Endoscopic Non Rib Spreading Video Guided Approach To Mitral Valve Surgery Short and Medium Term Results
A Thesis Presented to
The Division of Life Sciences Scuola Superiore Sant’Anna
In Partial Fulfillment
of the Requirements for the Degree
Second Level Master In Innovation In Cardiac Surgery: Advances In Minimally Invasive Therapeutics - 4th Edition.
Rafik Margaryan MD, PhD
Approved for the Division ()
Acknowledgements
I would like to thank all the surgeons from the adult cardiac surgery department of Ospedale Del Cuore in Massa, who helped me with this thesis. An especially I would like to take the opportunity and thank head of the same department Dr Marco Solinas for his support, continuous teaching and belief in myself.
Preface
Endoscopic mitral valve surgery is the ultimate level of minimally invasive cardiac interventions. It seems that this exact approach is the way for this particular single valve disease. It provides very effective and sufficient visualization if the valve itself, results are more are comparable to any kind of mitral valve surgery and patients recover much rapidly. It has leaning curve as any other new technique in cardiac surgery, but it is not steep and we believe that it is enough about 50 cases in order to pass it.
Table of Contents
Objective . . . xi
Material and Methods . . . xi
Results . . . xi
Conclusion . . . xii
Introduction . . . . 1
Materials And Methods . . . . 5
Patients’ Population . . . 5
Endoscopic Mitral Valve Procedure . . . 6
Mitral valve repair . . . 8
Statistical analysis . . . 9
Results . . . 11
Patients Characteristics . . . 11
Immediate and Short Terms Results . . . 12
Follow Up . . . 13
Discussion . . . 15
Study Limitations . . . 17
Figures . . . 25 Conclusion . . . 29 References . . . 31
List of Tables
1 Summary data for demographic variables . . . 20
2 Mitral Repair Complexity variables. . . 21
3 Mitral procedure detals by its complexity . . . 22
List of Figures
1 Increase of puplications using ‘minimally invasive mitral surgery’ search on pubmed. . . 3 2 Field prepered before incision. . . 6 3 Field with completed preparation. . . 8 4 Cardiopolmonary bypass time differences in defferent intercistal space
approach. . . 26 5 Cardiopolmonary bypass time differences in defferent intercistal space
approach. . . 27 6 Kaplan-Meier survival curve for main cohort. . . 28
Abstract
Objective
Our aim of this thesis was to analyse experience of endoscopic mitral valve surgery in Ospedale Del Cuore in Massa and to determine its non inferiority relative to other minimally invasive mitral valve approaches (inside the same institution).
Material and Methods
312 consecutively operated patients from 2015 to 2019 underwent totally endoscopic mitral valve surgery via limited 3-4 cm right thoracotomy and without costal retractor. All patients had preoperative chest x-ray (antero-posterior and lateral), echocardiogra-phy with quantitative measurments, flow dopplerograechocardiogra-phy for insufiecency estimation. All patients over 40 years old underwent coronarography, only selected patients had computed tomography scan.
Results
Mean age of 62.2 ± 11.8 years old. 97 (31.5%) of the patients were female, mean BMI was 24.7 ± 3.6. Valvular diseases were prevalent degenerative diseases 287 (92%). In men 200 (64.1%) patients a peri-areolar cut was performed. In female, a sub-mammary groove minithoracotomy of about 4 cm (n = 92 (94.8%)) was performed. The average
duration of extra-corporeal circulation was 144.8 ± 30.7 minutes. The aortic clamping on average was 92.3 ± 22.9 minutes. The average mechanical ventilation time was 6.3 ± 3.7 hours. The duration of stay in intensive care units was 1.2 ± 0.7 days.
Conclusion
Endoscopic mitral valve surgery is safe, reproducible and has results excellent potential to become standard of care. It is comparable with minimally invasive mitral valve standard procedures. CPB times and aortic clamping are part of the learning curve but did not affect the mortality or affect premature mortality.
Dedication
Introduction
The minimally invasive mitral valve surgery have become a standard choice for operating strategy in many centers(Glauber et al., 2015; Walcot et al., 2015); it does not refer to a single one but to a collection of new techniques and technologies specific to cardiac surgery(Borger et al., 2014; Poffo, Montanhesi, Toschi, Pope, & Mokross, 2018). Contemporary advances in cardiopulmonary perfusion, intracardiac visualization, robotic instrumentation and manipulation favored development in surgical technique, with more and more surgeons adopting minimally invasive valve surgery in their practice (see Figure 1).
Early data suggest that these operations are safe and effective and provide com-parable results to those obtained with conventional operations. To achieve these goals, surgeons have adopted an evolutionary implementation model. There are also favorable results for long term follow up versus conventional approach(Mkalaluh et al., 2018). Conventional minithoracotomic approaches have been modified and arrived quickly to micro incisions and the “port access” .
Then assisted video techniques are getting more popularity. Robotic mitral valve surgery in the north america is very popular(Cao, Harris, Croce, & Cao, 2017; Chit-wood, 2016). In order to decrease postoperative discomfort and hospitalization and return of patients to normal lifestyle quickly, 3-4 cm video-assisted techniques and incisions for almost all cases of isolated mitral disease were used. With these techniques both the replacement and repair of the mitral valve can be performed; however other
2
types of interventions also could be performed, like mixoma resection(Bianchi et al., 2019).
Minimally invasive surgery is applicable, especially to younger women who want surgery that leaves a much more cosmetic non visible scar. A quite safe and well established way to approach the mitral valve without aortic clamping is via hypothermic induced fibrillation, for example in case of intervention with bypass when re-sternotomy is hazardous. The related contraindications relate to previous pleural adherence / inflammation, severe pulmonary hypertension, severe posterior annular calcification, a calcific ascending or highly atherosclerotic aorta.
The video-assisted mitral valve surgery includes the combined advantages of a 3-4cm minitoracotomy, direct aortic clamping, telescopic video assistance, venous return assisted with negative pressure, and conventional surgical instruments for the minimally invasive surgery. Peripheral arterial perfusion was initially selected due to the need to have a better exposure to the surgical site. Central arterial cannulation is practicable in direct vision mitral valve surgery, in endoscopic, video-assisted cases it is convenient to use peripheric cannulation. At the Ospedale Del Cuore of ‘G Monasterio’ Foundation in recent years they has been treated with a minimally invasive approach, over 3,000 patients single valve disease cases. The aim of our study was to evaluate the technical feasibility of the endoscopic approach (beginning of July 2015), not inferiority to standard conventional minimally invasive surgery, and short and medium term results.
3 0 50 100 1990 2000 2010 2020 Year of Publications Publications' Count Source: www.Pubmed.com
Figure 1: Increase of puplications using ‘minimally invasive mitral surgery’ search on pubmed.
Materials And Methods
Patients’ Population
312 consecutively operated patients from 2015 to 2019 underwent totally endoscopic mitral valve surgery via limited 3-4 cm right thoracotomy and without costal retractor. All patients had preoperative chest x-ray (antero-posterior and lateral), echocardiogra-phy with quantitative measurements, flow dopplerograechocardiogra-phy for insufficiency estimation. All patients over 40 years old underwent coronarography, only selected patients had computed tomography scan. For demographic data see Table 1. Intercostal space approach was decided upon radiography analysis by experienced cardiac surgeon. All intervention where performed by senior cardiac surgeon. All clinical data was collected prospectively. All mitral patients were forwarded to endoscopic surgery and had different levels of complexity:
1. Simple if there were involved two procedures on the mitral valve itself (ex. annu-loplasty and one/two pair of neochordae positioning) or any other combination of two surgical repair gestures (resection, sliding, commisural closure, Alfieri stitch, etc).
2. Complex procedures where we preformed three or more surgical gestures during single mitral valve repair operation.
3. All mitral valve replacement cases were considered as a complex mitral valve procedure in endoscopic settings. For complexity see Table 2.
6
Endoscopic Mitral Valve Procedure
Under general anesthesia, patients were intubated using a single lumen endotracheal cannula for pulmonary ventilation. Disposable paddles for external cardiac defibrilla-tion were placed in the right scapula and anterolateral region of the left hemi-thorax. A two- or three-dimensional transducer for intraoperative trans esophageal electrocar-diography (TEE) was placed. Before the positioning the patient, the right hemi-thorax was carefully examined, and significant pre-existing asymmetries or chest deformities were recognized: that might predict complicated access via periareolar access. Af-ter patients have been positioned whit the right hemi-thorax about 15-20 degrees, marking the reference intercostal spaces and lines were cared out in order to facilitate the anatomical references when sterile field is completed (we do use sterile elastic field membrane). A right angle skin incision was performed inside the edge of the nipple-areolar complex, on its lower half circumference (hours position of 4 to 10, clockwise). In female patients we prefer to do skin incision in the inframmamary line as wide as periareolar incision (3-4 cm, see Figure 2).
Figure 2: Field prepered before incision.
Subcutaneous tissues was then sectioned with dietary through the entire length of the incision, reaching the major pectoral musculus the underlying intercostal space.
7
Later hemostasis was performed accurately. Soft tissue retractor was used providing 360 degree atraumatic circumferential retraction and allowing maximum exposure with minimum incision size. No rib retractor was used in this approach. A 10.5 (some cases 12.5) mm trocar was then inserted in the same intercostal space as the incision on the mid-axillary line ; and two intercostal spaced lower (5th or 6th intercostal spaces) in the anterior axillary line. Femoral vessels were isolated. Systematic heparinization was achieved (HMS or simple ACT guided). At that point the femoral vessels were cannulated using Seldinger technique under direct vision. Venous cannula (Biomedicus 25 F) were placed in the right atrium using trans-esophageal echocardiography. In the case of suspected insufficient single cannula venous drainage a second cannula was placed into the jugular vain (16 F). Seldinger technique was used also for femoral arterial cannulation with Biomedicus 15-21 F cannulas depending on the weight. Cardio-pulmonary bypass was established and the patients were cooled to 34oC.
After pump is started the mechanical ventilation was suspended. A pledgeted 4/0 polypropylene purse-string suture for cardioplegia and aortic venting was placed on the ascending aorta. Through the 2nd intercostal space in the anterior axillary line the Chitwood trans-thoracic clamp was introduced (Fehling Instruments, Karlstein, Germany). Under the video guidance the ascending aorta was clamped and cold crystalloid cardioplegic solution Custodiol HTK (Kohler Chemie GmbH, Bensheim, Germany) was administrated. The surgical instruments used were not specific for endoscopic mitral valve surgery; they are the routine minimally invasive surgery instruments. Under the videoscopy the pericardium was opened 2-3 cm above the phrenic nerve. The pericardium was retracted with three polypropylene 3/0 and three polyester 2/0 suture (above and under, respectively). The inferior retraction suture were extemporized using two ports and entrance for Chitwood clamp. With the aim of air embolism prevention CO2 insufflation was maintained during central part of the
8
Figure 3: Field with completed preparation.
Mitral valve repair
The left atrium was opened anteriorly to the right pulmonary veins and retracted using a trans-thoracic retractor (Estech, San Ramon, CA, USA or USB retractor, Belgium) positioned through the same intercostal space as the thoracotomy medially or laterally to right internal mammary artery. The mitral valve was inspected and then repaired or replaced. In the mitral valve repair the following techniques were used:
1. annuloplasty 2. leaflet resection 3. chordal implantation
4. commisural or any other leaflet closure 5. Alfiery technique
The valve competence was tested with cold saline solution after the repair was complete. In case of the mitral valve replacement mechanical or tissue valves were used. Additionally, when necessary tricuspid valve annuloplasty was carried out. In some patients atrial fibrillation the box lesion was created using Cobra System before the left atrial opening. After the procedure the atriotomy was closed with
9
3/0 polypropylene running suture and a ventricle vent was positioned through the atriotomy. Aim of the study was to develop an algorithm that could predict the intercostal space with highest accuracy possible. We have developed the machine learning algorithm using clinical data and some simple radiography measurements; and a deep learning algorithm that could only use the chest radiography for intercostal space prediction.
Statistical analysis
Clinical data was collected in prospective fashion. Continuous variables where pre-sented as mean and standard deviation and compared using non parametric and parametric test (Wilcos test, Student’s test, respective). Categorical variables where presented as percentage compared with Fisher’s exact test or ‰2 test. Algorithm bases
on clinical data was created using random forest tree classification algorithm. All the analysis were performed using R, Python programming languages using reproducible research rules.
Results
Patients Characteristics
A total of 312 patients with mean age of 62.2 ± 11.8 underwent mitral valve repair / replacement interventions in totally endoscopy setup. 97 (31.5%) of the patients were female, mean BMI was 24.7 ± 3.6 (see Table 1). Valvular diseases were prevalent degenerative diseases(287 (92%)) . 15 (8.72%) patients with prolapse of the anterior leaflet, 121 (70.3%) patients with prolapse of the posterior leaflet and 33 (19.2%) with prolapse of both leaflets. The NYHA class preoperative average was 1.0 ± 0.6. The EuroSCORE II preoperative mean was 1.1 ± 0.9, while Logistic Euroscore was relatively higher 5.1 ± 4.7 (compared EuroSCORE II, p <0.01), STS average score was 0.72 ± 0.37 and ACEF average score was 1.4 ± 1.4 (see Table 1). In men 200 (64.1%) patients a peri-areolar cut was performed, 200 (64.1%). In female, a
sub-mammary groove minithoracotomy of about 4 cm (n = 92 (94.8%)) was performed. In 3 (0.962%) patients were converted initial incision into complete sternotomy due to tense pleural pericardial adherence was necessary. In 14 (4.49%) patients, converting initial endoscopic incision in conventional minithoracotomy due to visualization problems and the inability to continue the operation in video-guided mode, was necessary. In 284 (91%) patients Crystalline caldioplegia were infused (Custodiol HTK, Dr Franz Köhler Chemie GmbH, Bensheim, Germany), in the remaining Calafiore modified cardioplegia (28 (8.97%)).
12
In 182 (58.3%) patients Gore-Tex 4/0 neo-chordae were implanted (W. L. Gore and Associates, USA). In 28 (8.97%) patients posterior leaflet resection was carried out; in 60 (19.2%) patients, indentation closure technique was used, and in 8 (2.56%) patients posterior leaflet resection with a sliding was performed. In 15 (4.81%) patients Carpantier-Edwards Physio II were implanted (mean diameter 28.5 ± 1.6; in 4 (1.28%) LivaNova Memo 3D (mean diameter is 33.3 ± 3.1); in 79 (25.3%) Medtronic Future Band (average diameter is 31.4 ± 2.7); in 4 (1.28%) Medtronic Future Ring (mean diameter is 31.5 ± 1.9, and in 76 (24.4%) Medtronic Simulus (mean diameter is 31.3 ± 3.1see Table 3). 35 (11.2%) patients underwent mitral valve replacement in main cohort(see 1). Repair rate in degenerative disease alone was 272 (94.8%). In 275 (88.1%), the Cor-Knot device (LSI Solutions, New York, USA) for rapid suturing in limited space. The average duration of extra-corporeal circulation of 144.8 ± 30.7 minutes was. The aortic clamping on average 92.3 ± 22.9 minutes lasted. The average mechanical ventilation time 6.3 ± 3.7 hours was. The duration of stay in intensive care units 1.2 ± 0.7 days was .
Immediate and Short Terms Results
A revision of the surgical wound for bleeding in 5 (1.6%) patient was required. The source of bleeding was the trocar insertion site (see Table 4). One patient underwent a replacement of the mechanical mitral valve for early thrombosis. 17 (5%) patient were transfused. There was no case of transient or permanent neurological dysfunction, low cardiovascular syndrome or intra-aortic balloon pumping; no acute renal failure, no pulmonary dysfunction in any patient was observed. Respiratory complications (pleural effusion, pneumothorax, subcutaneous emphysema, non invasive ventilation for more than 48 hours) in this case were infrequent (8 patients, 2.6%). The analysis of complications are reported in Table 4. Overall postoperative hospital stay was 7.5
13
± 3.5 days. No intraoperative and 30-day mortality in this patient was observed. A residual none, trivial or mild grade mitral regurgitation was in 299 patients (96.1%) was observed. No patient had moderate or severe IM impairment (3 + / 4 +) at the time of discharge.
Follow Up
The mean follow-up of 7.0 ± 6.0 months. We have full follow-up completed for 30 days up to 100%, 3 months 90.1% and more than one year 30.6% patients. The mean NYHA class at follow up was 1.4 ± 0.5 and statistically lower than preoperative (p <0.01). The echocardiographic follow-up monitoring no mitral regurgitation was observed in 259 (83.2%) , mild regurgitating (1 +) in 17 (5.7%) , moderate and/or above (Ø 3+) in 27 patients. In a subpopulation by removing first 50 cases (due to learning curve) we have drastic drop of moderate and/or above percentage (around 4 %). No case of endocarditis or thromboembolic events has been observed. Patient satisfaction with the SF12 questionnaire was higher in postoperative than preoperative (highest physical score and Mental score). Late mortality was not observed in any patient. When excluding leaning curve the patients discharge with over moderate to severe insufficiency was significantly dropped (p < 0.05).
Discussion
Our results underline the efficacy, reproducibility and feasibility of endoscopic mitral valve surgery in totally endoscopic approach. This technique seems to deliver superior short and midterm results. Owing to the anatomical position of the mitral valve, a right lateral approach (periareolare, sub-mammary or axillary) provides excellent visualization, even if operative space is limited. In our study population, endoscopic mitral valve approach provided very satisfactory early functional results in both groups which remained stable at 3-month and 1-year follow-up.
We found low rates of MACE for this subgroup of patients. We found comparable oper-ation times and hospitalizoper-ation times like reported previous our publicoper-ations(Glauber et al., 2015). Shorter operation times in the 3D endoscopy is likely to be attributed to a better orientation of the surgeons, more importantly, we think that endoscopic visualization and guidance, and especially 3D endoscopy, is a helpful tool creating a detailed overview, allowing improved depth perception (see Figure 4). Having a 3D view of the operation field, mitral valve inspection and repair is more simple and intuitive, and thus faster. Especially for cases of complex mitral valve reconstruction, it facilitates a superior orientation and allows perfect placement of artificial neochordae. We found 3D endoscopy-guided mitral valve surgery associated with a very fast learn-ing curve. Concerns about more distinct learnlearn-ing curves with evolution of minimally invasive techniques making the procedure technically more challenging could not be confirmed in our study. Fast recovery due to low complication rates, avoidance of
16
sternotomy, short operation times and early mobilization due to less pain lead to shorter hospitalization in this cohort. The analysis of patient questionnaires and interviews showed a great patient satisfaction regarding postoperative pain and early mobilization, as well as the cosmetic result, for men and for women. Patients from this cohort had a significantly less analgesics consumption and lower pain-scale values. Several meta-analyses already compared studies using either conventional sternotomy or a minimally invasive access for mitral valve surgery regarding procedure-related outcomes(Daemen, Heuts, Olsthoorn, Maessen, & Sardari Nia, 2018).
Consistently, these publications found reduced length of ICU stay and reduced total time of hospitalization, shorter respirator dependence, less complications and less postoperative pain (Cheng et al., 2011; Svensson et al., 2010). Most studies showed equivalent or longer times for operation, cardiopulmonary bypass and aortic cross-clamp without a negative effect on outcome (Cheng et al., 2011; Modi, Hassan, & Chitwood, 2008). However, criticism remains since some studies showed higher incidence of neurological events, aortic dissection and groin complications, longer learning curves attributed to technically more difficult procedures due to limited space and the need for conversion to mitral valve replacement instead of MVR (Vollroth et al., 2013). The first two problems are rather influenced by clamping and cannulation techniques. We did not see any neurological complications or aortic dissection in our study collective. And we think that groin complications can be prevented by per-cutaneous cannulation. We recently changed our cannulation strategy to a completely per-cutaneous access and did not see any more groin complications so far. We think that 3D endoscopic exposition is an interesting and intuitive tool to assist the surgeon by creating increased depth perception and better overview. It enables exact reconstruction in all dimensions allowing even complex repairs. Improved visualization does not only simplify complex repairs but also enables fast learning curves and shorter operative times.
17
In our study, we can report of excellent results, with regard to perioperative data, complications and early as well as mid-term repair results using only a soft-tissue retractor with no RS. Furthermore, we can report of high patient satisfaction being able to return to daily life early and without major complications with pleasing cosmetic results, placing the skin-incision in the infra-mammary fold for women and periareoolar for men.
Study Limitations
This study has several limitations. This is a single center retrospective study and therefore distortion in patient selection and the technique used is inevitable. In addition, this work covers all of our initial “learning curves”. It is a not randomized comparison (endoscopy vs mininvasive standard), and the lack of long-term follow up, are another two important limitations. However, the study confirms that the endoscopic approach is as safe and effective as the standard minitoracotomy.
20
Table 1: Summary data for demographic variables
3rd 4th p.overall
N=205 N=107
Sex: <0.001
Female 43 (21.4%) 54 (50.5%)
Male 158 (78.6%) 53 (49.5%)
Mitral Procedure Complexity: 1.000
No 146 (71.2%) 76 (71.0%)
Yes 59 (28.8%) 31 (29.0%)
CPB 146 (30.9) 142 (30.2) 0.314
Aortic Cross Clamping 93.3 (22.4) 90.4 (23.8) 0.307
Intervention Time 246 (50.5) 226 (143) 0.163 Weight 177 (714) 118 (494) 0.397 Height 178 (118) 169 (9.45) 0.322 Approach: <0.001 Areolare 155 (75.6%) 45 (42.1%) Axillary 4 (1.95%) 2 (1.87%) Mini 46 (22.4%) 60 (56.1%) Titanium Fasteners: 0.004 No 16 (7.80%) 21 (19.6%) Yes 189 (92.2%) 86 (80.4%) MVP: 0.089 repair 187 (91.2%) 90 (84.1%) replacement 18 (8.78%) 17 (15.9%) Conversion To Minithoracotomy: 0.084 No 199 (97.1%) 99 (92.5%) Yes 6 (2.93%) 8 (7.48%) Preparing Surgeon: 0.255 Surgeon 1 159 (77.6%) 88 (82.2%) Surgeon 2 35 (17.1%) 11 (10.3%) Surgeon 3 10 (4.88%) 8 (7.48%) Surgeon 4 1 (0.49%) 0 (0.00%) 3D Endoscopy: 0.994 2D 192 (93.7%) 101 (94.4%) 3D 13 (6.34%) 6 (5.61%)
21
Table 2: Mitral Repair Complexity variables.
Third Forth
Female Male p.overall Female Male p.overall
N=43 N=158 N=54 N=53 Annuloplasty: 0.116 0.310 No 6 (14.0%) 10 (6.33%) 11 (20.4%) 6 (11.3%) Yes 37 (86.0%) 148 (93.7%) 43 (79.6%) 47 (88.7%) Neochorde: 0.009 0.003 No 23 (53.5%) 48 (30.4%) 37 (68.5%) 20 (37.7%) Yes 20 (46.5%) 110 (69.6%) 17 (31.5%) 33 (62.3%) Alfieri: 1.000 0.495 No 42 (97.7%) 155 (98.1%) 54 (100%) 52 (98.1%) Yes 1 (2.33%) 3 (1.90%) 0 (0.00%) 1 (1.89%) Sliding: 0.580 0.363 No 43 (100%) 154 (97.5%) 53 (98.1%) 50 (94.3%) Yes 0 (0.00%) 4 (2.53%) 1 (1.85%) 3 (5.66%) Scallop closure: 1.000 0.964 No 34 (79.1%) 127 (80.4%) 45 (83.3%) 43 (81.1%) Yes 9 (20.9%) 31 (19.6%) 9 (16.7%) 10 (18.9%) Leaflet resection: 0.009 1.000 No 43 (100%) 138 (87.3%) 50 (92.6%) 49 (92.5%) Yes 0 (0.00%) 20 (12.7%) 4 (7.41%) 4 (7.55%) MV Procedure Complexity: 0.842 1.000 Simple 30 (69.8%) 115 (72.8%) 38 (70.4%) 38 (71.7%) Complex 13 (30.2%) 43 (27.2%) 16 (29.6%) 15 (28.3%)
Mitral Valve Procedure: 0.116 0.310
repair 37 (86.0%) 148 (93.7%) 43 (79.6%) 47 (88.7%)
22
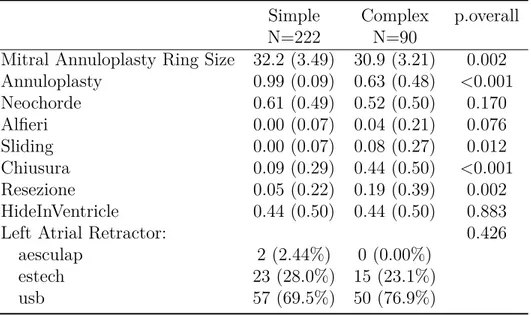
Table 3: Mitral procedure detals by its complexity
Simple Complex p.overall
N=222 N=90
Mitral Annuloplasty Ring Size 32.2 (3.49) 30.9 (3.21) 0.002 Annuloplasty 0.99 (0.09) 0.63 (0.48) <0.001 Neochorde 0.61 (0.49) 0.52 (0.50) 0.170 Alfieri 0.00 (0.07) 0.04 (0.21) 0.076 Sliding 0.00 (0.07) 0.08 (0.27) 0.012 Chiusura 0.09 (0.29) 0.44 (0.50) <0.001 Resezione 0.05 (0.22) 0.19 (0.39) 0.002 HideInVentricle 0.44 (0.50) 0.44 (0.50) 0.883
Left Atrial Retractor: 0.426
aesculap 2 (2.44%) 0 (0.00%)
estech 23 (28.0%) 15 (23.1%)
23
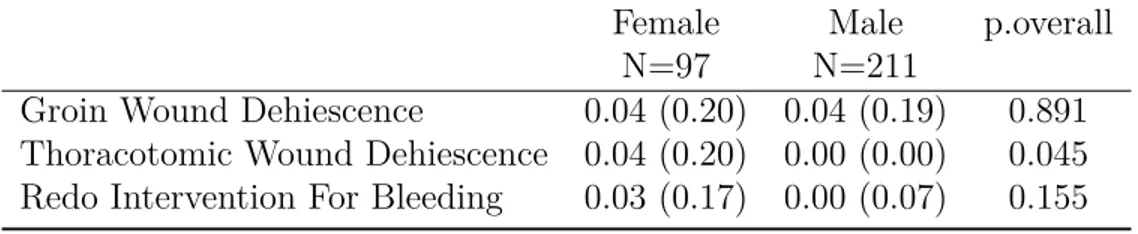
Table 4: Post porocedural complications
Female Male p.overall
N=97 N=211
Groin Wound Dehiescence 0.04 (0.20) 0.04 (0.19) 0.891 Thoracotomic Wound Dehiescence 0.04 (0.20) 0.00 (0.00) 0.045 Redo Intervention For Bleeding 0.03 (0.17) 0.00 (0.07) 0.155
26 Wilcoxon, p = 0.07 Wilcoxon, p = 0.28 Female Male 2D 3D 2D 3D 100 200 ThreeD CPB
Figure 4: Cardiopolmonary bypass time differences in defferent in-tercistal space approach.
27
Wilcoxon, p = 0.96 Wilcoxon, p = 0.38
Female Male
Third Forth Third Forth
50 100 150
Intercostal Space
XC
Figure 5: Cardiopolmonary bypass time differences in defferent in-tercistal space approach.
28
+ +
+
++
+
++
+++ + + + +
+++++
+
++++++
++
+++++
+++++++++ +
+ +
+ +
0.00 0.25 0.50 0.75 1.00 0 10 20 30 40Months
Sur
viv
al probability
Strata+
All 309 114 13 2 0 All 0 10 20 30 40Months
Str
ata
Number at risk
Conclusion
Endoscopic mitral valve surgery is safe, reproducible and has results excellent potential to become standard of care. It is comparable with minimally invasive mitral valve standard procedures. CPB times and aortic clamping are part of the learning curve but did not affect the mortality or affect premature mortality. With this approach we have been able to demonstrate that patients recover early and the discharge rate at their home is higher.
References
Bianchi, G., Margaryan, R., Kallushi, E., Cerillo, A. G., Farneti, P. A., Pucci, A., & Solinas, M. (2019). Outcomes of Video-assisted Minimally Invasive Cardiac Myxoma Resection. Heart, Lung and Circulation, 28 (2), 327–333. http://doi. org/10.1016/j.hlc.2017.11.010
Borger, M. A., Kaeding, A. F., Seeburger, J., Melnitchouk, S., Hoebartner, M., Winkfein, M., . . . Mohr, F. W. (2014). Minimally invasive mitral valve repair in Barlow’s disease: Early and long-term results. The Journal of Thoracic and Cardiovascular Surgery, 148 (4), 1379–1385. http://doi.org/10.1016/j.jtcvs.
2013.11.030
Cao, C., Harris, C., Croce, B., & Cao, C. (2017). Robotic mitral valve surgery. Annals of Cardiothoracic Surgery, 6 (1), 73. http://doi.org/10.21037/acs.2017.01.04 Cheng, D. C. H., Martin, J., Lal, A., Diegeler, A., Folliguet, T. A., Nifong, L. W., . . . Falk, V. (2011). Minimally invasive versus conventional open mitral valve surgery: A meta-analysis and systematic review. Innovations (Philadelphia, Pa.), 6 (2), 84–103. http://doi.org/10.1097/IMI.0b013e3182167feb
Chitwood, W. R. (2016). Robotic mitral valve surgery: Overview, methodology, results, and perspective. Annals of Cardiothoracic Surgery, 5 (6), 544–555. http: //doi.org/10.21037/acs.2016.03.16
32 References
Daemen, J. H. T., Heuts, S., Olsthoorn, J. R., Maessen, J. G., & Sardari Nia, P. (2018). Right minithoracotomy versus median sternotomy for reoperative mitral valve surgery: A systematic review and meta-analysis of observational studies. European Journal of Cardio-Thoracic Surgery: Official Journal of the European Association for Cardio-Thoracic Surgery, 54 (5), 817–825. http://doi.org/10.
1093/ejcts/ezy173
Glauber, M., Miceli, A., Canarutto, D., Lio, A., Murzi, M., Gilmanov, D., . . . Solinas, M. (2015). Early and long-term outcomes of minimally invasive mitral valve surgery through right minithoracotomy: A 10-year experience in 1604 patients. Journal of Cardiothoracic Surgery, 10 (1), 181.
http://doi.org/10.1186/s13019-015-0390-y
Mkalaluh, S., Szczechowicz, M., Dib, B., Sabashnikov, A., Szabo, G., Karck, M., & Weymann, A. (2018). Early and long-term results of minimally invasive mitral valve surgery through a right mini-thoracotomy approach: A retrospective propensity-score matched analysis. PeerJ, 6, e4810. http://doi.org/10.7717/peerj.4810 Modi, P., Hassan, A., & Chitwood, W. R. (2008). Minimally invasive mitral valve
surgery: A systematic review and meta-analysis. European Journal of Cardio-Thoracic Surgery: Official Journal of the European Association for Cardio-Cardio-Thoracic
Surgery, 34 (5), 943–952. http://doi.org/10.1016/j.ejcts.2008.07.057 Poffo, R., Montanhesi, P. K., Toschi, A. P., Pope, R. B., & Mokross, C. A. (2018).
Periareolar Access for Minimally Invasive Cardiac Surgery: The Brazilian Technique. Innovations (Philadelphia, Pa.), 13 (1), 65–69. http://doi.org/10.1097/IMI. 0000000000000454
Svensson, L. G., Atik, F. A., Cosgrove, D. M., Blackstone, E. H., Rajeswaran, J., Krishnaswamy, G., . . . Lytle, B. W. (2010). Minimally invasive versus conventional
References 33
mitral valve surgery: A propensity-matched comparison. The Journal of Thoracic and Cardiovascular Surgery, 139 (4), 926–932.e1–2. http://doi.org/10.1016/j.
jtcvs.2009.09.038
Vollroth, M., Seeburger, J., Garbade, J., Borger, M. A., Misfeld, M., & Mohr, F. W. (2013). Conversion rate and contraindications for minimally invasive mitral valve
surgery. Annals of Cardiothoracic Surgery, 2 (6), 853–854. http://doi.org/10. 3978/j.issn.2225-319X.2013.10.15
Walcot, N., Hohenberger, W., Lakew, F., Batz, G., Diegeler, A., & Perier, P. (2015). Totally endoscopic set-up for mitral valve repair. Multimedia Manual of Cardiotho-racic Surgery: MMCTS, 2015. http://doi.org/10.1093/mmcts/mmv016