Available
online
at
www.sciencedirect.com
ScienceDirect
j o ur na l h o me pa g e : h t t p : / / w w w . e l s e v i e r . c o m / l o c a t e / r p o r
Original
research
article
SBRT
and
extreme
hypofractionation:
A
new
era
in
prostate
cancer
treatments?
Filippo
Alongi
a,∗,
Alba
Fiorentino
a,
Berardino
De
Bari
baRadiationOncologyDepartment,SacroCuoreHospital,Negrar-Verona,Italy
bRadiationOncologyDepartment,CentreHospitalierUniversitaireVaudois(CHUV),Lausanna,Switzerland
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received25June2014 Receivedinrevisedform 30July2014
Accepted30September2014 Availableonline23October2014
Keywords: Radiotherapy Hypofractionation Prostatecancer Radiobiology
a
b
s
t
r
a
c
t
Aim: Radiationtherapy (RT) is a standard therapeutic optionfor prostate cancer (PC). Inthelastdecades,severalinnovativetechnologyapplicationshavebeenintroduced. 3-DimensionalconformalRT,volumetric/rotationalintensitymodulatedRTassociatedornot withimage-guidedRT,arebecominglargelydiffusedinthetreatmentofPC.
Background:ConsideringthatPCcouldhavealow␣/ratio,similartolate-reactingnormal tissues,itcouldalsobehighlyresponsivetofractionsize.Thus,thereductionofthenumber offractionsandtheincreaseofthedose/fractionseemtobereasonablechoicesinthe treat-mentofthiscancer.Thisreviewreportedthetechnologyevolution,theradiobiologicaland theclinicaldataabouttheroleofextremehypofractionatedRTinthetreatmentapproach ofPCpatients.
Materialsandmethods: Medline searchandanalysisofpublishedstudiescontainingkey words:prostatecancer,radiotherapy,stereotacticradiotherapy.
Results:Recenttechnologicaldevelopments,combinedwithanimprovedknowledgeofthe radiobiologicalmodelsinfavorofahighsensitivityofPCtolargerfractionsizesareopening anewscenarioinitstreatment,reportingfavorableefficacyandacceptabletoxicity,despite shortfollow-up.
Conclusion:Thus,thankstotechnologicalimprovementandtherecentradiobiologicaldata, “extremehypofractionatedRT”hasbeenstronglyintroducedinthelastyearsasapotential solidtreatmentoptionforPC.
©2014GreaterPolandCancerCentre.PublishedbyElsevierSp.zo.o.Allrightsreserved.
∗ Correspondingauthorat:RadiationOncologyDepartment,SacroCuoreHospital,ViaDonSempreboni5,37139Negrar-Verona,Italy.
Tel.:+390456014800.
E-mailaddress:fi[email protected](F.Alongi).
http://dx.doi.org/10.1016/j.rpor.2014.09.005
1.
Background
According toall international guidelines,radiation therapy (RT) is a standard therapeutic option for prostate cancer (PC).1–3
In the last two decades, several innovative technology applicationshavebeenroutinelyintroducedinexternalbeam RT (EBRT). At the turn ofthe century, 3-dimensional con-formalRT(3DCRT)became availableinalmost allradiation oncologydepartments,butthereafter,intensitymodulatedRT (IMRT)gained large diffusionand it isnow suggestedas a goldstandardinthetreatmentofPC.1,4Roboticor
volumet-ric/rotationalIMRTdeliverytechniques,associatedornotwith image-guidedRT(IGRT),arebecominglargelydiffusedinthe treatmentofPC.4–9Thus,theevidenceoftheclinicalimpactof
thesetechnologyadvancementspushclinicianstoimplement theseprecisetechniquesindailyclinicalpractice,andthe ben-efitsofthecurrenttechnologyrevolutionarepromising.10,11
Concomitantly, feedback from radiobiology estimations seemstobeevenmorerobustandalotofthesedataarein favorofareduceddurationofradicalRTtreatmentwithout adetrimentalimpactonclinicaloutcomes,bothintermsof efficacyandsafety.12–14
Finally, available technological improvements and the quite well established radiobiology data support extreme hypofractionationforPC,whichhasbeenrapidlyintroducedin thelastfewyearsandwhichisnowconsideredasapotential treatmentoptionforPCpatientscandidatetoEBRT.1
2.
Modern
stereotactic
body
Rt:
the
technology
revolution
In the last 30 years, several crucial steps have built the basesoftheimprovementsinRTdelivery.Afterthe introduc-tionofcomputertomography(CT)inradiationdepartments, therehasbeenadramaticgrowthintheimplementationof 3DCRT inclinical practice. IMRT was born as anevolution oftheconformaltechniquesandisabletoobtaindeep gra-dientand rapidfall-off ofdoses,for example betweenthe prostateandrectalwall,orclosetotheintestinalbowelwhen thepelvicnodesareincludedinthetreatmentplan,witha potentialimpactindecreasingbothacuteandlatetoxicities inPC treatments.10 Thus, IMRT is currentlyrecommended
over 3DCRT for the treatment oflocalized PC with a radi-calintent,inparticularwhenadoseescalationisconsidered suitable.15,16
Zaorsky et al. recently described as a ‘technologically advancedRT’, each RT modality allowinga morefavorable benefit/riskratiothanstandardRTapproaches.The technol-ogy gain derives from the use of upgraded IGRT, IMRT or integrationofboth.4,17
TheprincipalendpointofstereotacticbodyRT(SBRT)isto minimizethedosetothesurroundingcriticalnormal struc-tureswhiledeliveringhighdose/fractiontothetargetvolume. Upuntilafewyearsago,SBRTwasusuallyadoptedbyusing spatialcoordinatestodefinethepositionofthetargettobe irradiatedwithablativedoses.
Nowadays,thetermofSBRTisrapidlychangingtowarda conceptdescribinga“philosophy”fortreatingcancernot nec-essarilywithspatialcoordinates,butessentiallyprescribing highprecisedosesinoneorfewfractions.ModernSBRTadopts static, dynamic or volumetric IMRT techniques to provide sharperdosefall-offsandbetterdoseconformity.
In this context of high precision, extreme accuracy is essential.In particular,a specialattention shouldbegiven totheproblemoforganmotion,typicaloftheirradiationof extra-cranialorgans.Severaltechniqueshavebeenadopted: intraprostaticcoilsvisiblewithportalimaging(stereoscopic kVCT,megavoltageportalimages),CTscansimagesobtained immediatelybeforethetreatmentdelivery(kVcone-beamCT, megavoltagecone-beam CT),CTimageswithhelical acqui-sition (helical tomotherapy), ultrasound (B mode adapting targeting),andelectromagneticonlineverificationwith micro-probesplacedinthepatient.Pre-treatment3D-CTscansare probablybettersystems,butalso2D-systemadoptinginvasive fiducialmarkersisagoodalternative.
Finally, all these systems allow the verification of the positionofthetumor(orofthe targetvolume)beforeeach treatment session delivery, and substantially they reduce patientsetuperrorandallowareductionofthemarginaround thetarget.ThedeliveryofSBRTbadlyneedstheseverification tools,becausetheyallowareductionoftheuncertaintyof tar-getposition.18Allthesetechnologicalneedsseemdifficultto
beacceptedfromacost-effectivenesspointofview. Neverthe-less,manystudieshaveconcludedthatSBRTiscosteffective, asitallowsabetterorgansparinganddoseescalationonthe targetvolume,andtheyarealsocostsaving.19–21
AlthoughSBRTinPCcouldnotbeconsideredyetastandard option,duetothesmallnumberofpatientstreatedworldwide and therelatively shortfollow-up ofmostofthepublished experiences,itspreliminaryresultsarepromisingandSBRT adoption is rapidly increasing in the radiation oncology departments.1,18,22
Moreover,technologicalinnovationsshouldnotreplacethe clinical aspects ofPC, and indications forSBRT should be reservedtothosepatientswhowouldreallybenefitfromthis treatment.PatientspresentingT3tumorsand/orwithahigh riskofnodaldiffusionarenotthebestcandidatesforhighly focalized treatmentsand NCCN guidelinesdo notconsider SBRTamongstthetreatmentoptionsforthesepatients.1SBRT
inthesehigh riskpatientscould beconsideredasboostin someparticularcasesafterthefirstcourseofstandard exter-nalbeamirradiation(asitisfrequentlydonewithhighdose ratebrachytherapyinhighriskPCpatients)andalwaysinthe contextofcontrolled,prospectiveclinicaltrials(asinthetrial NCT01839994,availableonlineatwww.clinicaltrials.gov)..
3.
A
radiobiology
based
approach
The␣/ ratio isthe radiobiologicparameterto explainthe behavioroftissuesandcancerwithrespecttoradiation sched-ules. Inradiobiology,the␣/ratio isdefinedasthedoseat whichkillingofcellsbylinear(␣)andquadratic() compo-nentsisequal.Recentinvestigationsonbiochemicalcontrol inPCsuggestedan␣/valuebetween1and3GyforPC,which
issomewhatlowerthan thevaluetypicallyascribedto sur-roundingorgans,suchasbladderandrectum.23–27
ConsideringthatPCwouldhavealow␣/ratio,similarto late-reactingnormaltissues,itcouldbehighlyresponsiveto fractionsize.Thus,thereductionofthenumberoffractions andtheincreaseofthedose/fractionseemtobereasonable choicesinthetreatmentofthiscancer.
Hypofractionation would offer a unique opportunity to optimizethetherapeuticratiotakingadvantageofthe poten-tial heightened sensitivity of PC to higher dose/fraction (comparedtosurroundingorgansatrisk).Moreover,itmeans thatthetotallengthoftheradiotherapycourseisshortened, becoming less distressingand morerapidforthe patients, withanobviousimpactinimprovingthequalityoflifeand healthcosts.
Todate,several controlledrandomized trialscomparing standardRTscheduleswithmoderatehypofractionationfor PCcancerhavebeenpublished.28–33Despitesomedifferences
inthetreatmentschedulesadoptedintheexperimentalarms, inall these reportshypofractionated regimesappearto be associatedwithoptimal tolerabilityprofiles,comparable to thoseobservedforstandardcourses.Theseresultsseemto confirm the radiobiological assumption regarding the low ␣/ value of PC and the clinical and radiobiological back-ground,supporting thefurther reductionofthe number of fractionsandoveralltreatmenttime,theso-called“extreme hypofractionation”.Thisapproachcouldpotentiallydriveup thebiologicaleffectivedosefortumorcontrol;decreasethe equivalentdoseforlatetissueresponseanditisperformed in4–5 fractions, withvery large dose per fraction (usually 7–9Gy)inthecontextofvariousstereotacticbodytechniques. Moreover, SBRT add a novel radiobiological mechanism of radiation-induceddamage.Emergingdatasuggestthathigher dosesperfraction(ablativedoses)could addtodirect cyto-toxicitya microvascular damagewhich could substantially increasetumorcellkilling.34Finally,targetingthetumor
vas-culatureforobliteration withultra-high-dose radiation has beenassumedtobebeneficialfortumorcontrol.35,36
Finally,thepossibilitytodeliverhigherdoses/fraction pre-ciselydeliveredonthetargetcanofferasafeopportunityto increasethetherapeuticratioofPCradiotherapy.
4.
Published
data
AsafedeliveryofextremehypofractionatedRTregimes,other thanthefavorabletherapeuticratioofferedbythelowprostate cancer␣/ ratio, requires the use of highlyfocused irradi-ation techniques,delivering fulldoses tothe prostate only volumewitharapidfallofftominimizethedosetothe sur-rounding critical normal structures as well as the use of radiationtechniquesthatallowanoptimaltreatment accu-racybydailypatientrepositioningandcorrectionforinter-and intra-fractionorganmovements.37,38
MostoftheexperiencesreportingdataaboutprostateSBRT havebeenperformedwithCyberknife.39–51
OneoftheearliestreportsonCyberKnife®SBRTwas
con-ductedon44PCpatientstreatedwithatotaldoseof32–36Gy in4fractions.39Afteramedianfollow-upof13months,
over-all toxicity was mild and the 3-yearactuarial biochemical
freedomfromfailure(BFF)ratewasonly78%,butthislowrate wasexplainedbythelargeproportionofintermediate-and high-riskpatientsenrolledinthestudy.
Friedlandetal.40reportedtheresultson112patientswith
early stagePC treatedwith 35–36Gy in5 consecutive frac-tions.Afteramedianfollow-upof24months,themeanPSA valuewas0.78ng/ml.Twopatientsdevelopedbiopsy-proven local recurrenceand one patientdeveloped distant metas-tases.Authorsreportonlyonecaseofgrade3rectaltoxicity. Moreover,82%ofpatientsabletoachieveerectionspriorto therapymaintainedtheirpotency.34
Bolziccoet al.reportedpreliminarydataon45 low-and intermediate-risk PC patients and, more recently, updated theirdataon100patientstreatedwith35Gy(7Gy/fraction) deliveredwithCyberknife®.41,42 Noacute Grade3orhigher
acute toxicities were reported. Late Grade 3 genitourinary (GU)toxicitiesoccurredin1%ofthepatientsandnolate G3-4gastrointestinal(GI)toxicitieswereobserved.Noevidence of biochemical or clinical recurrence was shown in96/100 patients.42
A larger study,conducted byKatz et al.,43 involved 304
patients: the first 50 patients were treated with 35Gy (5 fractions)andtheremaining254patientsweretreatedwith 36.25Gy(5fractions).Resultsat6yearsshowedexcellent bio-chemicalcontrolratesandalowtoxicityprofile.44LateGrade
3GUtoxicitiesoccurredin2%ofpatientswhoweretreated with36.25Gy.Bowelandurinaryqualityoflife(QOL)scores camebacktobaselinevaluesafterafewmonthsfromSBRT and75%ofthepatientswhowerepotentbeforethetreatment remainedsexuallypotent.Actuarial5-yearBFFwas97%for low-risk,90.7%forintermediate-risk,and74.1%forhigh-risk patients,respectively.44
Kingetal.45enrolled,inaphaseIItrial,69patientswithlow
riskPCtoreceive36.25GyinfivefractionswithSBRTalone. TheauthorsreportedexcellentPSAresponses,alowtoxicity profileandQOLoutcomescomparabletootherradiotherapy approaches. Another analysison 211patients reported the sameresultsofSBRTCyberknife(35–36.25Gyin5fractions) showingoutcomescomparabletoconventionallyfractionated RTorbrachytherapy.46
Freemanetal.47reportedtheresultson41patients
receiv-ing SBRT with CyberKnife® (35–36.25Gy in 5fractions) for
clinicallylocalized,low-riskPC.Afteramedianfollow-upof 5 years,the BFFwas 93%, no late grade≥3 rectal toxicity occurred,andonlyonepatientexperiencedlategrade3GU toxicity.
Recently, a SBRT dose escalation study on 70 patients (37.5Gyvs.35–36.25Gyin5fractions)wasconductedbyOliai etal.48withfavorableefficacyandacceptabletoxicity:grade
3GUtoxicitiesincluded4%acuteand3%late(forhighdose group).
ApooledanalysisonSBRTusingtheCyberKnife(median doseof36.25Gyin4–5fractions)hasbeenpublishedbyKing et al.: the authors report the outcomes of a total of1100 patientswithclinicallylocalizedPCenrolledindifferent mul-ticentric prospective phase II clinical trials (8 institutions, treatmentperiod:2003–2011).Withamedianfollow-upof36 months, 49 patients experienced a PSAfailure (4.5%), 9of whichhavebeenlatelyclassifiedasbenignPSAbounces.The 5-yearBFFratewas93%forallpatients,butfor135patients
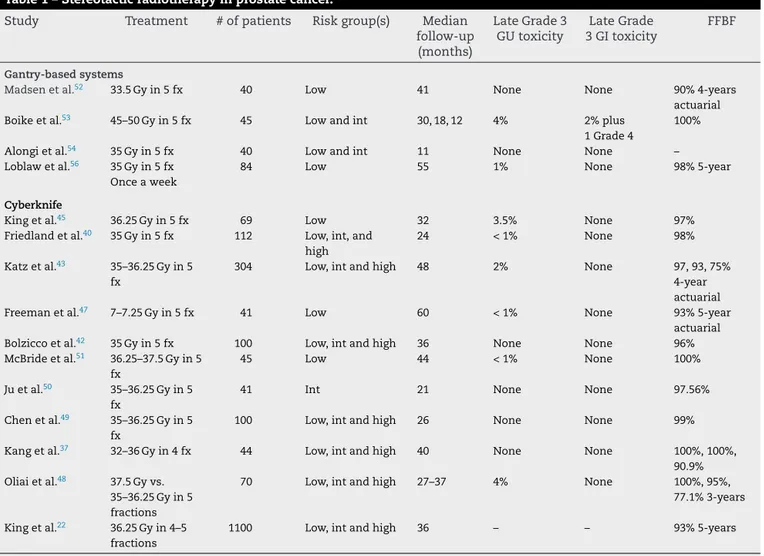
Table1–Stereotacticradiotherapyinprostatecancer.
Study Treatment #ofpatients Riskgroup(s) Median
follow-up (months) LateGrade3 GUtoxicity LateGrade 3GItoxicity FFBF Gantry-basedsystems
Madsenetal.52 33.5Gyin5fx 40 Low 41 None None 90%4-years
actuarial
Boikeetal.53 45–50Gyin5fx 45 Lowandint 30,18,12 4% 2%plus
1Grade4
100%
Alongietal.54 35Gyin5fx 40 Lowandint 11 None None –
Loblawetal.56 35Gyin5fx
Onceaweek
84 Low 55 1% None 98%5-year
Cyberknife
Kingetal.45 36.25Gyin5fx 69 Low 32 3.5% None 97%
Friedlandetal.40 35Gyin5fx 112 Low,int,and
high
24 <1% None 98%
Katzetal.43 35–36.25Gyin5
fx
304 Low,intandhigh 48 2% None 97,93,75%
4-year actuarial
Freemanetal.47 7–7.25Gyin5fx 41 Low 60 <1% None 93%5-year
actuarial
Bolziccoetal.42 35Gyin5fx 100 Low,intandhigh 36 None None 96%
McBrideetal.51 36.25–37.5Gyin5
fx
45 Low 44 <1% None 100%
Juetal.50 35–36.25Gyin5
fx
41 Int 21 None None 97.56%
Chenetal.49 35–36.25Gyin5
fx
100 Low,intandhigh 26 None None 99%
Kangetal.37 32–36Gyin4fx 44 Low,intandhigh 40 None None 100%,100%,
90.9% Oliaietal.48 37.5Gyvs.
35–36.25Gyin5 fractions
70 Low,intandhigh 27–37 4% None 100%,95%,
77.1%3-years Kingetal.22 36.25Gyin4–5
fractions
1100 Low,intandhigh 36 – – 93%5-years
FFBF:freefrombiochemicalfailure;int.:intermediate;GU:genitourinary;GI:gastrointestinal.
withaminimumof5yearsoffollow-up,the5-yearBFFrate forlow- and intermediate-risk patients was 99% and 93%, respectively.22
DespitethelargeuseoftheCyberknifeinthedeliveryof SBRTtreatmentsforPCpatients,severalreportsontheuseof linearaccelerators(LINAC)havebeenpublished.52–57
Madsen et al.52 reported the clinical experience on 40
prostatecancerpatientstreatedwith33.5Gy in5fractions. Withamedianfollow-upof41months,the4-yearBFFwas 90%.Acutegrade3GUtoxicitywasregisteredin5%ofcases, whilenograde3latetoxicitywasreported.
Boikeetal.53enrolled45patientsinamulti-institutional
prospectivedose-escalationstudytoevaluatethe maximum-tolerated dose (MTD) of five fractions of SBRT: groups of 15 patients received 45Gy, 47.5Gy, and 50Gy in five frac-tions. The overall incidence of G3+ GI and GU toxicities were 2 and 4%, respectively. The authors concluded that doseescalationto50Gy wasfeasibleandtheMTDwasnot reached.
Alongietal.54reportedaprospectivephaseI–IIstudy
eval-uatingthefeasibilityandearlysideeffectsofashortcourse hypo-fractionatedSBRTdeliveredwithvolumetricmodulated arctherapy(VMAT)andflatteningfilterfree(FFF)beams.After amedianfollow-upof11months,40patientswereenrolled: noacuteG3(orhigher)toxicitywasrecorded.Moreover,agood
patient-reportedQOLperceptionwasreportedforthefirstyear aftertreatment.55
Loblawetal.56conductedaphaseI-IIstudytoreportthe
efficacyandthesafetyoutcomesofpatientswithalowriskPC treatedonceweeklywithSBRT(35Gyin5fractions),delivered withastandardLINAC.Authorsreportedacutegrade≥3GI andGUtoxicityof0%and1%,respectively,andlategrade≥3 GIandGUtoxicityof1%forboth.Post-treatmentbiopsieswere negativein96%ofthepatientsandthe5-yearBFFwas98%.
Table1reportedtheavailabledataonSBRTforPC. Uptonow,nosignificantclinicalordosimetricdifferences have been showed in the published studies, and no com-parativestudieshavebeenperformed.Finally,noneofthese techniquesofirradiationcould beconsidered superiorover theotherandthechoicecouldbemadeinthesingle radiothe-rapydepartment,takingintoaccountlocalavailabilityofthe machines,theirintrinsicplanninganddeliverytime(shorter fortechniquesotherthanCyberknife)andlocalmedicaland physicsexpertise.57
5.
Conclusion
Recent technological developments, combined with an improvedknowledgeofradiobiologicalmodelsinfavorofa
highsensitivityofPCtolargerfractionsizesare openinga newscenarioinitstreatment.Indeed,selectedpatientswill probablybenefit from the feasibilityofhigh focused RT in oneorfewfractionswithrobustdoseconformalityand mod-ulation,witharapiddosefalloffanddeliveredwithhigher accuracy.Theold “paradigm”ofthestandarddose fraction-ation(35–40sessions),assumedastheoptimalcompromise betweenefficacyandsafety,israpidlychangingwiththe intro-ductionofmodernradiationtechniques.58Thecombinationof
IGRTandIMRT/VMATinthecontextofSBRTtreatmentsallows thedeliveryofhighertotalbiologicalequivalentdosesand/or higherdoseperfraction.
Althoughmorematureresultsare needed,the available experienceswithpatientswithmorethan5yearsoffollowup seemtosupportthiswidediffusionofSBRTinthetreatment ofwellselectedPCpatients.Theongoingrandomizedclinical trialswilladdimportantclinicalcomparativedataandallowa moreprecisedefinitionofabetterfractionation,efficacyand safetyofSBRTinthetreatmentofPCpatients(as,for exam-ple,inthe trialsNCT01737151,NCT01584258,NCT01764646, NCT01434290availableonlineatwww.clinicaltrials.gov).
Conflict
of
interest
Nonedeclared.Financial
disclosure
Nonedeclared.Acknowledgements
None.r
e
f
e
r
e
n
c
e
s
1. NCCN.Availablefrom: www.nccn.org/professionals/physiciangls/pdf/prostate.pdf [accessed24.06.14].2. HeidenreichA,BellmuntJ,BollaM,JoniauS,MasonM, MatveevV,etal.Part1:screening,diagnosis,andtreatment ofclinicallylocaliseddisease.EurUrol2011;59(1):61–71.
3. MottetN,BellmuntJ,BollaM,JoniauS,MasonM,MatveevV, etal.EAguidelinesonprostatecancer,PartII:Treatmentof advanced,relapsing,andcastration-resistantprostate cancer.EurUrol2011;59(4):572–83.
4. DeBariB,FiorentinoA,ArcangeliS,FrancoP,D’AngelilloRM, AlongiF.Fromradiobiologytotechnology:whatischanging inradiotherapyforprostatecancer.ExpertRevAnticancerTher
2014;14(5):553–64.
5. LenguaRE,GonzalezMF,BarahonaK,IxquiacME,LuceroJF, MontenegroE,etal.Toxicityoutcomeinpatientstreated withmodulatedarcradiotherapyforlocalizedprostate cancer.RepPractOncolRadiother2013;19(October4):234–8.
6. DavidsonMT,BlakeSJ,BatchelarDL,CheungP,MahK. Assessingtheroleofvolumetricmodulatedarctherapy (VMAT)relativetoIMRTandhelicaltomotherapyinthe managementoflocalized,locallyadvanced,and post-operativeprostatecancer.IntJRadiatOncolBiolPhys
2011;80(5):1550–8.
7. PietersBR,deBackDZ,KoningCC,ZwindermanAH. Comparisonofthreeradiotherapymodalitiesonbiochemical controlandoverallsurvivalforthetreatmentofprostate cancer:asystematicreview.RadiotherOncol2009;93(2): 168–73.
8. UdrescuC,DeBariB,RouvièreO,etal.Doeshormone therapymodifythepositionofthegoldmarkersinthe prostateduringirradiation?Adailyevaluationwith kV-images.CancerRadiother2013;17(3):215–20.
9. UdrescuC,JaladeP,DeBariB,RuffionA,Michel-AmadryG, JaladeP.Evaluationoftherespiratoryprostatemotionwith four-dimensionalcomputedtomographyscanacquisitions usingthreeimplantedmarkers.RadiotherOncol
2012;103(2):266–9.
10. StaffurthJ,RadiotherapyDevelopmentBoard.Areviewofthe clinicalevidenceforintensity-modulatedradiotherapy.Clin Oncol2010;22(8):643–57.
11. BujoldA1,CraigT,JaffrayD,DawsonLA.Image-guided radiotherapy:hasitinfluencedpatientoutcomes?Semin RadiatOncol2012;22(1):50–61.
12. DeBariB,FiorentinoA,GretoD,CiammellaP,ArcangeliS, AvuzziB,etal.Prostatecancerasaparadigmof
multidisciplinaryapproach?HighlightsfromtheItalian youngradiationoncologistmeeting.Tumori
2013;99(November–December(6)):637–49.
13. MiralbellR,RobertsSA,ZubizarretaE,HendryJH. Dose-fractionationsensitivityofprostatecancerdeduced fromradiotherapyoutcomesof5,969patientsinseven internationalinstitutionaldatasets:a/b=1.4(0.9−2.2)Gy.IntJ RadiatOncolBiolPhys2012;82(1):e17–24.
14. HernándezTG,GonzálezAV,PeidroJP,FerrandoJV,González LB,Caba ˜neroDG,etal.Radiobiologicalcomparisonoftwo radiotherapytreatmenttechniquesforhigh-riskprostate cancer.RepPractOncolRadiother2013;18(February(5)):265–71.
15. HartfordAC,GalvinJM,BeyerDC,EichlerTJ,IbbottGS, KavanaghB,etal.AmericanCollegeofRadiology(ACR)and AmericanSocietyforRadiationOncology(ASTRO)practice guidelineforintensity-modulatedradiationtherapy(IMRT).
AmJClinOncol2012;35(6):612–7.
16. BaumanG,RumbleRB,ChenJ,LoblawA,WardeP,Members oftheIMRTIndicationsExpertPanel.Intensity-modulated radiotherapyinthetreatmentofprostatecancer.ClinOncol
2012;24(7):461–73.
17. ZaorskyNG,HarrisonAS,TrabulsiEJ,GomellaLG,Showalter TN,HurwitzMD,etal.Evolutionofadvancedtechnologiesin prostatecancerradiotherapy.NatRevUrol2013;10(10):565–79.
18. ArcangeliS,ScorsettiM,AlongiF.WillSBRTreplace
conventionalradiotherapyinpatientswithlow-intermediate riskprostatecancer?Areview.CritRevOncolHematol
2012;84:101–8.
19. BijlaniA,AguzziG,SchaalDW,RomanelliP.Stereotactic radiosurgeryandstereotacticbodyradiationtherapy cost-effectivenessresults.FrontOncol2013;3(April):77.
20. SherDJ,ParikhR,Mays-JacksonS,PungliaRS.
Cost-effectivenessanalysisofSBRTversusIMRTforlow-risk prostatecancer.AmJClinOncol2014;37(3):215–21.
21. AminNP,SherDJ,KonskiAA.Systematicreviewofthecost effectivenessofradiationtherapyforprostatecancerfrom 2003to2013.ApplHealthEconHealthPolicy2014;12(August (4)):391–408.
22. KingCR,FreemanD,KaplanI,FullerD,BolziccoG,CollinsS, etal.Stereotacticbodyradiotherapyforlocalizedprostate cancer:pooledanalysisfromamulti-institutional consortiumofprospectivephaseIItrials.RadiotherOncol
2013;109(2):217–21.
23. BrennerDJ,MartinezAA,EdmundsonGK,MitchellC,Thames HD,ArmourEP.Directevidencethatprostatetumorsshow highsensitivitytofractionation(lowalpha/betaratio),similar
tolate-respondingnormaltissue.IntJRadiatOncolBiolPhys
2002;52(1):6–13.
24. DasuA.Isthealpha/betavalueforprostatetumourslow enoughtobesafelyusedinclinicaltrials?ClinOncol(RColl Radiol)2007;19(5):289–301.
25. WilliamsSG,TaylorJM,LiuN,TraY,DuchesneGM,KestinLL, etal.Useofindividualfractionsizedatafrom3756patients todirectlydeterminethealpha/betaratioofprostatecancer.
IntJRadiatOncolBiolPhys2007;68:24–33.
26. PediciniP,StrigariL,BenassiM.Estimationofa self-consistentsetofradiobiologicalparametersfrom hypofractionatedversusstandardradiationtherapyof prostatecancer.IntJRadiatOncolBiolPhys2013;85:e231–7.
27. JoinerM,vanderKogelA.Basicclinicalradiobiology.4thed. Arnold;2009.
28. LukkaH,HayterC,JulianJA,WardeP,MorrisWJ,
GospodarowiczM,etal.Arandomizedtrialcomparingtwo fractionationschedulesforpatientswithlocalizedprostate cancer.JClinOncol2005;23:6132–8.
29. YeohEE,BottenRJ,ButtersJ,DiMatteoAC,HollowayRH, FowlerJ.Hypofractionatedversusconventionallyfractionated radiotherapyforprostatecarcinoma:finalresultsofphaseIII randomizedtrial.IntJRadiatOncolBiolPhys2011;81:1271–8.
30. KubanDA,Nogueras-GonzalezNG,HamblinL,LeeAK,Choi S,FrankSJ,etal.Preliminaryreportofarandomizeddose escalationtrialforprostatecancerusinghypofractionation.
IntJRadiatOncolBiolPhys2010;78(Suppl.):S58.
31. PollackAW,WalkerG,BuyyounouskiM,HorwitzE,PriceR, FeigenbergS,etal.Fiveyearresultsofarandomizedexternal beamradiotherapyhypofractionationtrialforprostate cancer.IntJRadiatOncolBiolPhys2011;81(Suppl.):S1.
32. ArcangeliS,StrigariL,GomelliniS,SaracinoB,PetrongariMG, PinnaròP,etal.Updatedresultsandpatternoffailuresina randomizedhypofractionationtrialforhigh-riskprostate cancer.IntJRadiatOncolBiolPhys2012;84:1172–8.
33. DearnaleyD,SyndicusI,SumoG,BidmeadM,BloomfieldD, ClarkC,etal.Conventionalversushypofractionatedhigh doseintensity-modulatedradiotherapyforprostatecancer: preliminarysafetyresultsfromCHHiPrandomizedcontrolled trial.LancetOncol2012;13:43–54.
34. Garcia-BarrosM,ParisF,Cordon-CardoC,LydenD,RafiiS, Haimovitz-FriedmanA,FuksZ,KolesnickR.Tumorresponse toradiotherapyregulatedbyendothelialcellapoptosis.
Science2003;300:1155–9.
35. FuksZ,KolesnickR.Engagingthevascularcomponentofthe tumorresponse.CancerCell2005;8:89–91.
36. AlongiF,DeBariB,ScorsettiM.Couldsingle-highdose radiotherapybeconsideredthenewfrontierofstereotactic ablativeradiationtherapy?Tumori2014;100:e87–8.
37. KangJK,ChoCK,ChoiCW,YooS,KimMS,YangK,etal. Image-guidedstereotacticbodyradiationtherapyfor localizedprostatecancer.Tumori2011;97:43–8.
38. ZeriniD,Jereczek-FossaBA,VavassoriA,Bossi-ZanettiI, MauroR,IvaldiGB,etal.3D-conformalhypofractionated radiotherapyforprostatecancerwithdailytransabdominal ultrasonographyprostatelocalization:toxicityandoutcome ofapilotstudy.Tumori2010;96:941–6.
39. ChoiC,ChoG,KimK,ParkK,JoM,LeeC,etal.Stereotactic radiationtherapyoflocalizedprostatecancerusing cyberknife.IntJRadiatOncolBiolPhys2007;69:S375.
40. FriedlandJL,FreemanDE,Masterson-McGaryME,Spellberg DM.Stereotacticbodyradiotherapy:anemergingtreatment approachforlocalizedprostatecancer.TechnolCancerRes Treat2009;8(5):387–92.
41. BolziccoG,FavrettoMS,ScreminE,TamboneC,TascaA, GuglielmiR.Image-guidedstereotacticbodyradiation therapyforclinicallylocalizedprostatecancer:preliminary clinicalresults.TechnolCancerResTreat2010;9(5):473–7.
42. BolziccoG,FavrettoMS,SatarianoN,ScreminE,TamboneC, TascaA.Asingle-centerstudyof100consecutivepatients withlocalizedprostatecancertreatedwithstereotacticbody radiotherapy.BMCUrol2013;13:49.
43. KatzAJ,SantoroM,AshleyR,DiblasioF,WittenM. Stereotacticbodyradiotherapyfororgan-confinedprostate cancer.BMCUrol2010;10:1.
44. KatzAJ,SantoroM,DiblasioF,AshleyR.Stereotacticbody radiotherapyforlocalizedprostatecancer:diseasecontrol andqualityoflifeat6years.RadiatOncol2013;8(1):118.
45. KingC.Stereotacticbodyradiotherapyforprostatecancer: currentresultsofaphaseIItrial.FrontRadiatTherOncol
2011;43:428–37.
46. BhattasaliO,ChenLN,WooJ,ParkJW,KimJS,MouresR,etal. Patient-reportedoutcomesfollowingstereotacticbody radiationtherapyforclinicallylocalizedprostatecancer.
RadiatOncol2014;9:52.
47. FreemanDE,KingCR.Stereotacticbodyradiotherapyfor low-riskprostatecancer:five-yearoutcomes.RadiatOncol
2011;6:3.
48. OliaiC,LancianoR,SprandioB,YangJ,LamondJ,ArrigoS, etal.Stereotacticbodyradiationtherapyfortheprimary treatmentoflocalizedprostatecancer.JRadiatOncol
2013;2(1):63–70.
49. ChenLN,SuyS,UhmS,OermannEK,JuAW,ChenV,etal. Stereotacticbodyradiationtherapy(SBRT)forclinically localizedprostatecancer:theGeorgetownUniversity experience.RadiatOncol2013;8:58.
50. JuAW,WangH,OermannEK,ShererBA,UhmS,ChenVJ, etal.Hypofractionatedstereotacticbodyradiationtherapyas monotherapyforintermediate-riskprostatecancer.Radiat Oncol2013;8:30.
51. McBrideSM,WongDS,DombrowskiJJ,HarkinsB,TapellaP, HanscomHN,etal.Hypofractionatedstereotacticbody radiotherapyinlow-riskprostateadenocarcinoma:
preliminaryresultsofamulti-institutionalphase1feasibility trial.Cancer2012;118(15):3681–90.
52. MadsenBL,HsiRA,PhamHT,FowlerJF,EsaguiL,CormanJ. Stereotactichypofractionatedaccurateradiotherapyofthe prostate(sharp),33.5Gyinfivefractionsforlocalizeddisease: firstclinicaltrialresults.IntJRadiatOncolBiolPhys
2007;67(4):1099–105.
53. BoikeTP,LotanY,ChoLC,BrindleJ,DeRoseP,XieXJ,etal. PhaseIdose-escalationstudyofstereotacticbodyradiation therapyforlow-andintermediate-riskprostatecancer.JClin Oncol2011;29:2020–6.
54. AlongiF,CozziL,ArcangeliS,IftodeC,ComitoT,VillaE,etal. LinacbasedSBRTforprostatecancerin5fractionswith VMATandflatteningfilterfreebeams:preliminaryreportofa phaseIIstudy.RadiatOncol2013;8(1):171.
55. ScorsettiM1,AlongiF,ClericiE,ComitoT,FogliataA,IftodeC, etal.Stereotacticbodyradiotherapywithflatteningfilter-free beamsforprostatecancer:assessmentofpatient-reported qualityoflife.JCancerResClinOncol2014,
http://dx.doi.org/10.1007/s00432-014-1732-1.
56. LoblawA,CheungP,D’AlimonteL,DeabreuA,MamedovA, ZhangL,etal.Prostatestereotacticablativebody
radiotherapyusingastandardlinearaccelerator:toxicity, biochemical,andpathologicaloutcomes.RadiotherOncol
2013;107(2):153–8.
57. MacdougallND,DeanC,MuirheadR.Stereotacticbody radiotherapyinprostatecancer:israpidarcabettersolution thancyberknife?ClinOncol(RCollRadiol)2014;26(1):4–9.
58. PegurriL,BuglioneM,GirelliG,GuarnieriA,MeattiniI, RicardiU,etal.Changesinpatternsofpracticeforprostate cancerradiotherapyinItaly1995–2003.Asurveyofthe ProstateCancerStudyGroupoftheItalianRadiation OncologySociety.Tumori2014;100(1):31–7.