311ModFTPW/EN00
Second Level Master in “Innovation in Cardiac Surgery: Advances in Minimally Invasive Therapeutics”
Academic Year
2018/2019
PROPENSITY-MATCHED COMPARISON
BETWEEN MINIMALLY INVASIVE AND
CONVENTIONAL STERNOTOMY IN AORTIC
VALVE REPLACEMENT: EXPERIENCE IN A
SPANISH TERTIARY HOSPITAL
Author
Corazón Mabel Calle Valda
Scientific Tutor
Dr. Marco Solinas
Organization Tutor
Prof. Claudio Passino
ABSTRACT
Traditionally, the conventional approach for aortic valve replacement was through a complete median sternotomy. However, the rapid development and improvement of new surgical techniques, has allowed the realization of new approaches such as minimally invasive surgery that has revolutionized many facets of surgical practice in cardiac surgery and pretend to be an alternative to surgery with results at least equivalent to conventional surgery.
In this sense, the main objective is oriented to the analysis and comparison of the short and medium term results of the aortic valve replacement regarding the surgical approach: conventional surgery and minimally invasive surgery.
For this purpose, a retrospective cohort study was made with prospectively collected data on 371 patients undergoing aortic valve replacement between 2014 and 2018 at the “Hospital
Universitario de la Princesa” in Madrid. Of the 371 patients, 296 belonged to the conventional
surgery (CAVR) group and 75 to the minimally invasive aortic surgery group (MIAVR). To provide equivalence among the comparison groups, a multinomial "propensity score matching" 1: 1 analysis was performed and two patient cohorts were identified and selected statistically.
Among highlights of the results in this study, we observed that surgical times reflected a longer trend in the minimally invasive group compared to conventional surgery, though the difference is not statistically significant. Two patients in the minimally invasive group required conversion to a full sternotomy due to poor exposure of the aortic annulus. As regards complications, the minimally invasive surgery group showed a decreased incidence of new onset postoperative atrial fibrillation. However, more pneumothorax and pleural effusion were observed.
Additionally, the total hospitalization time, the MIAVR group presented shorter stays. During follow-up, no differences in mortality and survival were observed in the two groups. As regards the learning curve of the MIAVR group, was necessary a minimum of 27-30 cases to achieve these competences.
In conclusion, we can say that the two approaches for aortic replacement offer excellent results depending on the characteristics of each patient. A correct selection of patients by the "Heart Team" is fundamental to offer each individual the best possible treatment based on the available scientific evidence and the experience of each center.
TABLE OF CONTENTS
... 1
LIST OF ABBREVIATIONS ... 7
INTRODUCTION ... 8
SIGNIFICANCE OF THE STUDY ... 9
CHAPTER 1: HYPOTHESIS ... 11
CHAPTER 2: OBJECTIVES ... 12
CHAPTER 3: METHODOLOGY ... 13
3.1
STUDY DESIGN ... 13
3.2
PATIENT SELECTION ... 13
3.2.1 INCLUSION CRITERIA ... 13
3.2.2 EXCLUSION CRITERIA ... 14
3.3
DATA COLLECTION ... 14
3.4
STATISTICAL ANALYSIS ... 14
CHAPTER 4: RESULTS ... 16
4.1
DEMOGRAPHICS AND OPERATIVE CHARACTERISTICS OF TWO
MATCHED COHORTS. ... 17
4.2
INTRAOPERATIVE DATA OF TWO MATCHED COHORTS ... 18
4.3
POSTOPERATIVE RESULTS AND COMPLICATIONS OF TWO
MATCHED COHORTS ... 19
4.4
SURVIVAL ANALYSIS ... 20
4.5
LEARNING CURVE FOR MINIMALLY INVASIVE AORTIC VALVE
REPLACEMENT. ... 21
CHAPTER 5: DISCUSION ... 24
CONCLUSIONS ... 27
LIST OF ABBREVIATIONS
AHA:American Heart Association
AVA: Aortic valve area
AVR: Aortic valve replacement
CAVR: Conventional aortic valve replacement COPD: Chronic obstructive pulmonary disease CPB: Cardiopulmonary bypass
CUSUM: Cumulative sum
ESC: European Society of Cardiology
EuroSCORE: European System for Cardiac Operative Risk Evaluation ICU: Intensive care unit
MACCE: Mayor Adverse Cardiac and Cerebrovascular Event MIAVR: Minimally invasive aortic valve replacement MICS: Minimally invasive cardiac surgery
NYHA: New York Heart Association LVEF: Left ventricular ejection fraction
SECTCV: Sociedad Española de Cirugía Torácica-Cardiovascular SICCS: Sistema Informático Cirugía Cardíaca Sorin
SPSS: Statistical Package for Social Sciences STS: Society of Thoracic Surgeons
8
INTRODUCTION
The cardiovascular pathology is certainly one of the main causes of morbidity and mortality in our country. Recent data confirm that cardiovascular diseases remain the primary cause of death (rate of 323.6 deaths per 100.000 inhabitants), followed by cerebrovascular diseases (269.4) and bronchial
and lung cancer (220.9) (1).
In parallel, health care and health protection have been increasing dramatically since the late nineteenth century. Improvements in social development such as education, better nutrition, improvement of living standards, greater equality and social cohesion and a great improvement in
lifestyles (2) have meant that life expectancy has progressively increased. As a consequence of these
improvements, life expectancies have tended to increase from 70.6 years of life expectancy at birth
in men and 76.0 in women in 1975 to 80.4 and 85.7, respectively in 2017 (3).
The high prevalence of cardiovascular diseases, together with the increase in life expectancy and therefore of population aging, means that we are faced with an increase in the pathology of the aortic valve, in particular severe aortic stenosis. This pathology increases its prevalence with age, being 3%
in the population older than or equal to 65 years and 7.4% in those over 85 years (4).
According to the recent record of interventions of the Spanish Society of Thoracic-Cardiovascular
Surgery (SECTCV) (5) during 2017, 32692 procedures were performed in Spain in 62 centers. The
average number of interventions per center was 592. In a pathology analysis, the highest volume corresponds to the procedures performed in isolated valvular pathology (n = 9682) followed by ischemic pathology (n = 5029). When analyzing the number of isolated valve procedures performed in 2017, we observed an increase with respect to 2016 of 281 procedures. Of these, 77% were on a single valve and 23% on several valves.
The most frequent isolated procedure continues to be aortic valve replacement, with 5153 procedures (53.2% of the total isolated valve surgery) and an average mortality of 3.05% in 2017, less than 50% of that estimated by EuroScore II.
The transcatheter aortic prosthesis implant (TAVI) also continues to increase every year. During 2017, 507 TAVI were implanted by cardiovascular surgery services and 2821 TAVI by the cardiology services. Despite this, for the moment, this increase in activity in the percutaneous treatment of aortic valve pathology has not meant a decrease in the implantation of surgical aortic prostheses in
pathology isolated from the aortic valve. Currently, the TAVI implant represents about 30% of the treatment on the isolated pathology of the aortic valve.
Logically, the decision for operative intervention in an elderly patient entails a series of specific
problems related to increased mortality and operative morbidity (6). However, since the introduction
of the transcatheter aortic implant, it has been possible in patients in whom no intervention was
previously performed (7).
SIGNIFICANCE OF THE STUDY
Traditionally, aortic valve replacement is performed through a complete median sternotomy, but we currently have other approaches, such as minimally invasive surgery that has revolutionized many facets of surgical practice in cardiac surgery and percutaneous therapies, which prevent sternotomy and extracorporeal circulation, and pretend to be an alternative to surgery.
Minimally invasive cardiac surgery (MICS) has undergone numerous changes in its technique in recent years. The growing interest in laparoscopic surgery, in general, prompted the search for minimally invasive techniques for use in cardiac surgery, such as Cosgrove that described the first
MICS in 1996 (8, 9). Subsequently, multiple retrospective studies have reported long series of patients
under MICS (10, 11), it has even been observed that high-risk patients by Euroscore may be candidates
for MICS in a feasible way for AVR.
The initial resistance in the adoption of minimally invasive surgery was based on the limited surgical exposure that could compromise safety by significantly increasing aortic cross-clamp and
extracorporeal circulation times and they may worsen surgical outcomes (11). In recent years, interest
in these techniques has grown in parallel with the development of technology through the adaptation of surgical instruments, alternative perfusion techniques, video-assisted systems and robots, allowing less invasive cardiac interventions without significantly affecting surgical times or altering the surgical outcomes.
Although the technical aspect of each approach differs slightly, its objectives are common: the development of an effective and safe aortic valve replacement with a reduction in surgical trauma that reduces postoperative pain, accelerates postoperative recovery and incorporation into daily life and therefore reduce hospital stays and resource consumption and also improve aesthetic results and
10
personal satisfaction. On the other hand, other studies show a lower incidence of surgical wound infection and a faster rehabilitation and recovery of respiratory function, since it preserves the chest
wall integrity (12, 13). This last one is very important, since respiratory function is one of the limiting
factors of the postoperative recovery of patients undergoing cardiac surgery, drastically influencing the consumption of health resources and therefore of costs.
For all the above, we believe that it would be important to analyse in a more extensive and deeper way the minimally invasive surgery, as a therapeutic option to conventional surgery in aortic valve replacement. Likewise, it is unquestionable that, with the comparison of both approaches, we will be able to know the results of the procedures that will be evaluated according to morbidity, mortality and post-surgical survival, which could help in the right decision when choosing the best treatment for each patient.
CHAPTER 1: HYPOTHESIS
Minimally invasive cardiac surgery by miniesternotomy could be a feasible therapeutic option for patients with aortic valve disease with similar results in terms of perioperative morbidity and mortality, safety and efficacy in the short and medium term when compared to conventional surgery.
12
CHAPTER 2: OBJECTIVES
General Objective
To analyze and compare the results in the short and medium term of the treatment of aortic valve pathology according to the technique used: conventional surgery by full sternotomy and minimally invasive surgery by miniesternotomy.
Specific Objectives
To describe the characteristics of the population of patients referred to surgical valve replacement using conventional surgery techniques and minimally invasive surgery.
To compare the surgical times: cardiopulmonary bypass and aortic cross-clamp times.
To compare the length of stay in ICU and the total hospital stay.
To identify and evaluate the main perioperative complications.
To analyze the learning curve of the minimally invasive approach at the beginning of the implementation of a program.
CHAPTER 3: METHODOLOGY
3.1 STUDY DESIGN
A retrospective observational cohort study was carried out of all patients with aortic valve disease (n=371) at the Hospital Universitario de La Princesa between January 2014 and December 2018. Patients were classified according to surgical approach: full sternotomy (CAVR=296) and mini sternotomy (MIAVR=75).
To perform the comparative analysis between these two patient populations, demographic, clinical and echocardiographic variables were analyzed preoperatively, intraoperatively and postoperatively during follow-up. Subsequently, a multinomial analysis “propensity score matching” 1: 1 was performed and using logistic regression criteria based on the preoperative characteristics of the patients, two cohorts of patients were identified and statistically selected.
The learning curve was evaluated through the cumulative sequential probability sum (CUSUM) method.
3.2 PATIENT SELECTION
The study population included all patients with aortic valve disease, undergoing conventional surgery and minimally invasive surgery between January 2014 and December 2018 at the Hospital
Universitario de La Princesa, Madrid. A total of 371 patients with aortic valve disease were
identified, 296 (79.8%) by full sternotomy (conventional approach) and 75 (20.2%) by mini sternotomy (minimally invasive approach).
3.2.1 INCLUSION CRITERIA
All patients admitted for elective aortic valve replacement surgery and patients for whom aortic valve replacement was indicated under current ESC and AHA guidelines (SVA surgical indication according to current ESC and AHA guidelines).
14
3.2.2 EXCLUSION CRITERIA Patients who require other concomitant procedures (coronary or valvular surgery, or surgery of the ascending aorta or the aortic arch).
Patients operated on urgently.
Patients with lack of preoperative documentation. Patients lost for follow-up.
3.3 DATA COLLECTION
Pre, intra and post-operative data was gathered retrospectively from the Hospital Universitario
de La Princesa SICCS database (Sistema Informático Cirugía Cardíaca Sorin) (Biomenco, Madrid,
Spain).
3.4 STATISTICAL ANALYSIS
First, the general data of the total population were analyzed in order to know the overall results in patients undergoing aortic valve replacement. Subsequently, the results were analyzed comparing the groups according to the type of approach used: conventional surgery and minimally invasive surgery by miniesternotomy.
The statistical program used was SPSS (Statistical Package for Social Sciences) version 23.0 (SPSS Inc, MN, US). In all tests, a level of statistical significance was accepted when the value of p was less than 0.05 (p <0.05).
We used means, standard deviations, medians for quantitative variables, and frequencies and percentages for categorical variables. The Student's t-test was used for the comparison of means and the Chi-square test for categorical comparisons. When the distribution of the variable did not follow a normal distribution, non-parametric tests were used (Mann-Whitney U, Wilcoxon test, Kruskal-Wallis test).
After patients were assigned to the two treatment groups, and after the application of the inclusion and exclusion criteria, a 1:1 propensity match was conducted to provide evidence of equivalence between the comparison groups.
The Kaplan-Meier method is used for survival analysis. The statistic used to detect statistically significant differences between the different groups was the Mantel-Cox Long-Rank.
To assess the learning curve, the cumulative sequential probability sum (CUSUM) (14, 15) was
performed, which gave us almost real-time monitoring of surgical performance. Surgical failure was defined as the occurrence of one or more events: perioperative death, conversion to intraoperative sternotomy, major complications: myocardial infarction, rhythm disorders: Ventricular tachycardia, atrial fibrillation or complete AV block, neurological complications: CVA, renal failure , severe pneumonia, reoperation due to bleeding, mechanical ventilation> 48 hours, surgical wound infection; and success was defined as none of the previous complications.
16
CHAPTER 4: RESULTS
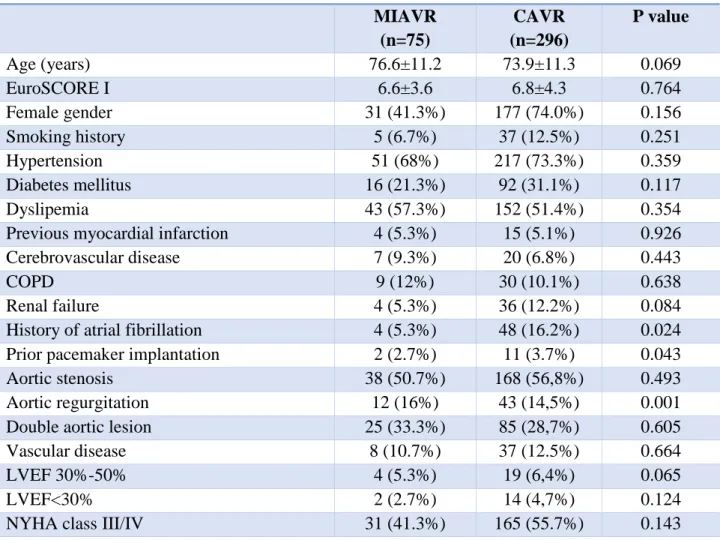
As can be seen in Table 1, when we make the comparison between the preoperative baseline clinical characteristics of the two types of approach, we can observe that being a retrospective study it contains some statistically significant differences between the groups, such as selection bias. Possibly, due to that the conventional surgery group has 296 cases and the minimally invasive surgery group with only 75 cases.
Table 1. Preoperative clinical characteristics of study patients
MIAVR (n=75) CAVR (n=296) P value Age (years) 76.6±11.2 73.9±11.3 0.069 EuroSCORE I 6.6±3.6 6.8±4.3 0.764 Female gender 31 (41.3%) 177 (74.0%) 0.156 Smoking history 5 (6.7%) 37 (12.5%) 0.251 Hypertension 51 (68%) 217 (73.3%) 0.359 Diabetes mellitus 16 (21.3%) 92 (31.1%) 0.117 Dyslipemia 43 (57.3%) 152 (51.4%) 0.354
Previous myocardial infarction 4 (5.3%) 15 (5.1%) 0.926
Cerebrovascular disease 7 (9.3%) 20 (6.8%) 0.443
COPD 9 (12%) 30 (10.1%) 0.638
Renal failure 4 (5.3%) 36 (12.2%) 0.084
History of atrial fibrillation 4 (5.3%) 48 (16.2%) 0.024
Prior pacemaker implantation 2 (2.7%) 11 (3.7%) 0.043
Aortic stenosis 38 (50.7%) 168 (56,8%) 0.493
Aortic regurgitation 12 (16%) 43 (14,5%) 0.001
Double aortic lesion 25 (33.3%) 85 (28,7%) 0.605
Vascular disease 8 (10.7%) 37 (12.5%) 0.664
LVEF 30%-50% 4 (5.3%) 19 (6,4%) 0.065
LVEF<30% 2 (2.7%) 14 (4,7%) 0.124
NYHA class III/IV 31 (41.3%) 165 (55.7%) 0.143
CAVR, conventional aortic valve replacement; MIAVR minimally invasive aortic valve replacement; EuroSCORE (European System for Cardiac Operative Risk Evaluation); COPD, chronic obstructive pulmonary disease; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
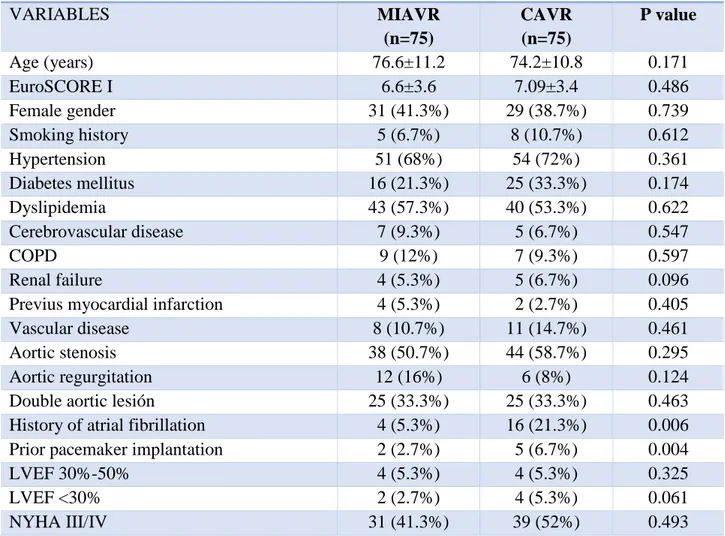
4.1 DEMOGRAPHICS AND OPERATIVE CHARACTERISTICS OF TWO MATCHED COHORTS.
In order to maintain equivalence between the two comparison groups, a propensity score matching analysis was performed selecting the main preoperative risk variables and baseline characteristics. The matching was performed 1: 1. The total cases were 150 (conventional group = 75; minimum invasive group = 75).
Table 2. Demographics and operative characteristics of two matched cohorts
VARIABLES MIAVR (n=75) CAVR (n=75) P value Age (years) 76.6±11.2 74.2±10.8 0.171 EuroSCORE I 6.6±3.6 7.09±3.4 0.486 Female gender 31 (41.3%) 29 (38.7%) 0.739 Smoking history 5 (6.7%) 8 (10.7%) 0.612 Hypertension 51 (68%) 54 (72%) 0.361 Diabetes mellitus 16 (21.3%) 25 (33.3%) 0.174 Dyslipidemia 43 (57.3%) 40 (53.3%) 0.622 Cerebrovascular disease 7 (9.3%) 5 (6.7%) 0.547 COPD 9 (12%) 7 (9.3%) 0.597 Renal failure 4 (5.3%) 5 (6.7%) 0.096
Previus myocardial infarction 4 (5.3%) 2 (2.7%) 0.405
Vascular disease 8 (10.7%) 11 (14.7%) 0.461
Aortic stenosis 38 (50.7%) 44 (58.7%) 0.295
Aortic regurgitation 12 (16%) 6 (8%) 0.124
Double aortic lesión 25 (33.3%) 25 (33.3%) 0.463
History of atrial fibrillation 4 (5.3%) 16 (21.3%) 0.006
Prior pacemaker implantation 2 (2.7%) 5 (6.7%) 0.004
LVEF 30%-50% 4 (5.3%) 4 (5.3%) 0.325
LVEF <30% 2 (2.7%) 4 (5.3%) 0.061
NYHA III/IV 31 (41.3%) 39 (52%) 0.493
CAVR, conventional aortic valve replacement; MIAVR minimally invasive aortic valve replacement; EuroSCORE (European System for Cardiac Operative Risk Evaluation); COPD, chronic obstructive pulmonary disease; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
18
When comparing the preoperative baseline characteristics of the two types of approaches, as Table 2 shows, no differences were found in the average age and the logistic EuroSCORE between the MIAVR and CAVR groups (76.6 ± 11.2 vs. 74.2 ± 10.8; p = 0.171).
Based on cardiovascular risk factors, high blood pressure, diabetes mellitus, dyslipidemia and smoking, no differences were observed in the two types of approach.
Severe aortic stenosis was the most common indication of SVA with more than 50% of cases in both groups (50.7 vs. 58.7%; p = 0.295). However, there is a tendency to a greater number of cases with severe aortic insufficiency intervened in the minimally invasive surgery group compared to conventional surgery, although the result did not become significant (16% vs. 8%; p = 0.124).
With reference to rhythm disorders, the highest proportion of patients with a history of atrial fibrillation (5.3% vs. 21.3; p = 0.006) and with a previous pacemaker (2.7% vs. 6.7%; p = 0.004) were operated by conventional surgery.
Distribution of percentage of NYHA class III-IV was 41.3% in MIAVR vs 52% in CAVR; p = 0.493.
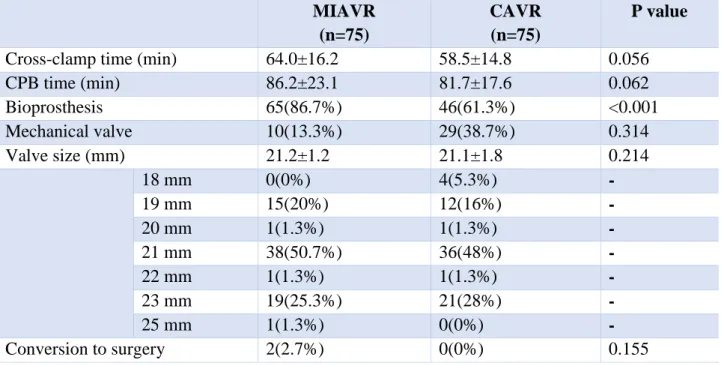
4.2 INTRAOPERATIVE DATA OF TWO MATCHED COHORTS
The intraoperative data are shown in Table 3, where we can see that the aortic cross-clamp (64.0 ± 16.2 vs 58.5 ± 14.8; p = 0.056) and extracorporeal circulation times (86.2 ± 23.1 vs 81.7 ± 17.6; p = 0.062) are slightly longer in the MIAVR group as compared with conventional surgery, though the difference is not statistically significant.
As regards the type of valve, our sample had a high preponderance of patients of advanced years, which meant that among the two groups more than sixty percent patients received a biological prosthetic valve (86.7% vs. 161.3%; p <0.001).
Two patients in the MIAVR group required conversion to full sternotomy due to poor exposure of the ring.
Table 3. Intraoperative Data MIAVR (n=75) CAVR (n=75) P value
Cross-clamp time (min) 64.0±16.2 58.5±14.8 0.056
CPB time (min) 86.2±23.1 81.7±17.6 0.062 Bioprosthesis 65(86.7%) 46(61.3%) <0.001 Mechanical valve 10(13.3%) 29(38.7%) 0.314 Valve size (mm) 21.2±1.2 21.1±1.8 0.214 18 mm 0(0%) 4(5.3%) - 19 mm 15(20%) 12(16%) - 20 mm 1(1.3%) 1(1.3%) - 21 mm 38(50.7%) 36(48%) - 22 mm 1(1.3%) 1(1.3%) - 23 mm 19(25.3%) 21(28%) - 25 mm 1(1.3%) 0(0%) - Conversion to surgery 2(2.7%) 0(0%) 0.155
CAVR, conventional aortic valve replacement; MIAVR, minimally invasive aortic valve replacement; CPB, cardiopulmonary bypass.
4.3 POSTOPERATIVE RESULTS AND COMPLICATIONS OF TWO MATCHED COHORTS
Early results and postoperative complications in each group are summarized in Table 4. Postoperative ventilation, drainage residue in the first 24 hours and stay in ICU were similar in both surgical groups. The total hospital stay for the MIAVR group was shorter compared with the CAVR group (9.7 ± 6.5 vs. 13.3 ± 8.8; p = 0.006).
There were no significant differences among the two groups as far as postoperative complications related to stroke to 30 days, MACCE events or re-operation due to bleeding.
The MIAVR group showed a decreased incidence of new onset atrial fibrillation (2.7% vs. 12%; p <0.001). However, the highest proportion of cases with pneumothorax and pleural effusion (8% vs. 1.3%; p = 0.032) were in the minimally invasive surgery group.
20
Table 4. Postoperative results and complications
MIAVR (n=75) CAVR (n=75) P value Ventilation time (h) 7.3±7.3 8.7±6.8 0.355 Postoperative bleeding (ml/24hr) 282±124.5 300.2±136.9 0.168
Total ICU stay(days) 2.4±2.6 3.1±4.2 0.272
Total hospital stay (days) 9.7±6.5 13.3±8.8 0.006
Mean gradient at discharge (mmHg) 16.1±9 14.1±5.2 0.327
Peak gradient at discharge (mmHg) 27.4±11.1 26.1±7.8 0.584
AVA 1.42±0.4 1.51±0.2 0.478
LV mass 169.4±38.9 155.4±50.2 0.296
Sternal Dehiscence 0(0%) 2(2.7%) 0.155
Pneumothorax/Pleural effusion 6(8%) 1(1.3%) 0.032
Reexploration for bleeding 0(0%) 1(1.3%) 0.365
Stroke to 30 days 1 (1.3%) 2 (2.7%) 0.064
MACCE events 2(2.7%) 7(9.3%) 0.061
New onset of atrial fibrillation 2(2.7%) 9(12%) <0.001
Pacemaker implantation 1(1.3%) 3(4%) 0.126
Thirty-day readmissions 1 (1.3%) 4(5.3%) 0.363
Thirty-day mortality 1(1.3%) 1(1.3%) 1.000
Overall mortality 8(10.7%) 15(20%) 0.124
CAVR, conventional aortic valve replacement; MIAVR minimally invasive aortic valve replacement; ICU, intensive care unit; AVA, Aortic valve area; LV, Left ventricular; MACCE, Major Adverse Cardiac and Cerebrovascular Events.
4.4 SURVIVAL ANALYSIS
The cumulative survival estimated by the Kaplan-Meier method with an average follow-up time of 46.7 months [95% CI 42-51.4] was 89.3% in MIAVR group and 80% in CAVR group (Long Rank x² = 1,583; p = 0.208 ) (Figure 1 and Table 5).
Table 5 .Cumulative survival of two matched cohorts Total Events Censurado Conventional surgery 75 15 60 (80.0%) Minimally invasive surgery 75 8 67 (89.3%)
Figure 1. Overall Survival (Kaplan- Meier) 46.7 months (95% 42.0-51.4)
4.5 LEARNING CURVE FOR MINIMALLY INVASIVE AORTIC VALVE REPLACEMENT.
Before analyzing the learning curve, we believe it is important to perform an analysis of moving averages with extracorporeal circulation and aortic cross-clamp times (Figure 2 and 3). As we can see, there is a decreasing trend in the times of both in the last cases in relation to the first, which were above the average, even some cases exceeded the upper confidence limit.
The CUSUM analysis was very important to represent the learning curve in minimally invasive surgery. As shown in Figure 4, we can clearly visualize three phases of the curve, phase 1 of initial learning (cases 1 to 27), the phase 2 of development or acquisition of skills (cases from 28 to 54) and phase 3 of greater mastery of the technique after the accumulated experience (cases from 55 to 75).
Chi2 Sig. Log-Rank (Mantel-Cox) 1.583 0.208
22
Figure 2. Moving average of cardiopulmonary bypass time in MIAVR.
Figure 3. Moving average of aortic cross-clamp time in MIAVR. 71 64 57 50 43 36 29 22 15 8 1 160 140 120 100 80 60 40 20 0 Muestra Pr om ed io mó vi l __ X=86,2 LCS=135,2 LCI=37,2
Al menos un parámetro histórico estimado se utiliza en los cálculos.
Gráfica de promedios móviles de Tiempo de CEC
71 64 57 50 43 36 29 22 15 8 1 120 100 80 60 40 20 Muestra Pr om ed io mó vi l __ X=64 LCS=98,4 LCI=29,6
Al menos un parámetro histórico estimado se utiliza en los cálculos.
24
CHAPTER 5: DISCUSION
Aortic valve disease is a frequent disorder that affects approximately 3% of the general adult population. Aortic valve replacement is the standard treatment for symptomatic patients and has
proven to be safe, effective and associated with low morbidity and mortality (16, 17).
During the last decades, with the increase in life expectancy and therefore the population aging, the rapid development and improvement of new surgical techniques has allowed the performance of minimally invasive approaches in complex valve surgery with results at least equivalent to conventional surgery.
Minimally invasive aortic valve surgery is defined as an aortic valve replacement procedure that involves a small incision in the chest wall instead of conventional complete sternotomy. The objective of this type of surgery is to reduce the invasion of the surgical procedure, while maintaining
the same efficacy, quality and safety of a conventional approach (18-20). The most common techniques
are miniesternotomy and right anterior minitoracotomy.
Compared to conventional surgery, minimal access surgery is associated with low
perioperative morbidity, mortality and a low conversion rate to complete sternotomy (21). Long-term
survival seems to be at least comparable to that reported for conventional complete sternotomy. In spite of the mentioned advantages, the surgery of minimum access is limited by times of aortic cross-clamp and extracorporeal circulation longer, which have presented some problems in fragile and high risk patients. However, with the introduction of valves without suturing and rapid
deployment, surgical times have been drastically reduced by 35-40% (14, 22).
Once we have explained the context in which we are currently in relation to aortic valve surgery, we can say that with the present work we want to analyze the results in our center of a population of subsidiary patients of aortic valve replacement belonging to the real world. This population were adjusted by propensity score and divided into two cohorts of 75 cases depending on the type of approach used: conventional surgery or minimally invasive surgery.
Regarding the preoperative clinical and demographic characteristics, in our study we did not observe significant differences between the two groups. With the exception that the highest proportion of patients with a history of atrial fibrillation and previous pacemakers who were operated
on in the group of the conventional surgery results similar to number of cases of the Neely et al. (23).
to initiate a minimally invasive program, as the main surgeon would choose patients with the best conditions before surgery.
With regard to intraoperative variables, contrary to expectations, despite presenting longer aortic cross-clamp and cardiopulmonary bypass with a minimally invasive approach, these differences failed to reach statistical significance. These results contrast with the meta-analysis of
Phan et al. (24) where longer times are observed in minimally invasive surgery by miniesternotomy
than with the conventional approach. Despite a recent study by The Brigham and Women’s Hospital
(23) where a propensity score analysis of 552 paired cases was performed, it presented similar results
to ours, without finding significant differences in surgical times.
Numerous retrospective studies (25-27) and meta-analysis (28, 29) coincide in the benefits of
minimally invasive surgery, in terms of improvement of lung function, reduction of postoperative bleeding, postoperative atrial fibrillation, intubation time, stay in intensive care unit, hospital stay and even decrease in early and late mortality. In our study probably due to a small number of recruited patients, we failed to demonstrate all the benefits, and contrary to expectations, we found a higher incidence of pneumothorax and pleural effusion (8%) compared to conventional surgery. However, we were able to observe the decrease in the incidence of new onset atrial fibrillation during the postoperative period (2.7%), although the aetiology of atrial fibrillation remains complex and multifactorial, this reduction has already been seen in other minimally invasive studies, due to less
manipulation of the structures (30).
The miniesternotomy has a shortened learning curve, due to the familiarity of the exposure, which at the same time facilitates reconversion in case of complication. In our series, the conversion rate was 2.7%, which represented two cases, due to poor visualization of the ring (all of them within the first 40 cases), this result being similar to previous studies where the rate of conversion to full sternotomy is around 3%.
In our experience, surgical mortality at 30 days was lower than that predicted by the logistic EuroSCORE I in all groups, although it is known that the EuroSCORE overestimates is surgical risk, especially in high-risk patients. With regard to late mortality, no differences were found between the three groups in our centre.
In representative retrospective studies, the results regarding mortality begin to show certain
26
of which 176 were operated by a minimally invasive approach and Paredes et al (32) with a sample of
615 patients, 83 by a minimally invasive approach; found a lower mortality in these groups, 3% vs 9% (p 0.008) and 0% vs 4.8% (p <0.05) respectively.
The rapid evolution of minimally invasive cardiac surgery has led surgeons to the need to gain experience in this new field, while maintaining high quality results compared to conventional surgery. In our study, with the beginning of the surgeon's experience a careful selection of patients was made. Later, when the surgeon felt more familiar with this new technique, he also began to consider the sickest patients suitable for performing the new techniques. It is interesting to note that with the gain of experience in the learning curve, as observed in the cumulative sum analysis, a minimum of approximately 30 cases were necessary to achieve the necessary skills to carry out this technique.
CONCLUSIONS
1. MIAVR by ministernotomy is a procedure with easy reconversion and is not associated with prolonged aortic cross-clamp or cardiopulmonary bypass times compared with a full sternotomy.
2. Patients undergoing the MIAVR approach had better outcomes in terms of mortality and morbidity, such as a lower incidence of new onset atrial fibrillation during the postoperative period and a shorter hospital stay compared to conventional surgery.
3. In our centre, the incidence of respiratory complications such as pneumothorax and pleural effusion are higher compared to conventional surgery.
4. A minimum of 27-30 cases are necessary to achieve the necessary skills to carry out this approach.
5. The collaboration of the teamwork is fundamental: cardiac surgeons, anesthetists, perfusionists and nurses, both at the beginning and during the implementation of a minimally invasive surgery program.
28
BIBLIOGRAPHICAL REFERENCES
1. National Institute of Statistics of Spain. Deaths according to cause of death. 2017.
2. Wilkinson RG, Marmot M. Social determinants of Health: The solid facts. 2nd Edition. WHO
Regional Office for Europe: Denmark 2003.
3. National Institute of Statistics of Spain. Deaths according to cause of death. 2017.
4. Ferreira-Gonzalez I, Pinar-Sopena J, Ribera A, Marsal JR, Cascant P, Gonzalez-Alujas T, et
al. Prevalence of calcific aortic valve disease in the elderly and associated risk factors: a population-based study in a Mediterranean area. Eur J Prev Cardiol. 2013;20(6):1022-30.
5. López Menéndez J, Cuerpo Caballero G, Centella Hernández T, Polo López L, Silva
Guisasola J, Gascón García-Verdugo P, et al. Cirugía cardiovascular en España en el año 2017. Registro de intervenciones de la Sociedad Española de Cirugía Torácica-Cardiovascular. Cir Cardiov. 2018. DOI: 10.1016/j.circv.2018.10.003
6. Azpitarte J. Valvulopatías en el anciano: ¿cuándo operar? Rev Esp Cardiol. 1998;51(1):3-9.
7. Morís C, Avanzas P. TAVI: una revolución en cardiología. Rev Esp Cardiol.
2015;15(Supl.C):1-2.
8. Gundry Md SR, Shattuck Pa OH, Razzouk Md AJ, del Rio Md MJ, Sardari Md FF, Bailey
Md LL. Facile Minimally Invasive Cardiac Surgery via Ministernotomy. Ann Thorac Surg. 1998;65(4):1100-4.
9. Cosgrove DM, 3rd, Sabik JF. Minimally invasive approach for aortic valve operations. Ann
Thorac Surg. 1996;62(2):596-7.
10. Attia RQ, Hickey GL, Grant SW, Bridgewater B, Roxburgh JC, Kumar P, et al. Minimally
Invasive Versus Conventional Aortic Valve Replacement: A Propensity-Matched Study From the UK National Data. Innovations. 2016;11(1):15-23; discussion.
11. Johnston DR, Roselli EE. Minimally invasive aortic valve surgery: Cleveland Clinic
experience. Ann Cardiothorac Surg. 2015;4(2):140-7.
12. Moscarelli M, Emmanuel S, Athanasiou T, Speziale G, Fattouch K, Casula R. The role of
minimal access valve surgery in the elderly. A meta-analysis of observational studies. International journal of surgery (London, England). 2016;33 Pt A:164-71.
13. Shehada SE, Elhmidi Y, Mourad F, Wendt D, El Gabry M, Benedik J, et al. Minimal access
versus conventional aortic valve replacement: a meta-analysis of propensity-matched studies. Interactive cardiovascular and thoracic surgery. 2017;25(4):624-32.
14. Murzi M, Cerillo AG, Gilmanov D, Concistre G, Farneti P, Glauber M, et al. Exploring the
learning curve for minimally invasive sutureless aortic valve replacement. J Thorac Cardiovasc Surg. 2016;152(6):1537-46.e1.
15. Yap CH, Colson ME, Watters DA. Cumulative sum techniques for surgeons: a brief review. ANZ J Surg. 2007;77(7):583-6.
16. Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Barwolf C, Levang OW, et al. A
prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J. 2003;24(13):1231-43.
17. Lucas G, Tribouilloy C. Epidemiology and etiology of acquired heart valve diseases in adults.
Rev Prat. 2000;50(15):1642-5.
18. Farhat F, Lu Z, Lefevre M, Montagna P, Mikaeloff P, Jegaden O. Prospective Comparison
Between Total Sternotomy and Ministernotomy for Aortic Valve Replacement. J Card Surg. 2003;18(5):396-401.
19. Glauber M, Ferrarini M, Miceli A. Minimally invasive aortic valve surgery: state of the art
and future directions. Ann Cardiothorac Surg. 2015;4(1):26-32.
20. Rojas SV, Haverich A. Minimally invasive cardiac surgery: a safe alternative for aortic valve
replacement? Rev Esp Cardiol (Engl Ed). 2013;66(9):685-6.
21. Moustafa MA, Abdelsamad AA, Zakaria G, Omarah MM. Minimal vs median sternotomy for
aortic valve replacement. Asian Cardiovasc Thorac Ann. 2007;15(6):472-5.
22. Eichstaedt HC, Easo J, Harle T, Dapunt OE. Early single-center experience in sutureless aortic
valve implantation in 120 patients. J Thorac Cardiovasc Surg.2014;147(1):370-5.
23. Neely RC, Boskovski MT, Gosev I, Kaneko T, McGurk S, Leacche M, et al. Minimally
invasive aortic valve replacement versus aortic valve replacement through full sternotomy: the Brigham and Women's Hospital experience. Ann Cardiothorac Surg. 2015;4(1):38-48.
24. Phan K, Xie A, Di Eusanio M, Yan TD. A meta-analysis of minimally invasive versus
conventional sternotomy for aortic valve replacement. Ann Thorac Surg. 2014;98(4):1499-511.
25. Castrovinci S, Emmanuel S, Moscarelli M, Murana G, Bertolino EC, et al. Minimally invasive
aortic valve surgery. J. Geriatr Cardiol. 2016;13(6):499-503.
26. Kempfert J, Mohr FW, Walther T. Minimally invasive aortic valve surgery: where now and
where to next? Expert Rev Cardiovasc Ther. 2009;7(5):451-3.
27. Lio A, Miceli A, Ferrarini M, Glauber M. Minimally invasive approach for aortic and mitral
valve surgery. Eur J Cardiothorac Surg. 2016;50(6):1204-5.
28. Khoshbin E, Prayaga S, Kinsella J, Sutherland FW. Mini-sternotomy for aortic valve
replacement reduces the length of stay in the cardiac intensive care unit: meta-analysis of randomised controlled trials. BMJ open. 2011;1(2):e000266.
29. Glauber M, Moten SC, Quaini E, Solinas M, Folliguet TA, Meuris B, et al. International
Expert Consensus on Sutureless and Rapid Deployment Valves in Aortic Valve Replacement Using Minimally Invasive Approaches. Innovations (Phila). 2016;11(3):165-73.
30
30. Glauber M, Miceli A, Gilmanov D, Ferrarini M, Bevilacqua S, Farneti PA, et al. Right anterior
minithoracotomy versus conventional aortic valve replacement: a propensity score matched study. J Thorac Cardiovasc Surg. 2013;145(5):1222-6.
31. Doll N, Borger MA, Hain J, et al. Minimal access aortic valve replacement: effects on
morbidity and resource utilization. Ann Thorac Surg 2002;74:1318–22.
32. Paredes FA, Canovas SJ, Gil O, Garcia-Fuster R, Hornero F, Vazquez A, et al. Minimally
invasive aortic valve surgery. A safe and useful technique beyond the cosmetic benefits. Rev Esp Cardiol (Engl Ed). 2013;66(9):695-9.