 + 5.2 and Abbreviated lnjury Score
(AlS) of 8.4 + 1.7, an overall morbidity rate of 52.9o/o (n = 9) and a mortality rate of 17.60lo (n = 3) were found. Post-surgical device removal, in local anesthesia or mild sedation. was performed 42.8+2.9 days after chest wall stabilization and no cases of wound infection, dislodgment of the wires or osteosynthesis failure were reported. Moreover, in these patients, an early postoperative improvement in pulmonary ventilation (ApaO, and ApCOr: +9.49 and -5.05,
respectively) was reported.
Conclusion: Surgical indication for the treatment of flail chest remains controversial and debated both due to an inadequate training and the absence of comparative prospective studies between various strategies. Our technique for the surgical treatment of the anterior flail chest seems to be anachronistic, but the aspects described, both in terms of technical features and of outcome and benefits (health, economic), allow to evaluate the effectiveness of this approach.
Keywords: Flail chest, Chest trauma, Kirschner's wire, lnjury Severity Score, Abbreviated lnjury Score.
consequences, but also long-term effects and disability. In
addition, flail chest also presents local (respiratory
impair-ment, shunt effect) and systemic (increased terminal
com-plement components) pathophysiological effects causing catastrophic results (5). The use ofpositive pressure
ven-tilation
(PPV) has been describedin
these patients (6). However,this
technique requires a prolonged mechani-cal ventilation which may arisein
pulmonarycomplica-tions
(pulmonary
infections, distress syndromes) withmortality
rates upto
360/o (7). Moreover, a conservative strategy does not always allow a stabilizationofthe
bonystumps, resulting
in
osteosynthesis failures, debilitating chronic pain, secondary chest wall deformities up to 64%oofcases (8).
j
by Kerman )ommons Attr rl Sciences. T //creaÌivecom article distributer 0), which permìt hlisl O 2016 The under the tervlucilli et al
Surgery
is not
frequently performed and,in
literature, data are controversial.It
is reported that less than 2o/oof
flail
chests are surgically treated (2). The reasonsof
thisunderutilization have to be found in many causes,
includ-ing unfamiliariry with the surgical technique and the lack of knowledge of the surgical indications for a prompt
pa-rietal
stabilization (9). The operative treatment,on
theother hand, is characterized by a reduction of mechani-cal ventilation, intensive care
unit (lCU)
stay,hospitaliza-tion,
tracheostomy,mortality
rates (10,11) andonly
fewreports
report
post-operativelong-term
complications (12,13). Butrib
surgical stabilization isdifficuÌt
both forthe characteristics of the fractures (lack of
uniformity
andalignment) and for clinical conditions of trauma patients. Nowadays, many repair systems (cortical and
intramedul-lary)
are adoptedin
clinical practice. The authors reporttheir
experiencein
the treatment offlail
chest by anex-tracortical internal-external stabilization technique
with
Kirshnert wires (K-wires).Methods
From 2010 to 2015, 137 trauma patients (109 males and 28 females) with an average age of 58.89+l9.74yearswere
observed in our department. Eighty-on e (59 .lo/o) present-ed a chest trauma, while others had polytrauma
(thora-co-abdominal, cranial-thoraco-abdominal).
In
almost all cases(n.
133-
97.1o/o), a blunt trauma was reported (e.g. direct trauma, precipitation) (Tablel).
On
admission,all
patients receiveda
detailed clinical,laboratory (blood chemistry, arterial blood gases),
cardio-logical (ECG, echocardiogram) and radiological
assess-ment (total body CT, abdominal ultrasound),
in
order to evaluate clinical conditions and identify any earlycompli-cations
or
undiagnosedinjury.
Moreover,all
the urgentmonitoring
maneuvers (venous incannulation, bladder catheterization, saturation and cardiacrhythm
monitor-ing) were set. The extent of trauma was stratifiedaccord-ing to the Abbreviated
Injury
Scale (AIS) and theInjury
Severity Score (ISS).
Thoracic
cageinjuries
were observedin ll3
patients(82.48%o)
with
an average of 3.2 fractured ribs per patient (mean 1.62 on the right and 1.75 on the left side). Sternalfractures (24, 17.5%), clavicle fractures (19, 13.97o) and vertebral ones (15, 10.97o) were also associated. Seventeen (12.41o/o) patients presented a
flail
chest and of these, 13 (9.a9%o) had an anterior one due to the presence ofmul-tiple
rib
fractureswith or without
a sternal one causing a paradoxical movementof
the thorax. Considering the extent and the dynamics of impact, parietal traumas were associatedwith
intrathoracic organ injuries such as pul-monary contusion (61, 44.5o/o), pulmonary laceration (9,6.67o), pneumothorax (46, 33.6%o), hemothorax,
hemome-diastinum or hemopericardium. Liver and spleen lacera-tions (13,9.5%) and diaphragmatic rupture (5,3.670) were reported in thoraco-abdominal polytraumas.
Thirty-four
patients (24.8Vo) underwent urgency surgery (thoracic, abdominal or both), while the remainings were subjected to medical therapy (79,57.7Vo) or tointerven-tional
procedures suchas
chestdrain
placement (24,17 .5o/o) (Tab\e 2).
All
flail
chest patients underwent early chest wall surgi-cal stabilization (within 48 hours from the injury). In caseof anterior paradoxical movement, we proceeded
with
anexternal-internal substernal
surgical stabilization
withcrossed K-wires by anchoring them to healthy ribs imme-diately below
or
above those fractured.With
the patientin
the supine position, the technique involves a crossed placement (i.e. "Saint Andrew's cross") of these devices via aminimally
invasive subxiphoid access or via a bilateralvideo thoracoscopic one (Figure
l).
In
open surgery, asubxiphoid incision is performed
in
orderto
access intothe anterior mediastinum and to proceed with a
blind-fin-gered dissection between the endothoracic fascia and the parietal pleurae. Protecting the pericardium with the back of the hand, K-wires are inserted laterally and beyond the
fractured ribs
with
an oblique course and crossing thembehind the sternum. The ends of these devices emerge to the skin in correspondence of the intercostal space
imme-diately above or below the
rib
stumps. The access and the mediastinal digital dissection allow a rapid stabilizationof
the chest wall with the patient in bipulmonary ventilation
and a chest drainage is usually not required. On the other hand, the minimally invasive bilateral thoracoscopic
tech-nique
for
anterolateralflail
chests requires a single-lungventilation and placement ofa chest tube due to the access
into the pleural cavity (Figure 2) as well as to drain an he-mothorax or suturing lung lacerations.
Results
In
the general population, an overallmorbidity
ol
21.9o/o(30 of 137) and a 30-day mortality rate of5.17o (7
of
137) were observed. Anemia, respiratory failure and arrhyth-mias werethe
earlymost
common complications. On admission, an average ISSof
15.60t 10.76 and an AISof
5.8013.12 were calculated. The average hospital stay was 7.92+5.53 days (Table 1).
By clustering the population according
to
the treatment (medical or interventional vs. surgical),in
the first group the average hospital stay was 5.47 + 4.33, while in thesec-ond
it
was 11.26+5.25 (P<0.001). Moreover, significant statistically differences between the two cohortsin
mor-bidity
(12.650/0 vs. 34.48o/o, P=0.002) andmortality
rates (1.28o/ovs. 10.34o/o,P= 0.017) were found (Table 3). Inpar-ticular, regarding the patients undergoing chest wall sur-gical stabilization (n = 17), the frequencies appear higher;
in
fact, an overallmorbidity
rate of 52.9o/o (n=
9), mostlyattributable
to
anemia
and
post-operative respiratoryfailure (Clavien-Dindo score=3), and a
mortality
oneof
77.60/o (n= 3) were noted. This can be explained
consider-ing patient's clinical conditions and the early respiratory and metabolic effects that develop
in
flail
chest patients, rather than the surgical technique itself.In
fact, the aver-age ISS was 28.3 +5.2with
an AIS of 8.4 + 1.7. Post-sur-gical device removal, in local anesthesia ormild
sedation, was performed 42.8!2.9
days after chestwall
Niucilli et al
Table 1. General population characteristics
Variable Sex Male Female Age Kind of trauma Blunt Open Type of trauma Thoracic Thoraco-abdominal Head-thoracic Ats ISS Treatment Medical Surgical lnterventional Hospital stay Morbidity o/o No. 109 28 79.6 20.4 Head-thoracic-abdominal 133 4 81 34 14 8 58.89!19.74 5.8+3.12 15.6+ 10.76 7.92+5.53 97.1 2.9 59.1 24.8 10.2 5.8 57.7 24.8 17.5 21.9 (16.00-98.00) (2.00-r 2.00) (4.00-s0.0) (2.00,33.00) n = 11 Anemia n = 7 Respiratory failure n = 4 Pneumonia n = 2 Myocardial infarction n = 2 Sepsis n=2RenalFailure n = 1 Ventricularfibrillation n=lAtrial fibrillation 79 34 24 30
Abbreviations: AlS, Abbreviated lnjury Scale; lSS, lnjury Severity Score.
Table 2. Trauma characteristics
No. of patients o/o
Thoracic cage injuries
Rib fractures Sternal fractures Clavicle fractures Vertebral fractures Scapular fractures Flail chest"
lntrathoracic organ injuries Pulmonary contusion Lung laceration
Great vessels injury
Pneumothorax Hemothorax Hemopericardium Diaphragmatic injury
lntraabdominal organ injuries
Hepatic contusion/laceration
Spleen laceration lntestinal laceration Kidney injury
" n =1 3 anterior; n = 4 antero-lateral.
tion
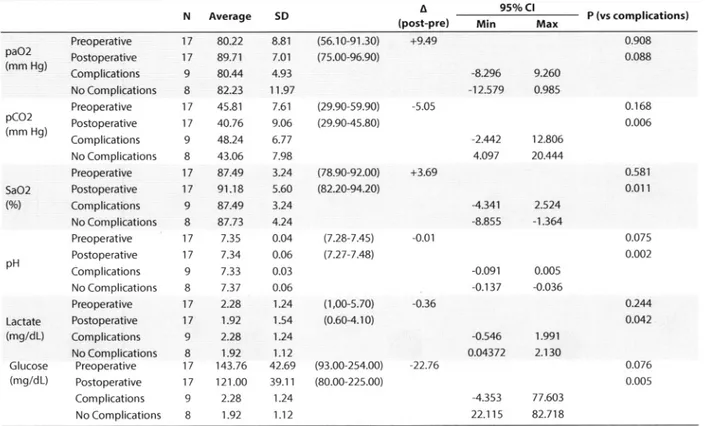
and no cases of wound infection, dislodgment of the wires or osteosynthesis failure were reported. Cumulative reoperation rate was 0.070 (Table 4).In
the second partof
the study, a descriptive analysisof
changes
in
respiratory (paO,, pCO,, SaO,) and metabolicparameters (pH, lactate, glucose), derived from pre-oper-ative and post-operpre-oper-ative
(third
P.O"D.) arterial blood gasanalyses, was performed
in
K-wire
patients. Data shows surgery correlateswith
an early improvementin
pulmo-nary ventilation (ApaO, and ApCO,: +9.49mm
Hg and -5.05 mm Hg, respectively) (Figure 3). Moreover, thebi-variate analysis demonstrates that postoperative
compli-cations correlate
with
thecount of
postoperative bloodgas metabolites rather than the preoperative ones; in other
words, an early
poor
adaptation and a lackof
improve-ment of the aforesaid parameters are predictors of postop-erative morbidity (Table 5).Discussion
With
the adventof
the internal pneumatic stabilization and the early report by Avery et al (14)in
1956, the man-agementof
chest trauma veered towards non-operative treatments, although sincefrom
the outsetthe
related-complications were clear (15). Today, a renewed interest insurgical stabilization techniques occurs.
In
2002, Tanakaet
al
(16) reported the benefitsof
surgeryfor flail
chesttreatment.
Although
these results are encouraging, butsurgical stabilization of the
flail
chest remains anunde-rutilized
procedure dueto multiple
factors, such asun-familiarity
and lack of knowledge of surgical indications (7,9,17). Moreover, surgical indicationfor
the treatmentofflail
chest remains subject ofextensive debate. Lardinois et al (18) reported 66 patients with anterolateral flail chest113 24 19 15 3 17 82.48 17.5 13.9 10.9 2.2 12.14 61 9 4 46 28 7 5 44.5 6.6 2.9 33.6 20.4 5.1 3.6 2.9 6.6 u.t 2.9 4 9 I 4 Average
i'{ucilli et al
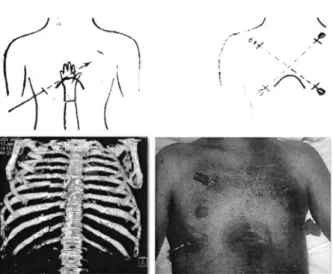
Figure I. Surgical technique for the stabilization ofthe anterior flail
chest with crossed Kirschner's wires (subxiphoid access).
Figure 2. Surgical technique for the stabilization of the anterior flail
chest with crossed Kirschner's wires (videothoracoscopic access).
who underwent 3.5 mm-plate surgical stabilization. The authors posed surgical
indication
in
non-intubated pa-tientswith
refractory respiratory failure,in
patients with flail chest disalignment,in
intubated patients without se-vere pulmonary contusion or brain injuries whodid
not require prolonged intubation and in patients requiring an emergency thoracotomy due to the presence ofintratho-racic organ injury.
In the 2013 Eastern Association for the Surgery of Trauma guidelines (5), the only
two
indicationsfor
surgicalfixa-tion
are the respiratory declineofa
flail chest patientfail-ing to wean from the ventilator and the need to perform a
thoracotomy regardless the presence
ofa
flail chest.But, the same guidelines recommend
that
an earlypro-phylactic chest stabilization should be avoided because
it
does not show any benefit. Moreover, the presence of
ex-Table 3. lndependent samples t test (medical and interventional/surgical treatment vs outcome)
tensive pulmonary contusion is a relative contraindication for surgery, as these patients require prolonged mechani-cal ventilation (19).
However, at the worsening of patient's ventilation or at the
partial resolution of contusions, surgical stabilization can be envisaged (20); while,
in
patientswith
severe isolated parietal injury, an early surgical fixation (within 72 hours)can reduce the
risk of
potential ventilator-relatedinfec-tious complications,
ICU
stay and can prevent the onsetof post-traumatic restrictive pulmonary syndromes.
An-other indication for surgical stabilization is the extension and locationof
theflail
chest.In
fact,in
young patientsin
case of an extended anterolateralflail
chest, surgery isimmediately indicated, even in the absence of respiratory complications, due
to
thehigh risk
of dislocation of therib
stumps. Posterior parietal defects are rarely surgically treated, except for the presence ofwedging fractured lineswithin
the pleural cavity that may lacerate intrathoracicorgans. Moreover, respiratory dynamics is ensured by the
bony structures of the shoulder girdle and the action
of
the trapezius, serratus and Iatissimus dorsi.
In
our
experience, we takeinto
accountfor
surgicalsta-bilization the extent
ofthe
flail chest, the onset ofrespira-tory
failure or muscle fatigue and the presence of a con-comitant indication for urgency surgery for other reasons. We also believe that a wait and see strategy could increasethe risk of
morbidity
and mortality. Moreover, older pa-tients (> 70 years) do not have negligible comorbidity (i.e. COPD, pulmonary emphysema) and need early surgical chest stabilization avoiding serious deterioration of their clinical conditions. Therefore, the early changes ofrespi-ratory parameters pose surgical indication, except for the presence of severe organ
injury
(brain, diffuse pulmonarycontusions).
In literature, many surgical fixation techniques are
report-ed
with
several devices that can be divided into: devicesfor
cortical
stabilization (cerclagewires and
clamping, screw fixation ones) and those for intramedullary stabili-zation (K-wires, Rehbein plate, rib splints) (17).The rationale
is the
mechanicalfunction
restorationof
the
chestwall.
Amongthe
cerclage techniques,histori-cally, Paris et al (21) introduced a 40 cm-length temporary struts
with
four
or
five holesto
anchorto
the cortexof
fractured ribs.
The experiences.by |udet
(22)
andby
Sanches-Lloret etal (23) are just historical notes. The modern evolution
of
cortical fixation for fractured ribs has led to the
develop-ment
of
anatomically shaped plates-
U-plate (24),ana-__/
\
i. ,,,. ,*
l'..'
i *^.6
#
{\
95o/oClN
o/o
Average
SD (A) P (y.21Min Max
Hospital stay (days)
Morbidity rate (o/o)
Mortality rate (o/o)
Medical lnterventional/Surgical Medical I nterventional/Surgical Medical lnterventional/Surgical 79/137 s8/137 10/79 20/s8 1/78 6/s8 57.66 42.34 12.65 34.48 1.28 10.34 5.47 11.26 -7.412 -8.64 -4.168 4.43 0.000 0.002 0.0'17 4.33 5.42
4 Journal of Emergency Practice and Trauma, 2016, x(x), x-x
/\
(
Mucilli et al
Table 4. Clinical finding and post-operative outcome in flail chest patients undergoing surgical stabilization
N
Average
o/o o s o o o co*-op I ere-op IFlail chest patients
Morbidity Mortality ISS AIS Post-surgical device removal(days) Reoperation rate 17 9/17 3/17 52.9 17.6 n = 13 anterior n = 4 lateral 28.3 + 5.2 8.4+ 1.7 42.8 + 2.9
tomical
rib
plates (3,25,26). Nowadays, these latters can also be fixedvia
aminimally
invasive technique (mini-mally invasive plate osteosynthesis orMIPO)
(27).Intramedullary
implants have also been described.K-wires have been reported in numerous reports
with
good results, although casesofrotatory
instability (28) or dislo-cation (29) have been described. In this regard, preformedrib
splints (30) have been introduced for fracture fixationensuring both radial and rotational stabiliry;
in
addition, they do not present risksof migration
(31,32) as anex-tremity
is fixed to the proximalportion
of the fracturedrib.
Finally,an
emerging conceptfor
treatmentof
rib
fractures is the useof
bioabsorbable materials (33). Fi-nally, Liovié et al (34) have reported a new experimental technique using an intramedullary telescoping splint an-chored by bone cement.Our proposed technique for the treatment of the anterior
flail
chest may appear anachronistic,but
the procedure presents some peculiarities that should be consideredin
Table 5. Blood gas analysis vs post-operative complications
P--"pI t"'u"pE 10 20 30 40 50 60 70 Posfop I rre-"p ! 0 80 $ 1@ 110 120 130 140
Figure 3. Early postoperative changes in respiratory and metabolic parameters in flail chest patients.
case of a polytrauma patient.
First of all,
it
is of rapid execution and,in
the subxiphoid technique,it
does not require a pleural drainage. Thepa-tient
is placedin
the supine position, therefore,limiting
any movements or tractions on the spine and the organs. Finally, we
did
not record any procedure-relatedcompli-cation (rejections, infections, decubitus) or osteosynthesis failure. The insertion of a 8
mm-K-wire
can be safely per-formed both in open technique (the device flows betweenthe operatort hand and the endothoracic fascia) and
in
the video assisted one. The removal is typically 40 days after the surgery under local anesthesia ormild
sedation. The result is the absence of foreign bodies or permanentimplants
in
the
chest. Moreover,it
is
also economicalwhen compared
to
the costsof
intramedullary fixation (ORIF);in
fact, for the latter the amount isfrom
$15 00095o/o Cl
N Average
SD P (vs complications) paO2 (mm Hg) pCO2 (mm Hg) SaO2 Lactate (mg/dL) Glucose 80.22 89.7"1 80.M 82.23 45.81 40.76 48.24 43.06 87.49 91.18 87.49 87.73 7.35 7.34 7.33 7.37 2.28 1.92 2.28 1.92 143.76 121.00 2.28 1.92 8.81 7.O1 4.93 11.97 7.6"1 9.06 6.77 7.98 3.24 s.60 3.24 4.24 0.04 0.06 0.03 0.06 1.24 1.54 1.24 1.12 42.69 39.1 1 1.24 1.12 +9.49 -5.05 +3.69 -0.01 -0.36 -22.76 Min -8.296 -12.579 -2.442 4.097 -4.341 -8.8s5 -0.091 -0.137 -0.546 o.04372 -4.353 22.115 Max 9.260 0.985 12.806 20.444 2.524 -1.364 0.005 {.036 1.991 2.1 30 77.603 82.718 0.908 0.088 0.168 0.006 0.581 0.01 r 0.075 0.002 o.244 o.o42 0.o76 0.00s (vù pH Preoperative Postoperative Complications No Complications Preoperative Postoperative Complications No Complications Preoperative Postoperative Complications No Complications Preoperative Postoperative Complications No Complications Preoperative Postoperative Complications No Complications Preoperative Postoperative Complications No Complications 17 17 9 8 17 17 9 8 17 17 9 8 17 '17 o 8 17 17 9 8 17 17 9 8 (s6.1 0-91 .30) (7s.00-96.90) (29.90-s9.90) (29.90-4s.80) (78.90-92.00) (82.20-94.20ì. (7.28-7.45) (7.27-7.48]' (1,00-s.70) (0.60-4.10) (93.00-2s4.oo) (80.00-22s.00) (mg/dL) 0 ANlucilli et al
to $30000 (3s,31).
Postoperative complication rate was 52.9o/o
(n=
9of
17)but none related
with
surgery, except 2 cases of acute re-spiratory failure.In
one of these, subjected to emergencystabilization
for
an extended iatrogenicflail
chest by an external cardiac massage, the etiology referred to a diffuse parenchymal injury.In
theflail
chest study arm, we ob-served a 17.60/o mortalily rate (n= 3 ofl7),
a slightly lower occurrence thanto
those reportedin
the literature (34). Extracortical surgical chest wall stabilization with K-wires results in an early improvement of the respiratory param-eters. As reported,in
our experience we noticed asignifi-cant improvement
in
arterial blood gas parameters from thethird
post-operative day (ApaO, and ApCO,: +9.49 and -5.05, respectively) and the bivariate analysis demon-strated the complication rate correlateswith
the countof
postoperative blood gas metabolites rather than the pre-operative ones;
in
other words, an early poor adaptation and a lack of improvement of the aforesaid parameters are predictors of postoperative morbidity.Conclusion
Although
these encouraging results, surgical indicationfor
the treatment offlail
chest remains controversial and debated dueto
both an inadequatetraining
and theab-sence of comparative prospective studies between various
strategies. Nowadays, a gold standard technique is not still
present, resulting in a widespread fragmentation of expe-riences and results.
Our
techniquefor
the surgical treat-ment of the anteriorflail
chest seems to be anachronisticin an era of strong technological innovations. Despite this, the aspects described, both
in
terms of technical features and of outcome and benefits (health, economic), allow to evaluate the effectivenessofthis
approach.Ethical issues
The article does not contain any research with human par-ticipants performed by the authors. For this type of study, no formal consent is required.
It
is an anonymous one.Authors' contributions
All
authors participated in data collection, statisticaÌ anal-ysis and text writing.References
l.
Clark GC,
SchecterWR
Trunkey
DD.
Variables affecting outcomein
blunt chest trauma:flail
chest vs.pulmonary contusion. I Trauma 1988; 28(3): 298-304. doi:
10. I097100005373- 198803000-00004.
2.
Cannon RM, Smith IW Franklin GA, Harbrecht BG, Miller FB, Richardson ]D. Flail chest injury: are we making anyprogress? Am Surg 2012; 7 8(4): 398-402.
3.
fayle CB Allain G, Ingrand R Laksiri L, Bonnin E,Hajj-Chahine J, et al. Flail chest
in
polytraumatized patients: surgical fixation using Stracos reduces ventilator time and hospital stay. Biomed Res Int 2015; 2015:624723. doi: 10.t155120r51624723.4.
Fowler TT, Taylor BC, Bellino MJ, Althausen PL. Surgicaltreatment of flail chest and rib fractures. I Arn Acad Orthop
Surg 20 14; 22(12): 7 5 | -60. doi: I 0.5435/|A AOS -22 - 12 -7 51.
5.
Simon B, Ebert J, Bokhari F, Capella l, Emhoff T, HaywardT
3rd, et al. Managementof
pulmonary contusion andflail
chest:an
Eastern Associationfor
the Surgery of 'liauma practice management guideline.I
Trauma Acute Care Surg 2012; 73(5 Suppl 4): 535l-61.doi:
10.1097/TA.0b0l3e3l8270l9fd.
6.
Gunduz M, Unlugenc H, Ozalevli M, Inanoglu K, AkmanH.
A
comparative studyof
continuous positive airway pressure (CPAP)and
intermittent positive pressureventilation (IPPV) in patients with flail chest. Emerg Med J 200 5 ; 22(5) : 325 -9. doi: I 0. I 1 36/emj. 20 0 4.0 t97 86.
7.
RichardsonfD,
FranklinGA,
HefileyS,
Seligson D.Operative fixation of chest wall fractures: an underused procedure? Am Surg 2007 : 7 3(6): 591 -6.
8.
Landercasperf,
CogbillTH,
Lindesmith LA. Long-termdisability after flail chest injury. I Trauma 1984; 24(5):
410-4.
9.
Mayberry JC, Ham LB, Schipper PH, Ellis TJ, Mullins RI.Surveyed opinion of American trauma, orthopedic, and
thoracic surgeons on rib and sternal fracture repair. I Trauma
2009; 66(3): 875-9. doi: I 0. I 097lTA.0b0 1 3e3 I 8 I 90c3d3.
10.
Cataneo Af, Cataneo DC, de Oliveira FH, Arruda KA, El Dib R, de Oliveira Carvalho PE. Surgical versus nonsurgical interventions for flail chest. Cochrane Database Syst Rev2015; (7): CD009919. doi: 10.1002/14651858.CD009919. pub2.
11.
Leinicke fA, Elmore L, Freeman BD, Colditz GA. Operative management ofrib
fracturesin
the setting of flail chest:a systematic review and meta-analysis. Ann Surg 2013;
258(6): 914-21. doi: 10.1097/sLA.0b013e3182895bb0.
12.
Nirula R, Allen B, Layman R, Falimirski ME, Somberg LB.Rib fracture stabilization in patients sustaining blunt chest
injury. Am Surg 2006; 72(4): 307 -9.
13.
Mayberry |C, Kroeker AD, Ham LB, Mullins Rl, Trunkey DD. Long-term morbidiry pain, and disabiliry after repair of severe chest wall injuries. Am Surg 2009; 75(5): 389-9a.14.
AveryEE, Benson DW, Morch ET. Criticallycrushed chests;a new method of treatment with continuous mechanical hyperventilation to produce alkalotic apnea and internal pneumatic stabilization. ] Thorac Surg 1956;32(3): 291-311.
15.
Ginsberg RJ, Kostin RF. New approaches to the managementofflail chest. Can Med Assoc I 1977; I 16(6): 613-5.
16.
TanakaH,
YukiokaI
YamagutiY,
Shimizu S, GotoH,
MatsudaH,
et al.
Surgical stabilizationof
internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma 2002;s2(4):727-32.
17.
Fitzpatrick DC, Denard PL Phelan D, Long WB, Madey SM, Bottlang M. Operative stabilization of flail chest injuries: reviewof
literature and fixation options. EurI
Trauma Emerg Surg 2010; 36(5): 427-33. doi: 10.1007/s00068-010-oo27-8.18.
Lardinois D, Krueger T, Dusmet M, Ghisletta N, GuggerM,
Ris HB. Pulmonary function testing after operative stabilisationof
the
chestwall for flail
chest.Eur
I Cardiothorac Surg 2001; 20(3): 496-501.19.
Richardson |D, Adams L Flint LM. Selective managementof flail chest and pulmonary contusion. Ann Surg 1982;
t9 6(4): 481 -7 . doi: I 0. I 097100000658- I 982 I 0000-000 1 2.
20.
Tzelepis GE, McCool FD, HoppinFG
Ir.
Chest wall distortion in patients with flail chest. Am Rev Respir DisI 989; 140( 1 ): 3 1 -7. doi: I 0. 1 164/ajrccm I 140.1.31.
Mucilli et al
21.
Paris F, Tarazona V, Blasco E, Canto A, Casillas M, Pastor |, et al. Surgical stabilization oftraumatic flail chest. Thorax1975; 30(5): 52r -7. doi: 10. I I 36lthx.30.5.52 1.
22.
]udet R. Osteosynthese costale. Rev Chir Orthop Reparatrice Appar Mot 1973; 59(Suppl 1):334-5. [in French].23.
Sanchez-Lloret J, Letang E, Mateu M, Callejas MA, CatalanM, Canalis E, et al. Indications and surgical treatment of the traumatic flail chest syndrome. An original technique. Thorac Cardiovasc Surg 1982; 30(5): 294-7. doi:10.1055/s-2007-t0224t0.
24.
Sales IR, Ellis TL Gillard l, Liu Q, Chen JC, Ham B, et al.Biomechanical testing of a novel, minimally invasive rib fracture plating system. J Trauma 2008;64(5): 1270-4. doi:
10. 1 097lTA.0b0 13 e3 r804a7 fd5.
25.
RamponiR
Meredith GT, BendinelliC,
Sòderlund T.Operative management
of
flail
chestwith
anatomical locking plates (MatrixRib). ANZ J Surg 2012;82(9):658-9.doi: 10. I I I l/j. I 445 -2197.20'\2.06 1 59.x.
26.
BottlangM,
Walleser S, NollM,
Honold S, Madey SM, Fitzpatrick D, et al. Biomechanical rationale and evaluation of an implant system for rib fracture 6xation. Eur I Trauma Emerg Surg 2010;36(5):417 -26. doi: I 0. 1 007/s00068-0l0-0047-4.
27.
Bemelman M, van Baal M, Yuan JZ, Leenen L. The role ofminimally invasive plate osteosynthesis
in rib
fixation: areview Korean J Thorac Cardiovasc Surg 2016; a9(1): 1-8.
doi: 1 0.5090/kjtcs.20 16.49. l. l.
28.
Engel C, Krieg |C, Madey SM, l.ong WB, Bottlang M.Operative chest wall fixation with osteosynthesis plates. I Trauma 2005; 58(l): 181-6.
29.
ShahTf. On
internal fixationfor flail
chest.I
Thorac Cardiovasc Surg 1996; I 12(3): 849-50.30.
HelzelI,
Long W, Fitzpatrick D, Madey S, Bottlang M. Evaluation of intramedullaryrib
splints for less-invasive stabilisation of rib fractures. Injury 2009; 40(10): 1104-10.doi: I 0. 1 016/j.injury.2009.06.004.
31.
GranhedHP,
PazookiD.
A
feasibility studyof
60consecutive patients operated for unstable thoracic cage.
J Trauma Manag Outcomes 2014; 8(1): 20. doi: 10.1186/ sl 3032-0 14-0020-2.
32.
Marasco SR Davies AR, Cooper ], Varma D, Bennett V, NevillR, et al. Prospective randomized controlled trial ofoperative
rib fixation in traumatic flail chest.
I
Am Coll Surg 2013;2t6(5): 924-32. doi: 1 0. I 016/j.jamcollsurg.2012.12.024.
33.
Nolasco-dela
Rosa AL, Mosiioz-Montes R, Matehuala-Garcia J, Rom6n-Guzmàn E, Quero-Sandoval F,Reyes-Miranda AL. Unstable thorax fixation with bioabsorbable
plates and screws. Presentation ofsome cases. Cir Cir 2015;
83( 1 ): 23-8. doi: 10. l0 16/j.circir.20 15.04.019. [in Spanish]
34.
Liovic B Sutalo ID, Marasco SF. Fixation of a human rib by an intramedullary telescoping splint anchored by bonecement. Comput Methods Biomech Biomed Engin 2016;
19(12): 1297 -305. doi: I 0.1080/|0255842.20|5.I|31979.