University of Pisa
Department of Biology
Biology applied to Bio-Medical Sciences
Curriculum Pathophysiology
Master Thesis
“
Susceptibility alleles involved in
differentiated thyroid carcinoma risk”
CANDIDATE SUPERVISOR
Chiara Campo Prof. Federica Gemignani
Dr. Asta Försti
1
INDEX
1. INTRODUCTION
1.1 Thyroid gland: anatomy
1.2 Epidemiology: incidence and mortality
1.3 Origin of thyroid cancer
1.3.1 Classification of thyroid cancer
1.3.2 Well Differentiated Thyroid Carcinoma (WDTC)
1.4 Risk factors
1.4.1 Ionizing radiation exposure
1.4.2 Family history
1.4.3 Benign thyroid conditions
1.4.4 Hormonal and reproductive factors
1.4.5 Dietary risk factors: iodine intake and nutrient consumption
1.4.6 Body weight and insulin resistance
1.5 Genetic studies in WDTC
1.5.1 Germline mutations in WDTC
1.5.2 Sporadic mutations in WDTC
1.5.3 Single nucleotide polymorphisms in WDTC
2. AIM OF THE THESIS
3. MATERIALS AND METHODS
3.1 Association studies
3.1.1 Population
3.2 Gene and SNP selection
2
3.4 The Polymerase Chain Reaction (PCR)
3.4.1 Taqman PCR
3.4.2 KASPar SNP Genotyping System
3.5 Statistical analysis
3.6 In silico tools
3.6.1 SIFT and PolyPhen
3.6.2 HaploReg V2
3.6.3 MicroSNiPer
4. RESULTS
4.1 In silico prediction
3
ACRONYMS
WDTC Well Differentiated Thyroid Carcinoma PDTC Poorly-Differentiated Thyroid Carcinoma
ATC Undifferentiated or Anaplastic Thyroid Carcinoma PTC Papillary Thyroid Carcinoma
CPTC Classical Variant Papillary Thyroid Carcinoma TCPTC Tall Cell Variant Papillary Thyroid Carcinoma FVPTC Follicular Variant Papillary Thyroid Carcinoma FTC Follicular Thyroid Carcinoma
MTC Medullary Thyroid Carcinoma FTA Follicular Thyroid Adenoma SNP Single-nucleotide olymorphism MAF Minor Allele Frequency
LD Linkage Disequilibrium Tg Thyroglobulin
TRH Thyrotropin-releasing hormone TSH Thyroid-stimulating hormone TK Tyrosine kinase
MAPKK Mitogen-activated Protein Kinase
PPARs Peroxisome proliferator-activated receptors
PAX8/PARγ Paired box gene 8-peroxisome proliferator-activated receptor gamma VEGFRVascular Epithelial Growth Factor Receptor
4 IR Ionizing Radiation
UTR Untranslated Region
GWAS Genome-Wide Association Studies HWEHardy Weinberg Equilibrium
OD Odds Ratio CI Confidence Interval
SIFT Sorting Intolerant From Tolerant PolyPhen-2 Polymorphism Phenotyping v2 eQTL Expression Qualitative Trait Locus
5
ABSTRACT
Thyroid cancer is a common endocrine malignancy. It accounts about 1% of all oncological diseases. There are several histological types and subtypes of thyroid cancer with different cellular origins, characteristics and prognosis. The Well Differentiated Thyroid Carcinoma (WDTC) represents more than 90% of all the forms of thyroid cancer. Among them it is possible to distinguish between Papillary Thyroid Carcinomas (PTC) and Follicular Thyroid
Carcinomas (FTC). The thyroid cancer incidence in the world has been increasing in the past
years. Although thyroid nodules are frequent their rate of malignancy is low. Many individual and environment factors have been considered as risk factors for thyroid cancer. The purpose of my thesis was to identify possible genetic polymorphisms, selected in genes somatically mutated in WDTC. For the analysis of genetic single-nucleotide polymorphism (SNP) data we carried out a candidate-gene case-control study.
A case-control association study was conducted with patients with sporadic WDTC and healthy controls from an Italian population. We collected 3277 samples (1558 cases and 1719 controls) and we used the browser Cosmic to select our genes from the top genes somatically mutated in WDTC, especially considering those involved in PTC. Focusing on 5´ UTR variants, 3´UTR variants and missense variants, considering the global minor allele frequency (MAF) over 10% and the linkage disequilibrium (LD) between these SNPs, we selected 34 SNPs. We used TaqMan PCR and KASPar SNP Genotyping System to genotype all the individuals. The association between our polymorphisms and the risk of
WDTC was evaluated with a multivariate logistic regression analysis. The results of this study provides evidence that inherited variants in the APC, TSHR,
SMAD4, GNAS and EGFR genes can play a role in the etiology of thyroid cancer. We used
in silico methods to predict the effect of possible amino acid substitutions on protein function
6
INTRODUCTION
1.1 THYROID GLAND: Anatomy
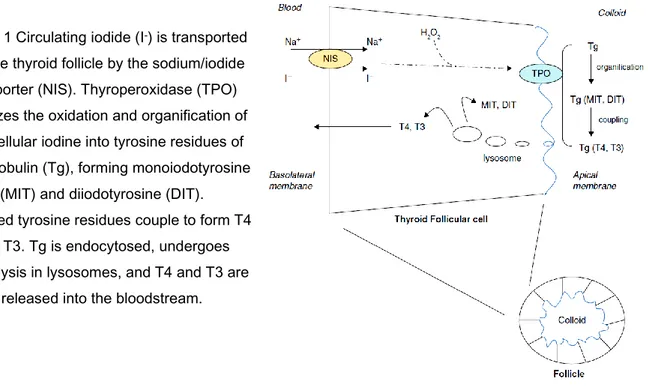
The thyroid is an endocrine gland. The correct function of this tiny gland is important for the human body because it regulates many metabolic processes, including growth and energy use. The thyroid is located in the anterior region of the neck, at the front of the neck. It consists of two lobes, the right lobe and the left lobe, connected by a middle part called isthmus. The thyroid is surrounded by a fibrous capsule; the back side is covered with muscles and it is located near by the parathyroid glands, small endocrine glands that secrete Parathyroid hormone [1]. Furthermore, it regulates, through Calcitonin, the metabolism of calcium and phosphorus. At the microscopic level the basic unit is the follicle, a cavity filled with colloid and surrounded by a layer of two epithelial cells: Follicular Cells secreting T3 and T4 hormones and C-Cells, located in the basal state of the thyroid follicle, secreting Calcitonin. The colloid is formed mainly of Thyroglobulin (Tg), which is stored within the center of thyroid follicles which constitutes a large reserve of performed hormone[2] Figure 1. Through lysosomal proteolysis the Tg release T3 and T4; in this way the thyroid hormones are available also during iodine deficiency.
Figure 1 Circulating iodide (I-) is transported
into the thyroid follicle by the sodium/iodide symporter (NIS). Thyroperoxidase (TPO) catalyzes the oxidation and organification of
intracellular iodine into tyrosine residues of thyroglobulin (Tg), forming monoiodotyrosine
(MIT) and diiodotyrosine (DIT). Iodinated tyrosine residues couple to form T4
and T3. Tg is endocytosed, undergoes proteolysis in lysosomes, and T4 and T3 are
7
Hormone secretion mainly involves Tireoxina (T4), which contains 4 iodine atoms, and
Triiodothyronine (T3), containing 3 atoms of iodine. These are hormones circulating in the
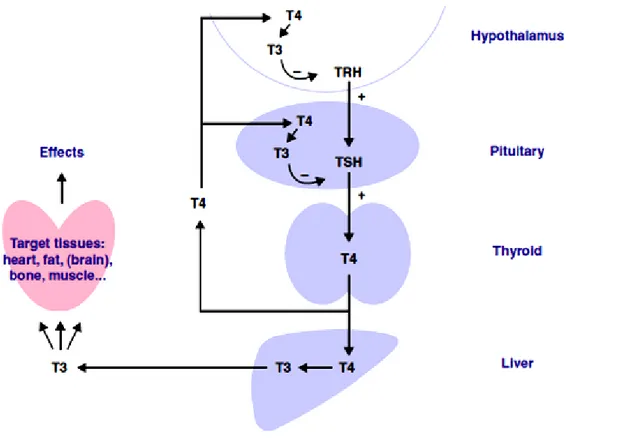
bloodstream in association with protein structures that carry them to the tissues, where they are released. In normal health most T3 circulating in the bloodstream has been converted from T4. Both T4 and T3 have the same action on the body´s cells; these free hormones enter the cell and mediate their effects through specific nuclear receptors which are distributed among tissues. T3 is more potent and it binds the thyroid hormone receptor with higher affinity than T4. For this reason T3 is often defined as the “active” ligand and T4 as the prohormone. In fact the majority of thyroid hormone secreted by the gland in the form T4 is later converted to T3 by deiodination in peripheral tissues. Thyroid hormone regulates the metabolic rate of almost all the cells of the body, and influences the health of the heart, brain and bones. These hormones secretion is regulated by the hypothalamic-pituitary-thyroid axis [3]. In particular, the thyrotropin-releasing hormone (TRH), produced by the hypothalamus, promotes the release of the thyroid-stimulating hormone (TSH) by the anterior pituitary gland which has the function to increase the secretion of thyroid hormones Figure 2
8
The TSH is a glycoprotein formed from two subunits α and β. It binds to a specific receptor present on the thyroid cells membrane and it promotes proliferation and cell differentiation, facilitating the uptake of iodine, the synthesis of Tg and thyroid hormones. Thyroid hormones are composed mainly of iodine which is primarily derived from the diet. Ingested iodine is assimilated from the stomach and intestine and with the circulation it becomes usable for uptake into the thyroid gland. The thyroid follicular cells can concentrate iodine and incorporate it into thyroid hormone. The reduction of circulating hormones is often associated with an iodine deficiency. A low intake of iodine in the diet increases, in fact, the levels of TSH resulting in an increase in the size of the gland in order to stimulate hormone secretion, thus forming the so-called goiter. Both active thyroid hormones T4 and T3 exert negative feedback upon the hypotalamus and the pituitary gland [4].
9
1.2 EPIDEMIOLOGY: Incidence and mortality
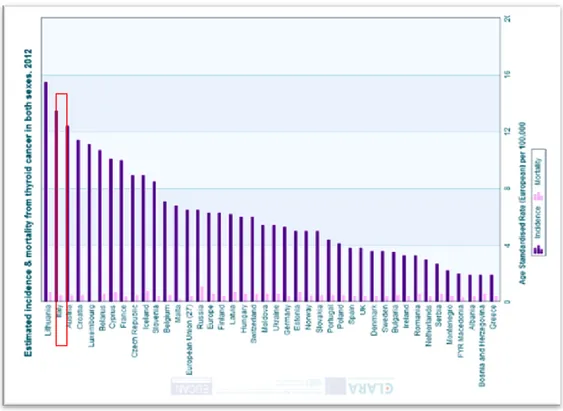
Thyroid cancer is a common endocrine malignancy. It is generally estimated that thyroid carcinoma comprises approximately 1% of all malignancies but it accounts for more than 90% of all endocrine malignancies [5]. Although thyroid nodules are frequent, their rate of malignancy is low; thyroid cancer has been considered a disease with excellent prognosis. Distant metastases are present in a small percentage of cases (1-3%), these characteristics are predictors of cancer associated with recurrence and mortality [6]. Thyroid cancer incidence has continuously increased in the last three decades all over the world [7]. Explanations for the increasing thyroid cancer incidence are controversial. Some experts suggest that the rise in the number of new cancers is due to the increased diagnostic intensity; other experts believe that this increase is associated to environmental factors and lifestyle changes. Thus, this increase might be due to a combination of true occurrence of the disease and also reflect more sensitive diagnostic procedures, higher exposure to radiation for diagnostic scrutiny and others risk factors not specific for thyroid. The more sensitive diagnostic procedures and biochemical markers have given the possibility to raise the discovery for many types of cancer, identifying also unrecognized forms in the preclinical stage for years or decades [8]. The combination of the ability to detect small nodules and then aspirate their contents has clearly facilitated the diagnosis of these smaller cancers. Genetic factors, environmental influences, and access to medical care can easily explain the high variability in the thyroid cancer incidence by geographic area and ethnicity [9]. The lowest rates of thyroid cancer were observed in blacks, the greatest rate of papillary thyroid cancer acceleration occurs in black females. Male and female annual percent increase was 6.3% and 7.1% for white patients, 4.3% and 8.4% for black, 4.2% and 6.7% for Hispanic and 3.4% and 6.4% for Asian/Pacific Islander patients, respectively [10]. Only in a few countries (Norway, Sweden) thyroid cancer incidence was decreased. The overall survival rate has remained at 90% to 95% in recent decades according to a Surveillance, Epidemiology, and End Results (SEER 2012) reportFigure 3. The joint point trend reported by SEER for the period 1988–2009 indicated a significant increase of thyroid cancer mortality (+0.8% annual percent change), primarily in males.
10
In Italy, some of the highest incidence rates of thyroid cancer worldwide have been reported
[11]. Considering both sexes, Italy takes the second place after Lituania Figure 4. Figure 3 SEER incidence and US Death Rates of Cancer of the Thyroid for Both Sexes, based on
November 2012 SEER data submission. Joint Point Analyses for Whites and Blacks from 1975-2010 and for Asian/Pacific Islanders, American Indians/Alaska Natives and Hispanics from 1992-2010.
(http://seer.cancer.gov/statfacts/html/thyro.html)
Browse the SEER Cancer Statistics Review 1975-2010
Figure 4 Estimated incidence, mortality & prevalence for both sexes, 2012. (http://eco.iarc.fr/eucan/Cancer.aspx?Cancer=35)
11
1.3 ORIGIN OF THYROID CANCER
Nodules of the thyroid gland are common. It is estimated that 4-7% of adults have a palpable thyroid nodule, and many have nodules which are recognizable at autopsy or by ultrasound. Most differentiated thyroid cancer patients have a very good prognosis if diagnosed at early stages, and 91% of patients are alive after 20 years when the classical treatment with surgery followed by radioiodine ablation and suppression of TSH is employed [12].
An anatomic pathology analysis of thyroid cancer gives the possibility to make a diagnosis about his benignity or malignancy and to distinguish the different ways in which it can manifest itself. In particular, concerning cellular origin, we can consider:
Tumors with parafollicular origin: From the de-differentiation of parafollicular or C-cells comes only a malignant form of the cancer: Medullary Thyroid Carcinoma
(MTC), which represents about 3-5% of cases.
Tumors with follicular origin: They represent more than 95% of thyroid cancer. The analysis of the architectural features makes it possible to distinguish benign from malignant follicular thyroid neoplasms. Thyroid tumors that originate from follicular epithelium include: benign forms, known as Adenomas, and malignant forms,
Carcinomas, which can be divided to the papillary and the follicular carcinomas (PTC
and FTC, respectively).
The specificity of genetic lesions found suggests independent origins of PTC and FTC; there are also some clear genetic evidences to support the idea that FTC represents the progression of Follicular Thyroid Adenomas (FTA). The development of FTC from FTA has been demonstrated in studies of experimental carcinogenesis in the rat [13]. At the initial phase of reversible pre-neoplastic lesions a latency period is followed by the formation of neoplastic atypias, the acquisition of invasiveness and the ability to metastasize. The onset of tumors, induced experimentally, has allowed the scientists to identify the action of agents promoting carcinogenesis and their ability to reduce the latency period, favoring the tumor progression.
12
1.3.1 Classification of thyroid cancer
There are several histological types and subtypes of thyroid cancer with different cellular origins, characteristics and prognosis. They can be classified into [14]:
- Well-Differentiated Thyroid Carcinomas (WDTC): This group represents more than 90% of all forms of thyroid cancer tumors. They have well-defined morphological and cytogenetic characteristics; in fact, they maintain the original structure of the thyroid gland. We can distinguish between Papillary Carcinomas (Papillary Thyroid Carcinoma or PTC) and Follicular Carcinomas (Follicular Thyroid Carcinoma or FTC).
- Poorly-Differentiated Thyroid Carcinomas (PDTC): This group of tumors has a biological behavior and an intermediate prognosis between undifferentiated and differentiated forms. They have a strong tendency to spread through the blood or the lymphatic system.
- Undifferentiated or Anaplastic Thyroid Carcinomas (ATC): This tumor type represents about 5% of all thyroid malignancies. It is highly malignant tumor whose cells have an irregular structure and the tissues are devoid of differentiation. It is a particularly aggressive form with an early development of distant metastasis, spreading by the lymphatic system or via blood [15]. This form is in many cases the terminal phase of de-differentiation process of a FTC or PTC. The anaplastic cells are not able to produce and to transport Tg iodine.
The initial clinical sign of the processes associated with tumorigenesis is generally a swelling of the thyroid gland which occurs in 80% of cases in a single lump, but can also be multinodular and have the appearance of a diffuse swelling in a lobe or in the whole thyroid. In the differentiated forms the swelling has almost always, in the initial phase, the appearance of a smooth lump, mobile with defined outlines and a slow growth. In advanced stages, the swelling has soft edges and irregular surface, its growth is rapid and the swelling always occurs from a pre-existing differentiated neoplastic nodule [16].
13
1.3.2 Well Differentiated Thyroid Carcinomas (WDTC)
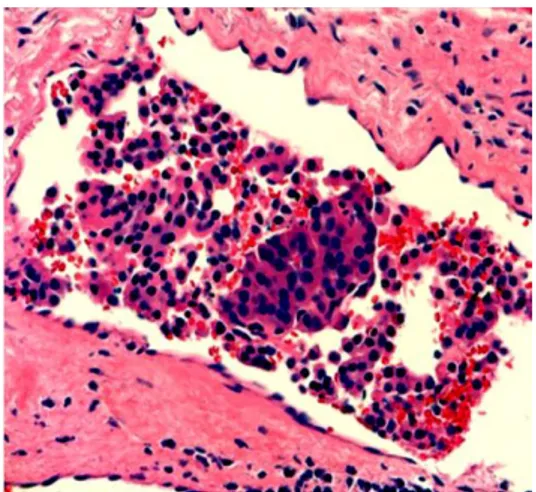
In general, the majority of all thyroid cancers are well-differentiated; they retain several typical features of normal follicular cells: TSH addiction, synthesis of Tg, ability to take up iodine. They have a more favorable mortality outcome and recurrence rate, compared to patients with MTC and ATC. However, the worst prognosis is usually observed with any type of thyroid cancer that has aggressively invaded through the thyroid capsule Figure 5 or metastasized to distant organs; otherwise distant metastasis is relatively rare among WDTC. The lungs and the bones are the most common sites of spread and can dramatically increase mortality rates [17].
The papillary carcinoma Figure 6 is the most common histological type of thyroid cancer and it is frequently multicentric. It is characterized by papillary structures and invaginations of the cytoplasm into the nucleus. This tumor is frequently unencapsulated, often multifocal and bilateral. There are several histologic variants of PTC, such as: the classical variant (cPTC),
the tall cell variant (tcPTC), the follicular variant (fvPTC) and the variant microcarcinoma.
A microscopic view shows in the cPTC, which is the most common form, the presence of papillae with connective-axis vasculature [18]. Most PTCs occur in adults from 20 to 50 years of age but can develop, also, in children and in the elderly. There is a female predominance, with a female to male ratio of 4:1. There is an association with environmental (iodine deficiency) and genetics factors. Prior radiation exposure to the thyroid is an important risk factor but many PTC occur in patients with no radiation history. PTCs are often slow-growing tumors; they metastasis to regional lymph-nodes and rarely progress to more aggressive disease [19].
The follicular carcinoma Figure 7 accounts for 5-15% of thyroid carcinomas overall, but is more prevalent in iodine-deficient areas of the world where the incidence is 20-40%. The FTC usually occurs as a single thyroid nodule, more or less encapsulated. It consists of small follicles, more or less differentiated, overlapping nuclei and poor or absent colloid. Their cells are not distinguishable from the ones of FTA Figure 8 therefore the diagnosis of malignancy is based on the infiltration of capsule and vessels. FTC is separated into two main groups
14
with important prognostic significance: widely invasive and minimally invasive. The ability to invade the capsule defines its nature to more or less invasive; its prognosis, in fact, is aggravated by increasing degree of (angio)invasion. Metastasis occurs mainly through blood [20].
Figure 5 Vascular invasion in widely invasive follicular carcinoma.
Figure 7 Follicular adenoma. Capsule separates adenoma (right) from non-neoplastic thyroid. Follicles in adenoma are more densely packed.
Figure 8 Follicular carcinoma. Figure 6 Papillary carcinoma.
Classical variant, showing papillary architecture. Nuclei are crowded and overlapping, elongated,
15
1.4 RISK FACTORS
The main risk factors for thyroid cancer, highlighted in epidemiological studies, are:
- Ionizing radiation exposure - Family history
- Benign thyroid conditions
- Hormonal and reproductive factors
- Dietary risk factors: iodine intake and nutrient consumption - Body weight and insulin resistance
1.4.1 Ionizing radiation exposure
Exposure to ionizing radiation (IR) is a proven risk factor for thyroid cancer. Thyroid gland seems to be an organ particularly vulnerable to IR. The thyroid may be irradiated more than other tissues because of its ability to concentrate the iodine and its position in the body. Risk depends on dose received, age at exposure, and sex. In general, the risk increases with larger doses and with younger age at treatment [21]. Sources of such radiation include certain medical treatment, thyroid disorders appear in patients treated with radiotherapy for head and neck cancer [22]. Radiation fallout from nuclear catastrophes (Hiroshima, Nagasaki, Chernobyl, Fukushima) has been associated with a significant increase in the incidence of thyroid gland carcinoma, showing an increased risk of pituitary gland tumors [23,24]. The risk of IR for thyroid cancer has recently been validated in the population exposed to radionuclides after the Chernobyl fallout [25]. Some studies reported an association between the thyroid cancer and the exposure to IR from the Chernobyl accident, which exposed millions of people to radioactivity in 1986. The accident caused large uncontrolled radioactive release into the environment and large quantities of radioactive substances were released into the air. Two radionuclides, the short-lived iodine-131 and the long-lived caesium-137, were particularly significant for the radiation dose released into the
16
environment. Their specific temporal and geographic distribution was suggestive of a common causative event in the development of the malignancy which was later proved to be internal exposure to I131 through its incorporation into food chains of pastured cows and further consumption of fresh milk. PTC among individuals exposed to radioactive iodine during their childhood or adolescence was the most important health consequence recognized after the Chernobyl accident.
1.4.2 Familial history
Inherited genetic susceptibility has an important role in the predisposition to cancer and it is now a well-established fact. Familial susceptibility, especially for medullary carcinoma (MTC), has been known for a long time and genetic factors are considered to be responsible for 20-25% of this type of thyroid cancer. The familial risks of MTC may be the highest ever reported in the population based studies [26]. In particular germ-line mutations in the RET gene are responsible for the hereditary tumor syndrome and the familial MTC [27].
Some studies have confirmed an association between a family history of benign thyroid cancer and a risk of thyroid cancer. The risk of thyroid cancer is increased for persons with a mother, sister, or aunt with a history of benign thyroid cancer, and there is a clear upward trend in risk with an increasing number of affected female relatives (P<0.0001). Stratification by age at diagnosis of the case proved that individuals aged ⩽35 years, who had an affected first or second/third-degree relative(s), had an approximately 3-fold increased risk of the cancer [28]. A population-level study showed high familial aggregation for defined thyroid diseases (Graves´ disease and goiter susceptibility). Shared lifestyle among family members seems to explain only a small proportion of the familial risk, but the known and unknown environmental factors may interact with the susceptibility genes which may complicate gene finding studies [29].
17
1.4.3 Benign thyroid conditions
Benign nodules/adenomas and goiter are considered to be risk factors for thyroid cancer [30]. The majority of thyroid nodules are asymptomatic but they are frequently evaluated by a specialist because they may represent malignancy [31]. Whether a thyroid nodule is benign or malignant is a major clinical dilemma but recent advances in markers for thyroid malignances suggest that some benign nodules have malignant potential. In particular some studies have attempted to use immunohistochemical markers to characterize follicular lesions with uncertain malignant potential, in order to define if benign nodules, including follicular adenomas, hyperplastic lesions, and Hurthle cell adenomas, are premalignant [32].
1.4.4 Hormonal and reproductive factors
The excess risk for thyroid cancer in women, compared to man, and events linked to reproductive and menstrual history have been suggested to be of relevance in thyroid cancer etiology. Several lines of evidence suggest that female sex hormones play a role in the etiology of thyroid cancer. Women have a higher incidence than men in virtually all geographical areas and ethnic groups, particularly before menopause. Moreover, pregnancy and some hormonal treatments have been associated with thyroid cancer among women [33]. Pregnancy, menarche and oral contraceptive are associated with growth of the thyroid gland and with increased serum levels of total T4 and T3. Female hormones may cause an elevation of TSH levels, leading in turn to thyroid hyperplasia and possibly cancer; experimentally increased TSH secretion has been shown to cause thyroid tumors in rodents [34]. A study, investigating the association of reproductive factors with risk of thyroid cancer in postomenual women, found a little support for associations of hormonal factors with risk of developing thyroid cancer [35]. However, previous epidemiologic studies have yielded inconsistent results regarding the role of hormonal and reproductive factors in the development of thyroid cancer. The results from a prospective study of 312 thyroid cancer cases among 187.865 postmenopausal women do not support a strong role for the examined female hormonal and reproductive factors in the etiology of postmenopausal cancer [36]. Therefore, further researches are needed to clarify the controversies about this association.
18
1.4.5 Dietary risk factors: iodine intake and nutrient
consumption
The wide geographical variation of thyroid cancer incidence suggests a relevant impact of environmental exposures and nutrition factors as candidates for thyroid cancer risk factors. In particular some studies examined in animal models the association between thyroid cancer and fish or vegetable consumption that contains a variety of constituents known to inhibit carcinogenesis. The relationship between iodine intake and the pathogenesis of thyroid carcinoma is complex. Iodine deficiency may induce an increasing incidence of benign thyroid conditions, but very high iodine intake also affects thyroid function and thyroid cancer risk. Iodine is essential for the normal function of the thyroid and ecological studies have suggested that thyroid cancer is more frequent both in areas with iodine deficiency (FTC) and iodine excess (PTC) [7]. PTC is more prevalent in iodine-sufficient areas and its frequency increases after iodine prophylaxis, a phenomenon also accompanied by a decrease in PTC size and an attenuation of malignant phenotype. Iodine deficiency-associated thyroid cancer has been linked with a specific molecular basis. RAS mutation in particular was more frequently present in FTC from iodine-deficient areas than that diagnosed in regions with sufficient iodine intake. It has also been discovered that iodine can prevent the progression of WDTC to anaplastic carcinoma by interfering with oncogene expression or the mutation of tumor suppressor genes such as BRAF, ERK, RAS, and TP53
[37]. Animal experiments have shown a clear increase of thyroid cancer after a long iodine deficiency leading to increased TSH level. On that basis, overstimulation by TSH was considered to play a major role in the tumorigenesis of thyroid carcinoma because of the increased thyroid cell response to TSH, increased thyroid cell EGF-induced proliferation, decreased TGFβ1 production and increased angiogenesis, all phenomena connected to promotion of tumor growth [38]. However, recent studies have revealed that the serum levels of TSH are in fact not increased or are even decreased in persons with mild-to-moderate iodine deficiency.
19
1.4.6 Body weight and insulin resistance
Several malignancies have shown a strong correlation between obesity, cancer risk and mortality. Thyroid hormones, that are crucial during development and the anthropometric measurements, such as height, weight and body fat, are involved in thyroid disorders. The prevalence of obesity has increased worldwide over the past few decades, and a number of studies, predominantly in the United States and Europe, have examined the association of obesity and height with risk of thyroid cancer [38]. The majority of these studies are suggestive of a positive association of body mass index and possibly of height with the risk of thyroid cancer [39]. The body size affects the request of iodine and, therefore, indirectly the risk of tumor. Some case-control studies have shown an increased risk of thyroid cancer in patients with high Body Mass Index (BMI). In women, weight gain >14% appears to correlate positively with the onset of thyroid carcinoma. The effects of relative weight and weight gain on thyroid cancer risk were stronger in post- menopausal women than in premenopausal women [40] .Recent studies have demonstrated that insulin resistance and hyperinsulinemia, two typical characteristics of obesity, can be a risk factor for thyroid cancer. Insulin regulates thyroid gene expression and stimulates thyrocyte proliferation, differentiation and transformation [10].
20
1.5 GENETIC STUDIES IN WTDC
Several genetic defects involved in the tumorigenesis of various thyroid tumors have been identified. The use of candidate gene sequencing, microarray expression analysis and whole-genome association studies have helped to determine the molecular alterations causing thyroid cancer. These enable clear classifications, precise prognosis, and targeted therapy.
1.5.1 Germiline mutations in WDTC
There is a strong evidence that the thyroid cancer is determined by the individual genetic background. In the last years many genetic linkage scans on thyroid cancer have been published, trying to determine this genetic contribution. Around 5% of WDTC shows familial aggregation and this could be explained by mutations in high-penetrance genes [41]. Hereditary factors seem to be implicated in some cases of PTC. In particular, mutations in the APC gene are associated with familial adenomatous polyposis, an autosomal dominant disease. A number of linkage studies, analyzing the distribution of markers such as microsatellites or SNPs in individuals with in diseased families, has reported putative susceptibility loci at 14q31, 19p13.2, 1q21, 2q21, 8p23.1-p22, 8q24 and 6q22 [42]. There is some evidence that loci 14q31, 19p13.2, 1q21, 2q21 are involved in the predisposition to familial WDTC, but no susceptibility genes have been discovered [43]. An evidence of linkage of MNG1 (multinodular goiter 1), on chromosome 14q31, was reported in a large Canadian family affected by PTC and a two generation family affected by goiter or FTC [44]. The TCO locus (thyroid tumors with cell oxyphilia on chromosome 19p32.2) was identified for the first time with a genome-wide linkage analysis performed on a French pedigree with familial thyroid cancer with cell oxyphilia. Then, several microsatellite markers have been frequently investigated to clarify the role of TCO locus in familial WDTC risk [45]
.
Similarly, the same studies concerning the analysis of microsatellites, suggested that fPTC/PRN locus (1q21) could predispose to this form of familial PTC associated with PRN (papillary renal neoplasia) [46]. Microsatellite markers were also genotyped in some families characterized by the presence of oxyphilia phenotype. The results reported an important role for a locus21
2q21 in familial WDTC susceptibility [47]. Identification of molecular markers, which segregate with the disease, could allow screening and treatment of patients at high risk before disease development. However, the results of these studies, concerning the genetic contribution to familial WDTC, have rarely been replicated and further analysis are needed to clarify the process of inheritance.
1.5.2 Sporadic mutations in WDTC
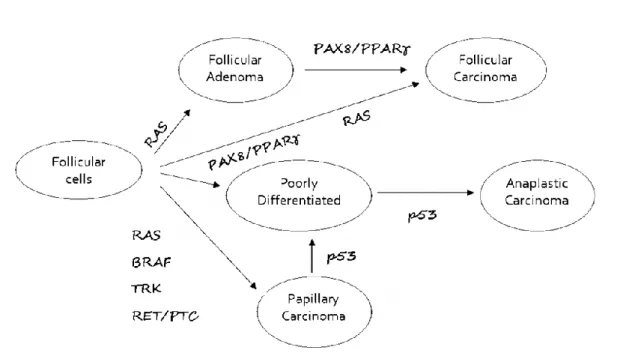
The common somatic alterations involved in WDTC are reported in Figure 9.The great majority of WDTC, around 95% cases, behaves as a sporadic entity.
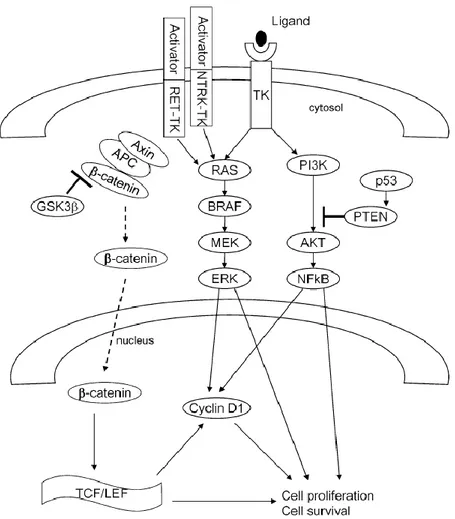
Somatic mutations discovered in the development of well-differentiated PTC include rearrangement of the tyrosine receptor kinases RET and TRK, and mutations of the intracellular signaling effectors B-type Raf kinase (BRAF) and RAS, causing activation of the Mitogen-activated Protein Kinase (MAPKK) and PI3K/AKT signaling pathways. Rearrangement of Paired box gene 8-Peroxisome Proliferator-Activated Receptor gamma (PAX8/PPARγ) and RAS mutations are frequent in well-differentiated FTC. These mutations have occasionally been identified in benign FTA. Also activation of PI3K/AKT pathway is
Figure 9 Genetic events involved in thyroid tumorigenesis. Mutation of BRAF and rearrangement of PAX8/PPARγ leading to PTC and FTC are mutually exclusive events.
22
involved in FTC pathogenesis. Other important genes associated with thyroid tumoroginesis are β-catenin (CTNNB1), TP53, IDH1 and Epidermal Growth Factor Receptor (EGFR).
Mutations of TP53 are involved in the ATC; this suggests that may have a role in the progression and aggressiveness of thyroid cancer.
In general, MAPK pathway is activated in PTC, instead PI3K/AKT pathway is activated in FTC; both the pathways are involved in aggressive thyroid cancer, such as metastatic recurrent cancers and ATC [49].Many other molecular alterations amplify and synergize their impacts on thyroid tumorigenesis [19].
Papillary Thyroid Carcinoma
PTC is the most common thyroid malignancy and, especially in the Western world, is increasing in frequency. This is due to several factors and it seems that benign thyroid diseases such Hashimoto´s thyroiditis, follicular, adenoma, and Graves´ disease are involved in an increased number of patients who present PTC. PTC etiologically originates as a radiation induced or as sporadic malignancy
[42]
. Radiation-related PTC is also variable in terms of the duration period of latency. It is considered that thyroid cancer requires an induction and latency period of at least 10 years exposure to ionizing radiation [50]. Many DNA damage types are induced by radiations; in particular double-strand DNA breaks are considered to be the most significant ones for chromosomal aberrations, mutagenesis, genetic instability and carcinogenesis. Many genetic lesions involved in PTC lead to the constitutive activation of the MAPK signaling pathway that has a fundamental role in the regulation of cell growth, proliferation, survival/apoptosis, and metabolic activities, through regulation of the expression of different genes Figure 10.More than 70% of PTCs present point mutations in RAS or BRAF genes and in 20-30% of cases there are chromosomal rearrangements of RET, especially RET/PTC. PTC is one of the rare human cancers of epithelial origin in which oncogenesis gene rearrangements play a noticeable role [51]. All the RET/PTC and TRK oncogenes are determined by chromosomal rearrangements juxtaposing the tyrosine kinase (TK) domain of the corresponding receptors to sequences of different genes [19].
23
BRAF
This gene encodes a protein belonging to the raf/mil family of serine/threonine protein kinases, which are intracellular effectors of the MAPK signaling cascade. BRAF mutation is the most common genetic alternation in thyroid cancer, occurring in about half of the sporadic PTCs in adults [52]. BRAF is a serine threonine kinase that is translocated to the cell membrane after being bound and activated by RAS, which results in the phosphorylation and activation of MAPK and other downstream targets of the MAPK signaling pathway [53]. One point mutation of BRAF is a thymine to adenine transversion at nucleotide 1799 (T1799A), leading to a substitution of valine to glutamic acid at residue 600 of the protein (V600E). This mutation determines the expression of BRAF-V600E mutant protein and
Figure 10 Genetic mutations involved in PTC tumorigenesis. Genetic alterations determine the activation of the mitogen-activated protein kinase (MAPK) signaling pathway. Those include RET/PTC and NTRK1 rearrangements and RAS and BRAF
24
causes constitutive activation of this serine/threonine kinase, leading stimulation of MAPK pathway, which results in oncogenic activation in the thyroid. BRAF-V600E mutation increases BRAF kinase activity by eliciting ERK1/2 phosphorylation. Subsequently phosphorylation of downstream MER1/2 and ERK1/2 leads to the expression of a number of specific genes involved in cell proliferation, differential, survival, and tumorigenesis [54]. This BRAF-V600E mutation occurs in 40-50% of cases, exclusively in PTC and papillary carcinoma-derived anaplastic cancer. This mutation has recently emerged, as a potential prognostic marker for PTC. Several studies have found this mutation to be associated with some clinicopathological characteristics [55]. It is associated with aggressive features such as extra thyroidal extension, lymph node metastases, advanced tumor stage, and radioactive iodine resistance. It is thought that the loss of responsiveness to I131 is due to loss of function of iodine metabolizing proteins such as NIS and TSHr. Tumor cells harboring this mutation have decreased NIS and TSHr gene expression compared to similar cells without the mutation [56].
Multifocal papillary thyroid carcinoma (mPTC) comprises about 20-30% of PTC. These encapsulated fvPTCs genetically demonstrate the presence of the BRAF-K601E (A1801G) mutation [57].
Another gene rearrangement in PTC is an inversion of chromosome 7q generating fusion between BRAF and AKAP9 (A-Kinase anchor protein gene 9) including BRAF domain without the N-terminal auto-inhibitory domain. In this way the fusion protein determines an elevate kinase activity. This kind of BRAF mutation has been discovered in radiation-induced thyroid carcinomas [58].
RAS
After BRAF mutations, RAS mutations are the second most common mutations in thyroid cancer and it occurs in 10-20% of all PTC. There are three isoforms of RAS (HRAS, KRAS,
NRAS) and they play an important role in the intracellular signaling. They encode a small G
protein located in the inner surface of the plasma membrane. In the inactive state they bind GDP; in the activate state they are bound to GTP. The intrinsic GTPase activity hydrolyzes GTP and converts RAS into an inactive GDP bound state, ending RAS signaling. Point
25
mutations alter its right function, switching in the active status and constitutively activating the downstream targets. They are associated exclusively with the fvPTC and not with the classical forms [59]. RAS can dually activate the MAPK (Ras, Raf, MEK, ERK) and the PI3K/AKT pathways; the latter pathway seems to be activated especially in thyroid tumors. The starting points of this pathway signaling are the various membrane growth factor receptors that present RTK, such as vascular epithelial growth factor receptor (VEGFR) and epidermal growth factor receptor (EGFR) [19]. The fact that RAS mutations occur also in FTA suggests that activated RAS has an important role in the beginning of the process. RAS mutation is necessary, with the presence of other mutations, to transform FTA into thyroid cancer [60].
RET/PTC
PTC is frequently associated with an RET rearrangement (40-70%), in which the tyrosine kinase domain of normally silent RET is fused with various constitutively expressed genes. RET is a proto-oncogene encoding for a cell membrane receptor tyrosine kinase. Structurally RET presents the typical protein kinase with a small N-lobe and a large C-lobe connected by a short linker. RET codes a membrane protein of the tyrosine kinase receptor family which is not expressed or expressed at very low levels in thyroid follicular cells. Its activation can be determined through chromosomal rearrangements involving the RET gene [61]. There are more than 10 types of RET/PTC translocation and the most common rearrangements are RET/PTC1 and RET/PTC3. Both of them are intrachromosomal paracentric inversions because they involve inversion of the long arm of chromosome 10, generating a fusion of part of RET intracellular domain coding region with the 5´end of heterologous genes. RET/PTC1 usually occurs in cPTC; tumors associated with RET/PTC3 are more common in solid-type PTC [62]. The rearrangements result in ligand-independent dimerization and constitutive tyrosine kinase function of RET, activacting the MAPK and PI3K/AKT pathways. There is an increasing body of evidence showing that the role of PI3K/AKT/mTOR pathway may be crucial for tumor development and may become an attractive target in the future [12]. RET/PTC lack the intracellular juxtamembrane domain which forms an integral part of the autoinhibited RET dimer interface; in this way the TK domain adopts the active conformation
26
[61]. Many studies show a higher prevalence of RET/PTC in PTC from children and young adults, it compares especially in PTC patients with a history of radiation exposure during childhood. This rearrangement is mutually exclusive with BRAF mutation in PTC but some studies have shown a coexistence of these mutations in PTC and ATC. This fact suggests that the two genetic alterations of the MAPK and PI3K/AKT pathways could have an important role in thyroid cancer aggressiveness [49].
TRK
TRK oncogenes derive from rearrangements of the NTRK1 gene on chromosome 1; their frequency does not exceed 12%. NTRK1 proto-oncogene rearrangements result in the formation of chimeric genes composed of the tyrosine kinase domain of NTRK1 fused to 5’ sequences of different genes (TPM3, MET and TRK-T2). It is estimated that NTRK1 proto-oncogene is activated by rearrangement with a similar frequency in “spontaneous” and radiation-associated thyroid tumors. Moreover, NTRK1 proto-oncogene activating rearrangements play a role in the development of a minority of radiation-associated PTC but not in adenomas [12]. This rearrangement demonstrates a worse prognosis compared to patients with RET rearrangement or without any alterations. This gene seems to be involved in the early process of thyroid carcinogenesis [19].
27
Follicular Thyroid Carcinoma
FTC is the second most common type of thyroid malignancy after PTC, and it comprises approximately 10–15% of all thyroid cancers in iodine-replete regions. FTCs are malignant epithelial tumors characterized by evidence of follicular cells differentiation; they can be distinguished in conventional or Hurthle-cell type with complete capsular or vascular invasion. FTC can be considered more aggressive compared with PTC [19]. There are many alterations, in common with PTC, involving MAPK signaling Figure 11.
The most common somatic mutations appear in NRAS, HRAS and KRAS; others occur in the elements of the RAF/MEK/MAPK and PI3K/AKT cell signaling pathways, determining the dysregulation of specific genes that promote thyroid proliferation and differentiation. The second most common mutation identified in FTC, in 30-40% of cases, is a chromosomal translocation which fuses a thyroid-specific transcription factor PAX8 to PPARγ, a nuclear hormone receptor important for the differentiation of several cells. Mutations of the RAS proto-oncogene are involved in up to 40% of follicular tumors. The presence of the RAS mutation does not differentiate FTC from FTA but is one important step in the transformation of follicular cells into carcinoma. In general, PAX8/PPARγ rearrangement and RAS mutation
Figure11 Molecular alterations in Follicular Thyroid Cancer. Alteration of the MAPK and the PI3K/Akt pathways in
FTC as a result of rearrangements involving PPARγ or deregulation of
28
are mutually exclusive. FTC and FTA are associated with Cowden syndrome characterized by mutations in the PTEN gene. PTEN mutation, identified in 6-12% of FTCs, decreases the right function of this gene, activating AKT and its downstream targets [59].
PAX8/PPARγ rearrangement
PAX8/PPARγ rearrangement is a result of the translocation that fuses the DNA binding domain of PAX8 to the peroxisome proliferator-activated receptor PPARγ. Peroxisome proliferator-activated receptors (PPARs) are members of the nuclear receptor superfamily, which form heterodimers with retinoid X receptor [63]. The heterodimers activate the transcription of specific genes in response to binding of a ligand. The PAX8/PPAR γ rearrangement generates an oncogenic paired box-8/peroxisome proliferator-activated receptor gamma fusion protein (PPFP) expressed under the control of PAX8 promoter. PPARγ is important in several biological pathways involving cell differentiation, insulin sensitivity, atherosclerosis and cancer. It has anti-neoplastic effects because it inhibits cell proliferation, inducing apoptosis and terminal differentiation with inhibition of angiogenesis. The fusion results in overexpression of PPARγ, and stimulates proliferation of normal human thyroid cell, in part due to loss of PPARγ actions. This rearrangement may be an early event in tumorgenesis [19]. Some studies have shown that the fusion protein exerts a dominant-negative effect on the wild-type tumour suppressor of PPARγ with consecutive anti apoptotic properties. Tumors with this rearrangement are present especially in solid growth pattern and in those with vascular invasion [59].
PIK3CA
The PIK3CA gene is mutated in 6-13% of FTC [59]. Amplification, genomic copy gain of
PIK3CA gene is an important oncogenic event. Genetic alterations in the PI3K/AKT are
especially common in FTCs and they promote the conversion of FTA to FTC determining tumour cells invasiveness. This pathway has, in fact, an important role in FTC [60]. It influences gene expression involving cell survival, proliferation, migration and tumour
29
progression. Follicular carcinomas show to have higher levels of AKT activation compared to normal tissue and papillary thyroid cancers.
PTEN
PTEN mutation has been identified in 6-12% of FTCs [59]. PTEN is a phosphatase that acts as a suppressor of PI3K/AKT pathway; it is a major human tumor suppressor and its genetic alterations have serious consequence. The loss of expression of PTEN can be determined by promoter methylation or deletion of the PTEN locus at 10q23. This modification involves the PI3K/AKT pathway in thyroid tumors, determining activation of AKT and its downstream targets [60].
1.5.3 SNPs in WDTC
Common genetic variants in low-penetrance genes may interact with each other and with the environment, regulating the thyroid cancer susceptibility [43,48].
Many association studies, both genome-wide and designed candidate gene approaches, have been published, in particular concerning the pathways involving DNA repair (XRCC1), cell-cycle control (TP53), detoxification (CYP1A1, GSTs) and thyroid function (TG) [42]. Some studies have evaluated possible associations between SNPs in the candidate DNA damage response genes (ATM, XRCC1, TP53, XRCC3, and MTF1), risk of radiation-induced and sporadic PTC. The best associated variants are those obtained from genome-wide association studies (GWASs) and confirmed both by replication studies and by functional assays. In particular FOXE1 is the best characterized locus predisposing the sporadic WDTC, since rs9665513 A allele has been recognized associated with an increased risk to develop the disease in a wide range of populations [64].
Two SNPs (rs116909374 and rs944289) within 14q13.3 were recognized in two different GWAS. Through computational analysis a large intergenic non-coding RNA gene, called Papillary Thyroid Carcinoma Susceptibility Candidate 3 (PTCSC3), located downstream rs944289 at 14q13.3, was discovered [65].The expression of this gene is down regulated in thyroid cancer tissues and its re-establishment inihibits cell growth, revealing its role as a
30
tumor-suppressor. Furthermore, the region 2q35 seems to contain common variants involved in WDTC. Strong associations were discovered for intronic SNP rs966423 in two independent GWAS. However, functional assays are necessary to validate the biological process concerning the associations in the 2q35 region [66].
31
AIM OF THE THESIS
The purpose of the thesis is to identify possible genetic single-nucleotide-polymorphisms (SNPs) involved in WDTC susceptibility, selected in genes somatically mutated in the disease. For the analysis of genetic SNP data we carried out a candidate-gene case-control study. A genetic case-control association study analyses the frequency of alleles or genotypes at genetic marker loci, considering people of a specific population, with and without a particular disease, in order to identify if there is a statistical association between the disease and the genetic alteration. Discovered associations with complex diseases could be used for clinical application, providing prognostic or strongly predictive information and possible pharmacological applications. In particular, this study consists of a gene and a SNP selection, genotyping and statistical association tests. After the identification of the candidate genes associated with the disease, further verification was done to analyze the functional action using in silico prediction tools.
32
MATERIALS AND METHODS
3.1 GENETIC ASSOCIATION STUDIES
We carried out a genetic association case-control study in candidate genes. The purpose was to compare the frequency of alleles and genotypes at genetic marker loci (SNPs) in individuals from an Italian population, with and without thyroid cancer, in order to determine if a statistical association exists between the disease and the genetic marker. We can define a genetic marker as a single biallelic locus with allele A and allele a. In the disease outcomes the risk factor for cases versus controls condition is the allele or genotype at a specific trait. The Odds Ratio (OR) is used to identify the association in the case-control studies; it represents the odds of a disease in exposed versus non-exposed individuals. The allelic OR describes the connection between the disease and the allele by analyzing the odds of the disease in an individual presenting allele A to the odds of the disease in an individual carrying allele a. The genotypic OR defines the association between the disease and the genotype considering the odds of the disease in persons carrying one genotype to the odds of the disease in persons carrying another genotype. The OR and its 95% Confidence Interval (CI) can be used to quantify association between an exposure and disease.
OR=1 Exposure does not affect odds of outcome
OR>1 Exposure associated with higher odds of outcome OR<1 Exposure associated with lower odds of outcome
The 95% CI is used to estimate the precision of the OR. A large CI indicates a low level of precision of the OR, whereas a small CI indicates a higher precision of the OR.
The first condition to consider during the observation is to assume that genotype distribution of the population is in Hardy Weinberg Equilibrium (HWE). We tested the genotype distribution for HWE proportion by using the chi squared test (χ2). Ors and 95% CIs were calculated unsing logistic regression. In this study the ORs were adjusted for age and gender using a macro, written using SAS (Version 9.2)
33
3.1.1 Population
The association study, a case-control study on WDTC, was established to verify the association between genetic polymorphisms and the risk to develop the disease. The cases and the controls came from all parts of the central and southern Italy. All patients were contacted during their routine follow-up by the Department of Endocrinology and Metabolism (University Hospital of Cisanello, Pisa). The initial diagnosis of WDTC may have been based on clinical suspection, but the final diagnosis was confirmed histologically or cytologically. The healthy controls were blood donors (University Hospital A. Meyer, Florence) and workers (mainly physicians, nurses and paramedical staff), of the same Hospital of Pisa, without
known thyroid disease. At the moment of blood collection both cases and controls were consulted in order to collect
some data: ethnicity, sex, age, height, body weight, birthplace and years of residence in the birthplace, place of residence, smoking habits, smoking history, eventual past exposures to IR and any positive family history of thyroid disease. The ethnicity of the cases and the controls is homogeneous as >99.9% of subjects are Caucasians (with Italian origin). According to the Helsinki declaration, the individuals signed an informed consent to participate in the study and to allow the genetic analyses on the biological samples.
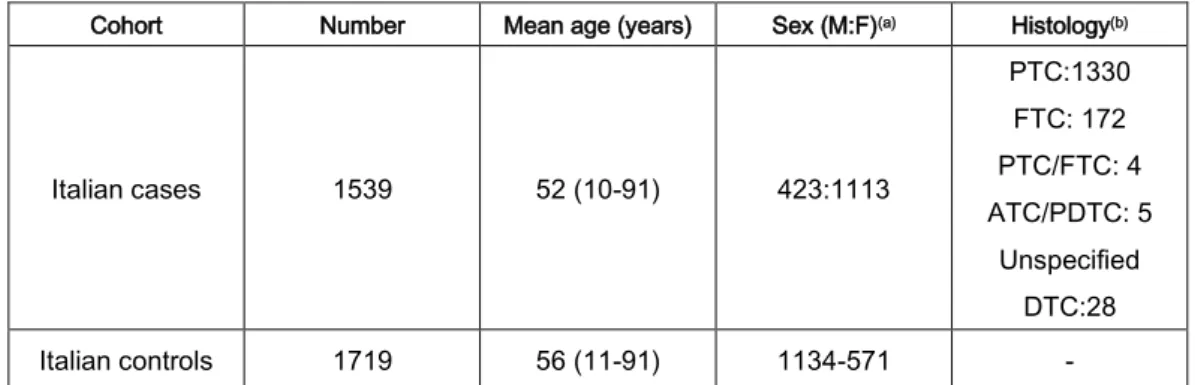
The case group considered in the present study consisted of 1558 WDTC patients, while the control group consisted of 1719 healthy individuals (640 blood donors and 1079 workers). The characteristics of the population used in this study are showed in Table 1.
Table 1 Characteristics of all the Italian cohort included in the study.
(a) M, male; F, female (b) ATC, anaplastic thyroid cancer; DTC; differentiated thyroid cancer; FTC, follicular thyroid cancer; PDTC, poorly differentiated thyroid cancer; PTC, papillary thyroid cancer.
Cohort Number Mean age (years) Sex (M:F)(a) Histology(b)
Italian cases 1539 52 (10-91) 423:1113 PTC:1330 FTC: 172 PTC/FTC: 4 ATC/PDTC: 5 Unspecified DTC:28 Italian controls 1719 56 (11-91) 1134-571 -
34
The genomic DNA was isolated from peripheral blood. The DNA samples from cases and controls were randomly placed on 96-well PCR plates.
We used the Biomek NX robot to prepare 384-well PCR plates, starting from four 96-well PCR plates. Negative controls (NTCs) and quality controls (QCs) were also included to verify the correct function of the analysis. In particular, negative controls are necessary to avoid false positive amplifications and quality controls represent duplicates to some samples, for the purpose of validate the assay´s accuracy and reproducibility.
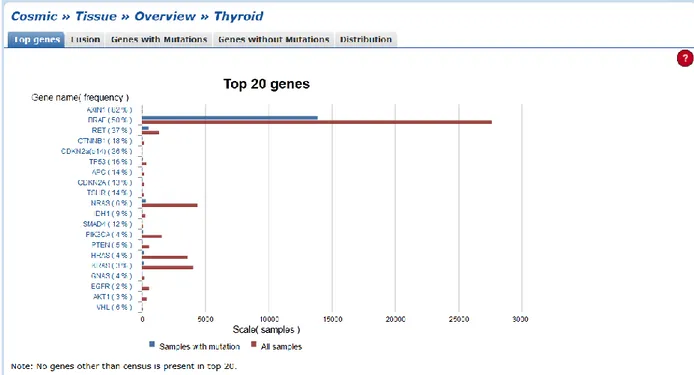
3.2 GENE AND SNP SELECTION
We used the browser Cosmic (http://cancer.sanger.ac.uk/cancergenome/projects/cosmic/) to select genes from the top genes mutated in thyroid cancer, especially considering those
involved in PTC (the most common thyroid cancer), obtaining a total of 20 genes Figure 12.
For each of these genes the SNPs selection was executed using the Ensembl Genome Browser (http://www.ensembl.org/index.html).
35
First, we considered all gene transcripts and we selected:
- 5´UTR variants: SNPs that are located in the 5 prime untranslated region (UTR). - 3´UTR variants: SNPs that are located in the 3 prime untranslated region (UTR). - Missense variants: SNPs that are located in protein coding regions and lead to an
amino acid change in the encoded protein sequence.
Among them, we further selected SNPs with global minor allele frequency (MAF) value over 10% and MAF over 5% in Italian population (TSI). We checked the linkage disequilibrium (LD) of the SNPs in the HapMap Project (http://hapmap.ncbi.nlm.nih.gov/) and in the 1000 Genomes Project (http://www.1000genomes.org/).
By selecting SNPs with pairwise LD r2 <0.8 we reduced the number of SNPs to genotype, choose SNPs in genetic sequences where there are no other polymorphisms that could influence the PCR amplification reaction.
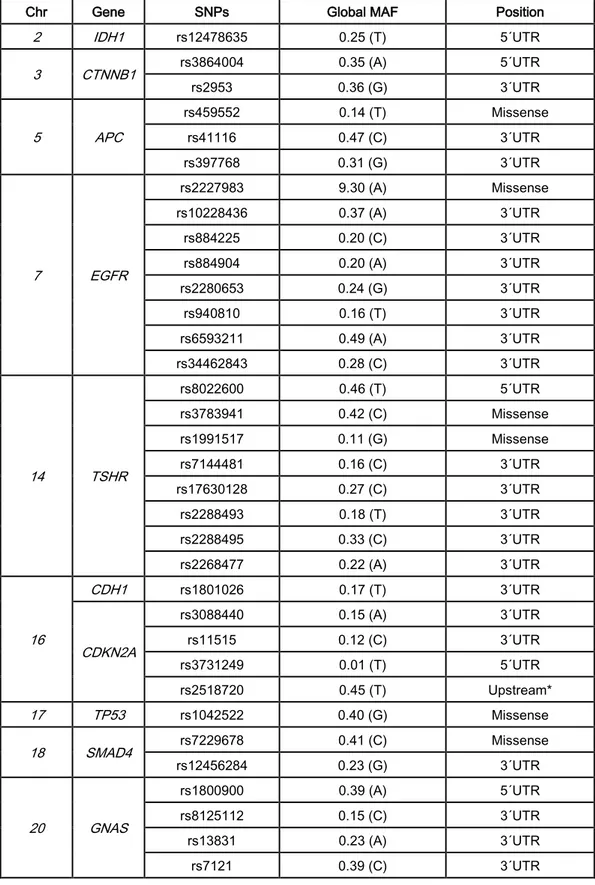
In this way we selected a total of 34 SNPs (5´UTR: 6, 3´UTR: 22 and missense: 6) located in 10 different genes Table 2.
36 .
Table 2 In the end 34 SNPs selected * r2=0.93, D´=1.0 with rs3814960 located in 5´UTR
Chr Gene SNPs Global MAF Position
2 IDH1 rs12478635 0.25 (T) 5´UTR 3 CTNNB1 rs3864004 0.35 (A) 5´UTR rs2953 0.36 (G) 3´UTR 5 APC rs459552 0.14 (T) Missense rs41116 0.47 (C) 3´UTR rs397768 0.31 (G) 3´UTR 7 EGFR rs2227983 9.30 (A) Missense rs10228436 0.37 (A) 3´UTR rs884225 0.20 (C) 3´UTR rs884904 0.20 (A) 3´UTR rs2280653 0.24 (G) 3´UTR rs940810 0.16 (T) 3´UTR rs6593211 0.49 (A) 3´UTR rs34462843 0.28 (C) 3´UTR 14 TSHR rs8022600 0.46 (T) 5´UTR rs3783941 0.42 (C) Missense rs1991517 0.11 (G) Missense rs7144481 0.16 (C) 3´UTR rs17630128 0.27 (C) 3´UTR rs2288493 0.18 (T) 3´UTR rs2288495 0.33 (C) 3´UTR rs2268477 0.22 (A) 3´UTR 16 CDH1 rs1801026 0.17 (T) 3´UTR CDKN2A rs3088440 0.15 (A) 3´UTR rs11515 0.12 (C) 3´UTR rs3731249 0.01 (T) 5´UTR rs2518720 0.45 (T) Upstream* 17 TP53 rs1042522 0.40 (G) Missense 18 SMAD4 rs7229678 0.41 (C) Missense rs12456284 0.23 (G) 3´UTR 20 GNAS rs1800900 0.39 (A) 5´UTR rs8125112 0.15 (C) 3´UTR rs13831 0.23 (A) 3´UTR rs7121 0.39 (C) 3´UTR
37
3.4 METHODS USED FOR THE POLYMORPHISM ANALYSIS
Thanks the recent developments in molecular genetics there are several techniques that allow identification of known mutations on the DNA directly by examining the differences in the nucleotide sequence. In particular for this thesis work we used specific techniques to recognize DNA changes:
- TaqMan Real-Time PCR
- KASPar SNP Genotyping System (for the SNP rs2518720 in the CDK2A gene).
3.5 THE POLYMERASE CHAIN REACTION (PCR)
The PCR is a relatively inexpensive and simple tool that can be used to focus on a DNA segment and copy it billions of times. This reaction is a method to analyze a short sequence of DNA (or RNA) even in samples containing only minimal quantities of genetic material. It amplifies selected sections of DNA or RNA. With one cycle, a single segment of double-stranded DNA template is denatured into two separate single-double-stranded DNA molecules; these two pieces are then available for amplification in the next cycle. Repeating these cycles, more and more copies are generated and the number of copies of the template is increased exponentially.
The PCR reaction requires the following components:
- DNA template: The sample DNA that contains the target sequence. At the beginning
of the reaction, the high temperature denatures the original double-stranded DNA molecule.
- DNA polymerase: A type of enzyme that synthesizes new strands of DNA
complementary to the target sequence. Taq DNA polymerase is the DNA polymerase that is most often used in PCR, it comes from a strain of bacteria called Thermus aquaticus that lives in the hot springs of Yellowstone National Park. It is heat resistant, in fact it can survive near boiling temperatures and works quite well at 72 ° C.
38
- Primers: Oligonucleotides, typically 15-30 bases long, hybridize to opposite strands
and flank the target DNA for amplification. In the PCR primer selection, it is important that they do not contain bases complementary to themselves or with each other. Complementarity at the 3'ends should especially be avoided to minimize the formation of an artifact product, often called "primer-dimer" or "primer-oligomer". Their specificity is also important because the high concentration of primers may promote mispriming and the accumulation of non-specific products, on the other hand, a low concentration may not allow for the completion of all cycles established with a consecutive decrease of the desired final product.
- Nucleotides (dATP, dTTP, dCTP, dGTP): Single units of the bases A, T, C, and G
which are necessary for the new DNA strands. For a good efficiency of the PCR the four nucleotides must be present in equimolar concentrations. On the one hand too high concentration may increase the rate of wrong incorporation and, on the other hand too low concentration may damage the efficiency of the reaction.
- Reaction buffer: The buffer, based on Tris-HCl and KCl, serves to reproduce the
optimal conditions of the DNA polymerase activity and to increase its processivity, the number of nucleotides that the enzyme is able to insert in the new strands before detaching from template strand.
- Magnesium chloride (MgCl2): It is an essential element for the activity of the DNA
polymerase because its binding with the enzyme stabilizes the enzyme in a three dimensional conformation, promoting its activity. A high concentration of MgCl2 increases the yield but decreases the reaction specificity because it reduces the stringency of the primer hybridization; a low concentration increases the stringency of the primer hybridization making the base-paring more specific, but decreasing the PCR products.
PCR reaction starts with the denaturation step. Two primers are designed to match the DNA region to be amplified. Through complementary base-pairing, one primer attaches to the top strand at one end of the target sequence, and the other primer attaches to the bottom strand at the other end. Primers are essential for the DNA polymerase activity because it can generate new DNA strands by just adding new bases into an existing piece of DNA. A
39
mixture of four types of nucleotides (A, C, G, T) is used for the PCR reaction. Nucleotides are the building blocks that DNA molecules are made of. DNA polymerase attaches itself near the end of the primer and starts adding nucleotides. Samples are heated to 94-96 ºC, for one to several minutes, to denature the DNA template. Later the temperature is lowered to 50-65 ºC; this allows the left and right primers to anneal to their complementary sequences. When the temperature is raised to 72 ºC the Taq polymerase can attach at each priming site and synthesize a new complementary DNA strand. These three steps are repeated for 40 cycles obtaining several DNA copies of the DNA template.
1. Denaturation: At 94 ºC the double-stranded DNA melts and opens into two pieces of single-stranded DNA.
2. Annealing: At medium temperatures, around 54 ºC, the primers anneal with the single-stranded DNA template.
3. Extension: At 72 ºC, the optimal temperature for polymerase activity. The polymerase attaches on the joined primer and template and starts copying the DNA target. DNA building blocks complementary to the template are coupled to the primer, making a double stranded DNA molecule.
40
3.5.1 TaqMan PCR
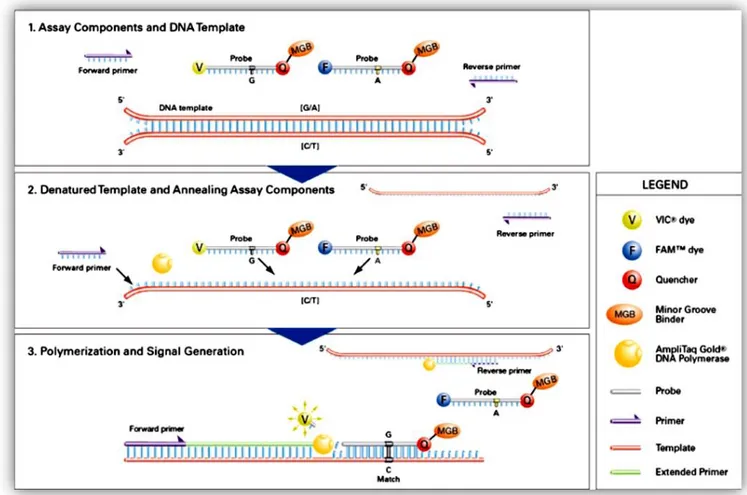
One particular type of PCR is the TaqMan PCR. The DNA region including the SNP is amplified in the presence of two allele-specific fluorescent probes; in this way more specificity can be determined by their hybridization because each fluorescent probe is specific for one allele of the DNA template. The TaqMan SNP genotyping assay is called the 5´nuclease allelic discrimination assay because it utilizes the 5´nuclease activity of the DNA polymerase to hydrolyze the probe bound to its target amplicon. It requires forward and reverse PCR primers, necessary to amplify the polymorphic sequence of interest, and two different TaqMan minor groove binder (MGB) probes that attach to the minor groove of the DNA helix, stabilizing the probe/template complex. TaqMan probes are single-stranded DNA oligos that contain a reporter dye linked to the 5´end of the probe and a fluorescent quencher at the 3´end of the probe. One probe is marked with FAM dye (6-carboxyfluorescein) and detects the Allele 1 sequence; the second probe is marked with VIC dye (4,7,2′-trichloro-7′-phenyl-6-carboxyfluorescein) which detects the Allele 2 sequence. When the probe is intact, the proximity of the reporter dye to the quencher does not give the possibility to emit fluorescence. During PCR, the TaqMan probe anneals specifically to a complementary sequence between the forward and reverse primer sites; the 5´nuclease activity of AmpliTaq Gold® DNA Polymerase (Applied Biosystem) cleaves only those probes that are hybridized to the complementary target. In this way the reporter dye and the quencher dye are separated, increasing fluorescence of the reporter Figure 13.
41
The reaction produces fluorescence spectra with several peaks that can be measured only with specific instruments equipped with a spectrograph on the emission side and supported with a powerful software to analyze the spectra.
The increase in fluorescence signal is detected only if the target sequence is complementary to the probe and is amplified during PCR. Because probes are included in the PCR, genotypes are defined without any post-PCR processing. When the fluorescence signal is not quenched, it can be detected with laser excitation.An increase in either FAM or VIC dye fluorescence indicates homozygosity for specific alleles and an increasing fluorescence of both dyes indicates heterozygosity Figure 14.
Figure 13 Each probe is specific for one allele and is linked with different fluorescent dye (VIC, FAM) at the 5´end. Both probes have the same quencher at the 3´end. When annealed to the target
sequence, the probe will be degraded by the DNA polymerase’s 5´nuclease ability during the extension step of the PCR. Probe degradation allows for separation of the reporter from the quencher
42
TaqMan Protocol
To identify the best conditions of amplification we tested all the 34 assays using one of our sample plate; when satisfied genotype clusters were obtained we extended the genotyping to all the other Italian sample plates, using one of the following protocols in order to obtain optimal clusters of the fluorescence signals during the plate reading Table 3, 4, 5.
If the clusters were too close to each other we tried the PCR amplification with two different Assay Mix volumes (12/24µl) or with two different Master Mixes as HOTFIREPol and QUIagen Mastermix Figure 15.
a b c Figure 14
The different visible clusters refer to genotype condition: homozygotes for either Allele 1 (blue dots) or 2 (red dots)
and heterozygosites for both alleles (green dots) derived.
Figure 15 Master Mix conditions:
a (HOTFIREPol 12µl) and b (HOTFIREPol 24µl) genotype clusters do not separate from each others; c (QUIagen Mastermix 24µl) the separate clusters corresponding to the three possible genotypes.
43
Mix Composition:
- HOT FIREPol DNA Polymerase - 5x Probe qPCR buffer
- 15 mM MgCl2
- dNTPs including dTTP to improve reaction sensitivity and efficiency compared to dUTP
- ROX dye: it is an internal passive reference dye used to normalize the fluorescent reporter signal generated in qPCR.
Cycling conditions in HydroProgram HOTFIREPol:
1. Initial denaturation 95 ºC, 15 minutes2. Denaturation 95 ºC, 15-20 seconds 3. Annealing 60 ºC, 60 seconds
Repeat steps 2-3 39 times (a total of 40 cycles).
Further cycling and reading can be performed until tight genotyping clusters have been obtained (recycling conditions).
Recycling conditions:
1. 95 ºC 20 seconds 2. 60 ºC 60 secondsRepeat steps 1-2 twice (a total of 3 cycles) PCR reaction mix volumes 384-well plate 384-well plate 5x Reaction mix 400µl 400µl 40x Assay mix 12µl 24µl H2O 1588µl 1576µl Final volume 2000µl 2000µl
44
Cycling conditions in HydroProgram QIA40:
1. Initial denaturation 95 ºC, 15 minutes 2. Denaturation 95 ºC, 20 seconds 3. Annealing 60 ºC, 30 seconds
Repeat steps 2-3 39 times (a total of 40 cycles)
.
Recycling conditions:
1. 95 ºC 20 seconds 2. 60 ºC 60 secondsRepeat steps 1-2 twice (a total of 3 cycles). PCR reaction mix volumes 384-well plate 5x Reaction mix 900µl Assay mix 24µl H2O 900µl Final Volume 2000µl