Gut, 1976, 17, 501-505
Abnormalities of sodium
excretion
and
other
disorders of
renal function
in
fulminant
hepatic
failure
S. P. WILKINSON, V. A. ARROYO', HELEN MOODIE, L. M. BLENDIS2, AND ROGER WILLIAMS
From the Liver Unit,King's College Hospital and Medical School, Denmark Hill, London
SUMMARY Renal function was evaluated in 40 patients with fulminant hepatic failure. Theywere divided intotwogroups onthe basis ofglomerular filtrationratesgreaterthan 40 ml/minorless than 25 ml/min. A number of patients in group 1 had markedly abnormal renal retention of sodium
together withareduced freewaterclearance and low potassium excretion which could be explained by increased proximal tubular reabsorption of sodium. The patients ingroup 2had evidence that renal tubularintegritywasmaintained when the glomerularfiltrationratewas > 3ml/min (functional renal failure), butevidence of tubular damagewaspresentwhen thiswas <3ml/min (acute tubular necrosis).
A previous study of 48 patients with fulminant hepatic failure showed that 38hadevidence ofrenal impairment associated with a particularly poor prognosis (Wilkinson et al., 1974a). A number of patients from that study whose renal function other-wise appeared to be normal showed marked renal retentionof sodium.Inthepresentserieswestudied an additional consecutive group of40 patients to establish more precisely the functional changes occurring within the kidney, particularly the renal handling of sodium when the glomerular filtration rateis relatively well maintained.
Methods
Fulminant hepatic failure was caused by viral hepatitis in 10 patients (two beingHBAg positive), multiple anaestheticexposures tohalothaneinnine, self-induced overdose with paracetamol
(16),
acute Budd-Chiari syndrome (one), hypersensitivity to pyrazinamide (one), acute fatty liver ofpregnancy(two),and poisoning withAmanitaphalloides(one). The patients, 29 female and 11 male, were aged between 15 and 66 years and all 40 had severe hepatic encephalopathy. The patients were all well hydrated and none hadpreviouslyreceiveddiuretics or had a history ofrenal or cardiac disease. No fluids containing sodium were given for one hour
'Present address: Liver Unit,Hospital ClinicoyProvincial, Barcelona, Spain.
2Presentaddress:DepartmentofGastroenterology, Central Middlesex Hospital, London,N.W.10.
Received forpublication5April1976
before the study. Arterial blood pressure, central venous pressure, and respiratory rate had been constant in all cases for at least six hours and no patientwasbleeding.
Renal functionwasevaluated by inulin clearance (glomerular filtration rate), para-aminohippurate clearance (effective renal plasma flow), free water clearance (a measure of the patient's ability to excrete a waterload), urinary sodium andpotassium excretion, andmicroscopy of the sediment ofafresh urinespecimen. Eachpatientwasgivenawaterload of 20 ml/kg body weight intravenously as 5% dextrose, over one hour. This procedure never reducedplasmasodiumconcentrationby morethan 3mmol/l. Inulin andpara-aminohippuratewerethen immediately infused intravenously, initially as a loading dose followedbyaconstantinfusion. Urine collections weremade from a three-way indwelling Foley bladder catheterevery 30minutes, ensuring by airdisplacement that the bladder was empty. Free water clearance was calculated as the difference betweenmaximumurinaryflowand osmolar clearance (Smith, 1956) for the30 minuteperiod ofmaximal diuresis after the water load wasgiven. Values for inulin and para-aminohippurate clearance,
cor-rected to abody surfaceof 1-73sq.m were calculated from the mean of three consecutive 30 minute clearances-the first beginning30 minutes after the loading doses of inulin and para-aminohippurate. Blood samples for osmolality, inulin, and para-aminohippurate concentrations were taken at the midpointof each clearance period.Inulin and para-501
I 3M Iq 2250 z 0 200 F w u X 150 w 0 100. o 0 LO 50 28 I PONTS 0 0 0 50 100 150 2CO
GLOMERL-ARFILTRATIONRATE
ML/MIN
Fig. 1 Relationship between sodium excretion and
glomerularfiltrationrateinthecomplete series.
aminohippurate concentrations weredetermined by
standard biochemical methods (Varley, 1967), osmolality bydepression of thefreezing point, and sodium and potassium by flame photometry. The
water load was not given to patients with urine volumesofless than 25 ml/h, and inseverelyoliguric patients(urine volume less than 12 ml/h) glomerular filtration ratewasdetermined from theendogenous
creatinine clearance based on 12 or 24 hour urine
collections. In the latter group of patients
para-aminohippurate clearance wasnot measured. In all, 52 studies were carried out in the 40 patients.
Results
Glomerular filtration rate and urinary sodium
excretionrangedwidelywith values from less than 1
to 176ml/minand from less than1to295mmol/24
hours respectively. Statistical analysis showed a
highly significant correlation between these two measurements (r = 049,p < 0001). However,the series washeavily weighted bythelarge number of patients with a markedly reduced glomerular
filtrationrateoflessthan25ml/min,allof whom had values forurinary sodiumexcretion of less than 25 mmol/24 hours.None of thepatientshadglomerular filtrationratesbetween 25 and 40ml/min, and in the 18 patients whosevaluesweregreaterthan 40 there
was nocorrelation between thetwovariables (Fig.1). The patientshave therefore been grouped into those with a glomerularfiltration rate ofgreater than 40 ml/min (group 1) and those in whom this was
reducedtoless than 25ml/min(group2).
GROUP 1 (PATIENTS WITH GLOMERULAR
FILTRATION RATE GREATER THAN 40 ML/MIN)
(Table 1)
All 18 patients in thisgroup were receivingatleast 100 mmolsodiumdaily (range 100-300 mmol)given inthe formoffreshfrozen plasmaastreatmentfor their coagulation disturbance. A comparison of urinary sodium excretion and sodium intakeshowed that in 10 patients (sodium retainers) renal retention ofsodiumwasmarked, withapositivebalance ofat
least 100 mmolonthedayofinvestigation. Four of
these patientswereadmittedtothis unit withinone
dayoftheonsetof fulminant hepatic failure andnone
of them hadanegative sodiumbalance before their
renal function was investigated. In the other six a
previous negative sodium balancewasmostunlikely
asthey hadnotreceived diuretics or lost sodiumby vomiting. A latertestof sodium excretion intwoof the sodium retainers and the remaining eight in
group 1 showed that they had a normal sodium excretionoronly moderate sodium retention(sodium
Table 1 Renalfunction in patients withglomerularfiltration rate > 40ml/min
Glomerular Renal Free Plasma Sodium Total Urinary Plasma Potassium Urinary ArterialpH filtration plasma water sodium intake sodium sodium potassium intake potassium
rate flow clearance concentra- (mmol/ loss* excretion concentra- (mmol/ excretion
(ml/min) (ml/min) (ml/min) tion 24h) (mmol/ (mmol/ tion 24h) (mmol/
(mmol/1) 24h) 24h) (mmol/l) 24h) Sadium excretors Mean 113 730 6-5 133 175 128 123 3-6 70 53 7-49 ± SD 37 337 3-7 5 57 72 69 05 39 22 0-04 Sodiumretainers Mean 87 559 0-8 131 193 31 9 3-7 60 50 7-49 i SD 40 271 1.9 7 67 44 8 05 53 50 0-05
*Includesurinary lossandgastric aspirate.Does notinclude stoolandinsensiblelosses.
a '
7
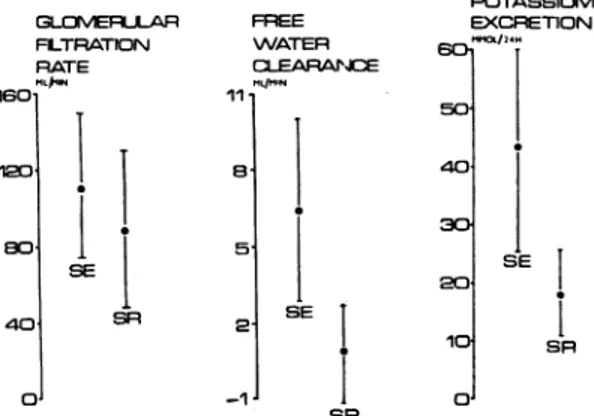
Abnormalities ofsodium excretion and other disordersofrenal functioninfulminanthepaticfailure GLCMERLLAR FLTRATION RATE MLk$ 160 120 80 40 ol *1 IC SR. FREE WATER CLEARACE 111 E l 5. 2--1 I SE 40 30 20 SR 10 OJ POTASSIUM EXCRETION 24*H SE SR
Fig. 2 Comparison ofglomerularfiltrationrate,free waterclearance, and potassium excretion in patients with glomerular filtrationrate > 40ml/min. Values for potassium excretion in patientswith arterial pH > 750 arenotincluded(SE-sodiumexcretors,SR-sodium retainers;meanvalueswithstandard deviations shown)
excretors). In mostcasesexcretion matched intake, andnopositive balance exceeded 100 mmol/day.
Acomparison of other renal functiontestsof the sodium retainers and sodium excretors showed a
similarrangeofvalues forglomerular filtrationrate
(Fig. 2), renal plasma flow, plasma sodium
concen-tration, and filtered load of sodium (the product of glomerular filtration rate and plasma sodium concentration). In all cases systolic arterial blood pressureexceeded105mmHg, withacentralvenous pressure ranging from 1 to6cm H20. There were
differences, however, in the measurements of free
water clearance, the mean value in the sodium excretors being significantly higher than that found inthe sodium retainers (mean 6'5 ml/min ± 3*7 SD,
mean 0-8 ml/min ± 1-9 respectively, P < 0-001)
(Fig. 2).
There was a statistically significant relationship
between free water clearance and filtered load of sodium(r= 060,p < 0.005)inthecompletegroup,
although four patients who could not excrete free
waterhad relativelyhigh values for the latter (greater than 11mmol/min).
The sodium excretors and sodium retainers had similarmeanvalues forurinary potassium excretion, but whenpatients witha severealkalosis(arterial pH
greaterthan750)wereexcluded,significantly lower
values for potassium excretion werefound in those
with severe sodium retention (p < 0-005) (Fig. 2).
Urinary lossesofpotassium inexcessofintakewere seen only in patients with severe alkalosis. Mean
values for plasma potassium, calculated potassium intake, and arterial pHweresimilarinthetwogroups
and plasma potassium was unrelated to urinary potassium excretion (r = -0-21, NS).
Subsequent course Five of the 10 patients with severesodium retentiondied, three of these develop-ing renal failure before death. One of the five survivors regained her ability to excrete sodium normally whilestillindeepcoma, but the remainder recovered consciousness before this occurred.
All the patients with a relatively good sodium excretion survived, though one case developed evidence ofseveresodium retention before beginning toimprove. Thisdifference in mortality between the two groups is statistically significant (p = 0-01, Fisher's exact test), although they were otherwise similarinage, sex,aetiologyofliver failure,gradeof encephalopathy, andstandard liver functiontests.
Follow-up studies onfour cases during recovery showed that glomerular filtrationrate,renal plasma flow, and free waterclearance returned to normal withintwoweeks.
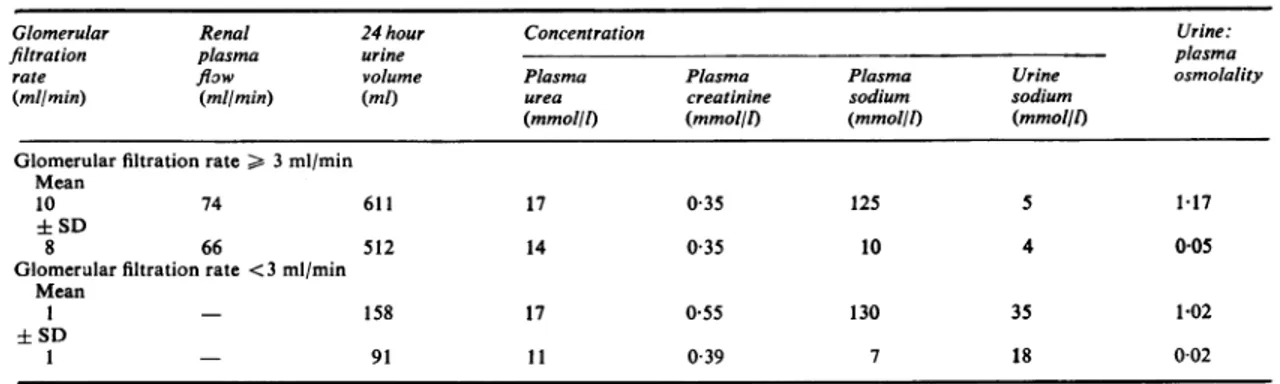
GROUP 2 (PATIENTS WITH GLOMERULAR FILTRATION RATE LESS THAN 25 ML/MIN) (Table 2)
In additiontothethree sodium retainerswhoserenal function subsequently deteriorated, there were 22 other patients in this group. Of these 25 only one survived.
Glomerularfiltrationratevaried from less than I to24ml/min. The 14 patients in whom thiswas >3
ml/min all had low urine sodium concentration values, the highest being 14 mmol/l witha meanof 5 mmol/l (±4, SD). These patients also hada hyper-osmolarurine, the lowest valueof theratiobetween the urine and plasma osmolality being
1P09
with a mean of1P17
(±005, SD). In contrast, when glomerularfiltrationrate was <3ml/min (13 cases, includingtwoinwhom itwaspreviously>3ml/min), values for urine sodium concentrations were relatively high(>16mmol/linall butone case, mean 35mmol/l, ± 18 SD) and the urine: plasma osmolality ratio low ( 1 09, mean 1-02 ± 0-02 SD). In the patients in whom glomerular filtration rate fell from >3 to < 3ml/min, the values for urine sodium concentration and urine:plasma osmolality changed accordingly.Renal histology from necropsy examination was available in eight of the cases whose glomerular filtrationratewas <3ml/min, andatleastoneof the following changes was present: tubular dilatation,
tubularnecrosis, interstitial oedema. In seven cases with aglomerular filtrationrateof>3ml/minrenal histology was normal, but in three others changes similar to thoseoccurring in the other group were
found. However, these latterthree patientsall had terminalhypotension andanuria.
Examination of the urine sediment for granular and cellular casts did not necessarily distinguish 503
Table 2 Renalfunction in patients with glomerularfiltration rate < 25 ml/min*
Glomerular Renal 24 hour Concentration Urine:
filtration plasma urine plasma
rate flow volume Plasma Plasma Plasma Urine osmolality
(ml/min) (mllmin) (ml) urea creatinine sodium sodium
(mmol/l) (mmol/l) (mmol/l) (mmol/l) Glomerular filtration rate > 3 ml/min
Mean
10 74 611 17 035 125 5 1-17
± SD
8 66 512 14 035 10 4 005
Glomerular filtration rate <3 ml/min Mean
I - 158 17 0 55 130 35 1-02
± SD
1 - 91 1 1 0-39 7 18 0-02
*Fulldetailsrelating to individual patients are available from the authors.
between these patients. Althoughcastswerealways
found in those with aglomerular filtration rate of
<3 ml/min, thesewere alsoseen in the urine from sevenoftheother 14patients.
Para-aminohippurate clearance was measured in
nine of the patients withaglomerular filtrationrate
of >3 ml/min and values ranged from 9 to 201 ml/min.
Discussion
Renalretention of sodium,animpairedresponsetoa waterload and minorreductions in renal perfusion have all been described in infectious hepatitis (Cachera and Darnis, 1951; Wolf et al., 1958; Dittrich, 1966). In the present study these changes
werealsofound in patients with hepatic necrosis due to paracetamol overdose and multipleexposures to
halothane. Thus it is likely that these changes are
secondary to hepatocellular disease rather than a
directnephrotoxic effect of theseagents,eventhough
paracetamol has been described as a nephrotoxin
(Matthew, 1972). As inourprevious study(Wilkinson et al., 1974a) the incidence of renal failure in this serieswassimilar in the differentaetiologicalgroups.
When assessing sodium and potassium excretion it is usual to base conclusions on the results of
balance studies carried outfora minimum of three
or four days. However, this is not possible in fulminant hepatic failure because of the unstable
natureof the syndrome. The limitations of the value oftheone day balances in the present studymust
therefore be borneinmindinthe interpretationof the
results. The separation of patients withaglomerular
filtrationrate greaterthan 40ml/min intotwogroups on the basis ofurinary sodium excretion is
some-whatartificial in thatacompleterangeofvalueswas
found. However, looking at the two ends of the
spectrum might help in understanding the patho-physiology of sodium and water retention in this
condition. Since glomerular filtration and renal plasmaflowweresimilar in those patients with and withoutsodiumretention, it isunlikelythatchanges
inthesetwofactorswereofmajorimportancein the pathogenesis of sodium retention. Free water is normally generated in the kidney as a result of selective sodium (or chloride) absorption from the ascending limb of the loop of Henle so that early distal tubular fluid is hypotonic-that is, contains 'freewater'.Thisis thereforedependentonadequate delivery of sodium to the ascendinglimb and this depends on both the filtered load and proximal tubularreabsorption of sodium.Althoughtherewas astatistical relationship between freewaterclearance andfiltered load ofsodiumanumberofpatientswith relatively high values for the latterwere unable to excrete free water, so again other factors must be involved. One explanation for both sodium and water retention is that themajor site of abnormal sodium reabsorption is the proximal tubule since this wouldlimitthe amount ofsodium delivered to the diluting segment for generation of free water.
Hyperaldosteronism,evenifpresent,wouldtherefore notbeof majorimportance intheabnormal sodium retention unlessithas anactionontheproximalin addition tothedistal tubule of the nephron. Infor-mationonthis latterpoint isconflicting (Hierholzer
and Stolte, 1969;Lynch etal., 1972). However, the low potassium excretion found in association with sodium retention is further evidence against hyper-aldosteronism. Why excessive proximal sodium reabsorptionshouldoccuristhereforeuncertain, but previous sodium depletion seems unlikely. Alter-native explanations for the impaired free water clearance, such as inappropriately high circulating levels of antidiuretic hormone cannot, however, be excluded.
These findings differ from those described in
cirrhosis, as retention of sodium in the latter condition is oftenaccompanied byawell-maintained
Abnormalities of sodium excretion and otherdisorders of renal function in fulminant hepaticfailure 505 capacity forfree waterclearance, indicating that in
suchpatients excessive distal sodiumreabsorption is important(Baldusetal., 1964).
Free water clearance was determined in 24 investigations performed and, not surprisingly, a markedly reduced value (less than 1 ml/min) was related to the occurrence ofhyponatraemia (plasma sodiumconcentration less than130mmol/l,P= 0-03, Fisher's exacttest). Thus hyponatraemia is likelyto belargely duetooverhydration.
Althoughurinary loss ofpotassium is saidtobe high in fulminant hepaticfailure (Trey and Davidson, 1970),wehavenotbeenabletoconfirmthis,exceptin patients with a marked alkalosis. Some patients appeared to be in positive potassium balance yet values for plasma potassium concentration were often reducedor atthe lower limitof normal. Other significant losses, such as gastric aspiration and diarrhoea,were notusually found.
Renal failure in fulminant hepatic failure and cirrhosis is often classifiedasbeing either 'functional' or 'acutetubularnecrosis'. Inthepresent studythe patients withaglomerular filtrationrateofbetween 3and25ml/minhadalow urine sodium concentra-tion andahyperosmolarurine, featuressuggestive of intact tubular function, though more specific tests for this (urinary acidification, excretion of amino-acids, and tubular proteins) were not carried out. However, since renal histology was normal in this group itis reasonabletorefertothe renalfailureas 'functional'. The reduced para-aminohippurate clearance in thesepatients suggests that the patho-physiology is of reduced renal perfusion,ashas been describedincirrhosis(Baldusetal., 1964;Epsteinet al., 1970). When the glomerular filtration rate was less than 3ml/min the urinewasvirtuallyisomolar and the urine sodium concentrationrelatively high, findings thatareusually considered tobeindicative ofacute tubular necrosis (Levinsky, 1966), and in these patients an abnormal renal histology was found. Granular or cellular casts in the urine sedi-mentcouldnotsatisfactorily distinguish between the types of renal failure and, indeed, casts may be found inanyjaundiced patientwith otherwisegood renal function (Eknoyan, 1974). The difference betweenthesetwotypesof renalimpairmentmaybe quantitative rather than qualitative in that tubular function appears to be maintained until renal per-fusion is so low that the glomerular filtration rate falls toless than 3 ml/min. Below that level tubular necrosis occurs. The progression of some patients from functional renal failure to acute tubular necrosis is additional evidencethat these two types
of renal failureare partofasinglespectrum. Inother studieswehave shown that there is aclosecorrelation between the occurrence of both functional renal failureand acutetubular necrosis withendotoxaemia (Wilkinsonetal., 1974b). Endotoxin, a potentrenal vasoconstrictor, is derived from gram negative organisms in the bowel, andpresumablyescapesinto the systemiccirculation because of impairedhepatic clearance.
We are particularly grateful totheDepartments of Chemical Pathology for theirhelpwith some ofthe determinations.
References
Baldus, W. P., Feichter, R. N., Summerskill,W. H. J., Hunt, J. C., and Wakim, K.G.(1964).Thekidney incirrhosis.
2Disorders of renal function.Annals of InternalMedicine,
60,366-377.
Cachera, R., and Darnis, F. (1951). Les formes inapparentes de l'oedeme dans l'infectieuse aigue b6nigne hepatite. Semainedes HopitauxdeParis, 27, 1843-1849.
Dittrich, P. (1966).Partialfunktionen der Niere bei Hepatitis epidemica und Verschlussikterus. Klinische Wochenschrift, 44,441-446.
Eknoyan, G. (1974). Renal disorders in hepatic failure. British MedicalJournal,2,670.
Epstein, M., Berk, D. P., Hollenberg, N. K., Adams,D.F., Chalmers, T. C., Abrams, H. L., and Merrill, J.P.(1970). Renal failure in the patient with cirrhosis. The role of
active vasoconstriction. American Journal of Medicine, 49, 175-185.
Hierholzer, K., and Stolte, H. (1969). The proximal and
distal tubular action of adrenal steroids on Na reabsorp-tion. Nephron, 6,188-204.
Levinsky, N. G. (1966). Management of emergencies.
5Acute renal failure. New EnglandJournalof Medicine, 274, 1016-1018.
Lynch, R. E., Schneider, E. G., Willis, L. R.,and Knox,F. G.
(1972). Absence of mineralocorticoid-dependant sodium reabsorption in dog proximal tubule. American Journalof Physiology, 223,40-45.
Matthew, H. (1972). Drug overdose. Medicine(London), 4, 273-286.
Smith,H. W.(1956). PrinciplesofRenalPhysiology.Oxford University Press: London.
Trey, C., and Davidson, C.S. (1970). The management of
fulminant hepatic failure. In Progress in Liver Disease, pp. 282-298. Edited by H.Popper andF.Schaffner.Grune
and Stratton: New York.
Varley, H. (1967). PracticalClinical Biochemistry. 4th edn, pp.178-182. Heinemann: London.
Wilkinson, S. P., Blendis, L. M., andWilliams, R.(1974a). Frequency and type of renal and electrolyte disordersin
fulminant hepatic failure. British MedicalJournal, 1, 186-189.
Wilkinson, S. P., Arroyo, V., Gazzard, B. G., Moodie, H.,
and Williams, R. (1974b). Relation of renal impairment
andhaemorrhagic diathesis toendotoxaemiainfulminant hepatic failure. Lancet, 1, 521-524.
Wolff, H. P., Koczorek, K. R., and Buchborn, E. (1958). Aldosteroneandantidiuretic hormone (adiuretin)in liver
doi: 10.1136/gut.17.7.501
1976 17: 501-505 Gut
S P Wilkinson, V A Arroyo, H Moodie, et al.
failure.
function in fulminant hepatic
and other disorders of renal
Abnormalities of sodium excretion
http://gut.bmj.com/content/17/7/501
Updated information and services can be found at:
These include:
References
http://gut.bmj.com/content/17/7/501#related-urls
Article cited in:
service Email alerting
online article.
article. Sign up in the box at the top right corner of the Receive free email alerts when new articles cite this
Notes
http://group.bmj.com/group/rights-licensing/permissions
To request permissions go to:
http://journals.bmj.com/cgi/reprintform
To order reprints go to:
http://group.bmj.com/subscribe/